Occurrence of a spinal intradural arachnoid cyst after epiduroscopic neural decompression
Article information
Epiduroscopy is a relatively new technique that enables visualization of structures directly within the epidural space to detect pathology, improve adhesion, and to administer local anesthetics and steroids to affected nerve roots [1,2]. However, several complications such as visual impairment, epidural abscess, and encephalopathy with rhabdomyolysis have been reported. We report a case of a symptomatic spinal intradural arachnoid cyst induced by an accidental dural tear during epiduroscopy in a patient with failed back surgery syndrome (FBSS).
A 65-year-old woman presented with chronic low back pain and radiating leg pain. She complained of hip and thigh pain, and claudication improved with rest. She had undergone a discectomy and laminectomy twice at L4, L5, and S1 2 years ago. On examination, the straight leg raising test was positive bilaterally. The Patrick test was negative, and no vascular abnormalities were observed. Magnetic resonance imaging (MRI) revealed an epidural adhesion with postoperative changes, degenerative changes of the L4-5 disc, and a laminectomy state at L5 and S1. A variety of pain therapies were ineffective. Her illness was diagnosed as FBSS, and our plan was epiduroscopic neural decompression.
She was placed in the prone position with routine monitoring in the operating room. An 18.5-G Tuohy needle was introduced into the epidural space through the sacral hiatus under aseptic conditions and with local anesthesia. An introducer sheath was advanced into the sacral epidural space. A 0.9 mm flexible endoscope (3000E, Myelotec, Roswell, GA, USA), covered with a 2.9 mm steering catheter (2000, Myelotec), was introduced through the sheath and advanced cephalad into the epidural space under fluoroscopic guidance. Adhesions in the epidural space were mobilized with the tip of the instrument under careful direct vision. However, sufficient epidural adhesiolysis could not be achieved above the S1 level due to the dense adhesions and scar tissue. Epidural fat and scars were visualized, but the image was fuzzy. Further adhesiolysis was attempted. Despite slow advancement of the endoscope, there was a sudden loss of resistance at the level of L5-S1. The S1 nerve roots appeared with small blood vessels, but they were unclear.
Iohexol contrast (IOBRIX 300®, 640 mg/ml, Accuzen) instillation under fluoroscopy demonstrated a myelogram, which confirmed that the endoscope had entered the subarachnoid space. The endoscope was retracted from the hole in the dura, and a catheter was placed into the ventrolateral aspect of the left L5-S1 intervertebral foramen under fluoroscopy via the epiduroscope working channel. Contrast agent administration revealed good ventrolateral epidural spread along the L5 nerve roots without connection to the subarachnoid space after negative aspiration of cerebrospinal fluid and blood. A test dose of 2 ml 0.4% lidocaine with 5 mg triamcinolone was injected. The patient had no adverse hemodynamic or neurologic sequelae. Thirty ml of 0.4% lidocaine and 30 mg of triamcinolone were injected into the epidural space at the end of the epiduroscopy. The total volume of saline used for epidural irrigation was 200 ml. The operation was terminated after 40 min due to her frequent complaints of low back pain and movement during the procedure. No complications developed, and the patient was stable. Thus, we did not take action such as an epidural blood patch. She only complained of mild low back pain after 3 hours.
However, she complained of bursting pain on the left hip and leg after 4 days. The numeric rating score (NRS) was 7-8/10. We performed a transforaminal epidural block of the left L5 and S1 dermatome, and the patient was prescribed 1,200 mg/day gabapentin for pain control. She visited again after 2 weeks and complained of pain at the left hip, leg, and pelvic area. The transforaminal epidural block had no effect, and the symptoms had not improved after 4 weeks. A lumbar spinal MRI was rechecked. The MRI revealed an intradural arachnoid cyst with a longitudinal length of 8 cm that spanned from the midbody of L4 to the S2 level (Fig. 1). Computed tomography (CT) showed an arachnoid cyst that was connected with the thecal sac below the upper margin of S1. She underwent a partial cystectomy with dural repair and a microdiscectomy at L5-S1. Symptoms improved after 4 weeks, and the NRS decreased to 3-4/10.
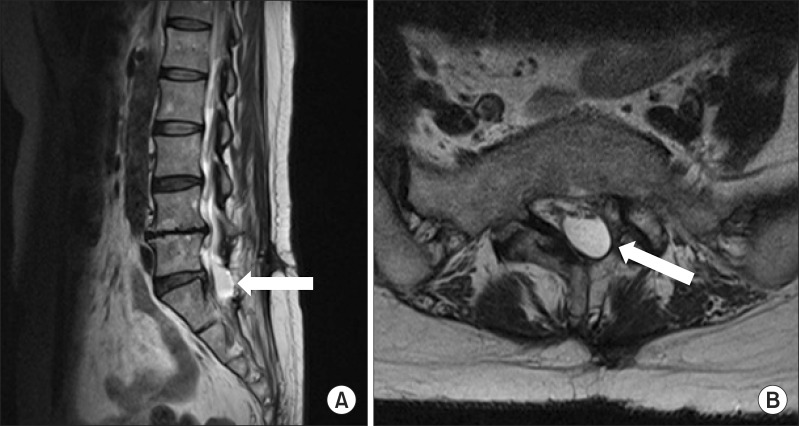
Magnetic resonance imaging T2 sagittal image (A) shows high signal intensity cystic lesion (white arrow) at L5-S1. In axial image (B), arachnoid cyst (white arrow) is herniated to the laminectomy site at L5-S1.
Complications can occur during epiduroscopy even in experienced hands. Furthermore, surgery may alter the anatomy of the epidural space and increase the risk of inserting devices in the wrong location. Iatrogenic spinal arachnoid cysts are rare. A dural injury itself dose not become a complication unless the accidental perforation is not recognized and is not responded to, for instance, by applying local anesthetics.
Intradural spinal arachnoid cysts are usually asymptomatic. They are found incidentally on MRI imaging and usually do not require any specific treatment. The etiology of a spinal arachoid cyst is uncertain. Clinical manifestations of arachnoid cysts include progressive back pain, which is worse at night or when recumbent, gait difficulties, spastic or flaccid paralysis, radiculopathy, and worsening of symptoms with a Valsalva maneuver. MRI is the preferred imaging modality to determine the presence and extent of an arachnoid cyst after plain radiography to exclude bony abnormalities. CT myelography can be used for patients in whom MRI is contraindicated and may provide additional information about cyst architecture and any fluid communication that may exist. Surgical intervention is the most effective treatment when imaging confirms the presence of a spinal arachnoid cyst, and the cyst is the main cause of a patient's symptoms. Complete resection is the preferred method, but drainage by fenestration may be used in cases where location or vigorous adherence to the cord prevents resection [3].
Complications associated with epiduroscopy should not be overlooked, and obtaining a clear visual field is essential for safe mechanical adhesiolysis. The epiduroscope should not be advanced blindly or with brute force to achieve the target epidural position. Using proper epiduroscopic equipment as well as acquiring sufficient experience with the epiduroscopic technique can prevent complications.
We overlooked the clinical manifestations of this patient and possible side effects, and a timely evaluation was not performed. Thus, close observation and continuous assessment after the procedure and prompt management of a complication are always required.