Thoracic spondylitis induced myelopathy combined with herpetic neuralgia
Article information
Herpetic neuralgia is a significant source of morbidity following reactivation of dormant varicella zoster virus in dorsal root ganglia. Although majorities are uncomplicated, motor neuropathy may develop [1] and it can cause a diagnostic confusion with spondylitis, disc herniation, or spinal tumor. This case emphasizes the importance of careful history, clinical examination, laboratory markers and neuroimaging for diagnosis in patient with uncertain back pain.
A 75-year-old, 178 cm, 79 kg male patient was referred to our pain clinic with lower back and left buttock pain (L5 to S1 dermatome). He had history of two attacks of herpes zoster at the same site for 5 years and complete recovery with antiviral agent. Two weeks prior, he had undergone appendectomy. After the surgery, pneumonia was developed and treated with antibiotics. A few days later, painful vesicules had developed on left buttock and clinical evaluation by dermatologist confirmed acute herpes zoster. The vesicules resolved with antiviral agent. However, the buttock pain was sustained. In initial examination, herpetic scars were present at left buttock. He suffered from continuous lancinating pain (8 points on a 0 to 10 verbal rating scale; VRS, 0 = no pain, 10 = worst pain imaginable). He felt radicular numbness and tingling on the left leg. The motor strength was normal over both legs and sensation was mildly diminished along the left buttock and lateral upper thigh. The pain was not aggravated by position, and straight leg raise test was normal. There was no percussion tenderness in lower back and left buttock. Vital signs were stable and all laboratory findings were unremarkable, with the exception of erythrocyte sedimentation rate (ESR) level of 23 mm/hr. A diagnosis of recurrent herpes zoster with radiculopathy was made, and he was treated with gabapentin, opioids, tricyclic antidepressants, and caudal block with epidural catheter on the left L5 to S1 root with 0.75% ropivacaine 2 ml and triamcinolone 40 mg, which was diluted in normal saline to 5 ml. On the second visit after seven days, the buttock pain had mildly subsided (5 VRS). However, left thoracolumbar pain was developed (7 VRS). On the examination, vital signs were stable and there were no new vesicules, only herpetic scars at the left buttock, and the pain was a continuous lancinating pattern. There was no percussion tenderness on thoracolumbar area and no change in motor strength and sensation. With our suspecting prodromal herpetic pain on left thoracolumbar area, he underwent caudal block with conventional medication, adding acyclovir 800 mg in a day. On the third visit after four days, he complained of heavy back pain and progressive weakness in both legs. He also presented sensory disturbances in both legs. Vital signs were stable without fever. Straight leg raise test was not able to do due to severe back pain. A neurologic examination revealed 3/5 strength of the left L2 hip flexor and L3 knee extensor, and 3/5 strength of the right L2 hip flexor, and 2/5 strength of the right L3 knee extensor. Sensory abnormality was below T11 dermatome. An immediate magnetic resonance imaging (MRI) of the spine demonstrated necrotic spondylitis at T9 to T10 levels with compressive myelopathy (Fig. 1). Emergent laminectomy was undertaken and antibiotic therapy was done. At surgical field, there was no visible abscess but vertebral body granulation tissue. The specimens demonstrated only non-specific inflammation. It was tested for gram staining and culture, and all results showed negative. After the surgery, the leg weakness showed gradual improvement, and back pain was significantly improved (2 VRS). Eight weeks later, he was discharged with conservative treatment and bracing.
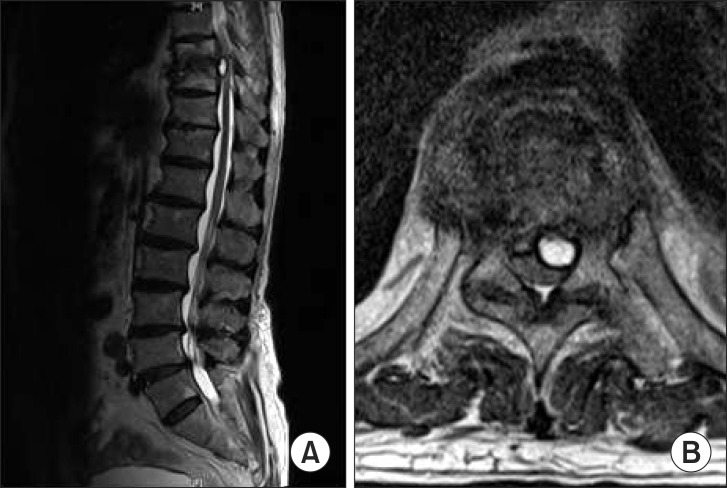
This figure shows the sagittal and axial magnetic resonance images of the thoracolumbar spine. The T2-weighted sagittal view image (A) demonstrates necrotic spondylitis causing myelopathy in T9 to T10 levels. The T2-weighted axial view image (B) demonstrates the fluid content to the left, which compress spinal cord.
Spondylitic myelopathy may occur due to cord compression from epidural granulation tissue or abscess. It presents with back pain, progressive radiculopathy or myelopathy, and sensory deficit with or without fever [2]. This various symptoms commonly make diagnostic delay, range from 2 to 12 weeks [3]. Predisposing factors are the advancing age, malnutrition, immunodeficiency, diabetes mellitus, and septicemia [4].
Zoster myelopathy presents with focal weakness and sensory impairment after varicella zoster infection. Weakness usually develops within 2 to 3 weeks of vesicular eruptions, but varies from hours to month. Because varicella zoster infection is treatable disease requiring timely diagnosis and management, it is to be ruled out in suspicion of myelopathy.
In our case, the initial symptoms were indistinguishable from radiculopathic zoster neuralgia to spondylitic myelopathy, leading to the diagnostic delay. Herpes zoster is diagnosed clinically by a prodrome of 1-3 days, unilateral pain, grouped vesicules, and rash history in the same distribution. In the study by Yawn et al. [5], the incidence of zoster recurrence showed higher rates of 1.7 to 4.4% in immunocompetent individuals over 60 years. Our patient had a zoster history and recent episode of zoster vesicules at the same dermatome, and typical zoster pain pattern. So, we diagnosed the pain only as a recurrent herpes zoster with radiculopathy and prodromal zoster pain possibility at thoracolumbar area and did not exclude spondylitis until he showed motor weakness. In case of varicella-zoster virus (VZV) reactivation without rash, there are laboratory modalities for virological confirmation, such as VZV DNA in saliva, VZV DNA and anti-VZV antibody in blood and CSF [1]. But we could not lumbar puncture due to the concern for the dissemination of possible infection. After MRI evaluation, it was finally diagnosed as a compressive myelopathy by necrotic spondylitis, combined with acute herpetic neuralgia. We can assume that this spondylitis was caused by previous pneumonia organism or immunocompromised induced bacterial infection. At surgical field, we could not find obvious focus of infection, and culture results were negative. The antibiotics after appendectomy and pneumonia may have compromised the negative infection signs and culture results.
In conclusion, physicians should know the signs and possible causes of back pain with myelopathy and take care for early accurate diagnosis to improve outcome. When patients present sustained pain with an episode of zoster infection, even though it has a strong possibility of herpetic neuralgia, we must exclude other conditions causing radiculopathy in the affected dermatome.