A comparison of hemodynamic changes after endotracheal intubation by the Optiscope™ and the conventional laryngoscope
Article information
Abstract
Background
Optiscope™ is a newly developed video stylet device. This study evaluated and compared the hemodynamic changes observed after endotracheal intubation with video stylet and after conventional laryngoscopic endotracheal intubation.
Methods
Fifty-eight adult patients with American Society of Anesthesiologists (ASA) physical status class 1 or 2, undergoing general anesthesia, were randomized into two groups: one group of patients were intubated using video stylet (n = 29) and the other group were intubated using direct laryngoscope (n = 29). Systolic blood pressure (SBP), mean arterial pressure (MAP), diastolic blood pressure (DBP), heart rate (HR), POGO (percentage of glottic opening) score, time for intubation and degree of sore throat were recorded.
Results
There were no significant differences in the SBP, MAP, DBP, HR, and the sore throat incidence between the two groups. Optiscope™ produced better POGO scores, but time for intubation was longer than with conventional laryngoscope.
Conclusions
Optiscope™, when compared with conventional laryngoscope for intubation, does not modify the hemodynamic response, but it provides a better view of the vocal cords.
Introduction
Endotracheal intubation is an essential manipulation in respiratory failure or general anesthesia, but the resulting hemodynamic response and complications can cause serious problems for the patient. The force applied by the laryngoscope during endotracheal intubation and the irritation caused when the tube enters the trachea, expansion of the cuff, and pressure on the ring cartilage, among other factors, can stimulate the autonomic nervous system, resulting in hemodynamic changes in the patient, and can also cause cerebral hemorrhage or aneurysm rupture in patients with cerebrovascular disease [1,2].
Of the types of irritation that can occur during endotracheal intubation, irritation from the laryngoscope and irritation from the tube entering the trachea have the greatest effect on hemodynamic changes. When lifting a larynx with a laryngoscope, a force of approximately 40 N is applied to the pharynx and larynx [3], and research using a lightwand or optical bronchoscope in endotracheal intubation to reduce hemodynamic changes through reducing irritation has shown varying results [4-8].
New instruments have been developed for safe and accurate endotracheal intubation, and with the development of electronic and optical technology, current instruments are made so endotracheal intubation is performed while viewing the larynx with video assistance. Optiscope™ PM 201 (Clarus Medical, Minneapolis, MN, USA) is a semi-rigid fiberoscope with two light sources and a 4-inch LCD monitor, so intubation can be performed while visualizing the patient's larynx through the monitor (Fig. 1). The angle of the tip can be adjusted for each patient, and blind endotracheal intubation can be performed as with a lightwand, using the red light source. Endotracheal intubation is possible using the Optiscope™ alone or together with the laryngoscope.
Unlike the lightwand, the Optiscope™ can provide accurate images during endotracheal intubation, and in contrast to existing optical bronchoscopes, with which the image has to be seen directly or by connecting a cable to a monitor, images can be seen through the monitor fixed to the handle, allowing a more comfortable posture during intubation and making it easier to operate.
The authors hypothesized that when endotracheal intubation is performed with Optiscope™, there will be no irritation on the pharynx and larynx from the laryngoscope blade, so fewer hemodynamic changes will be produced than when endotracheal intubation is performed with a laryngoscope, and there will be a reduction in the degree of sore throat following surgery.
In this study, endotracheal intubation using the conventional laryngoscope (Macintosh Laryngoscope) and the Optiscope™ were compared to see if there were any differences in hemodynamic changes and sore throat in the patients. The success rate of the first attempt, visibility of the larynx, and time taken for intubation were also investigated to determine if there were any differences.
Materials and Methods
This study was approved by the Institutional Review Board of our hospital. In accordance with the Declaration of Helsinki (2008), the purpose and method of the study were sufficiently explained to the patients, and the study was conducted after obtaining informed consent.
Study subjects were patients scheduled for surgery under general anesthesia who were age 20-65 and American Society of Anesthesiologists physical status class (ASA) 1 or 2.
Patients with hypertension, severe cardiovascular disease or lung disease, and those in whom difficulty in intubation could be anticipated, such as patients with BMI greater than 30, bad teeth, disorder in mouth opening or neck extension, and Mallampati score IV were excluded from the study. In the case of patients who had no history of hypertension but had systolic blood pressure over 140 mmHg in the operating room, their blood pressure was checked in the ward, and when there was suspicion of high blood pressure they were excluded from the study. When intubation was not successful on the first attempt, the Optiscope™ was used together with a laryngoscope for the reattempt, and the Macintosh laryngoscope was used together with a stylet in the reattempt. Cases in which intubation did not succeed on the first attempt were excluded from the study.
The subject patients were divided into two groups using randomly generated numbers from Excel, and the patients were not aware which group they were in. One group underwent endotracheal intubated using the Optiscope™ (group S), and in the other group, the Macintosh laryngoscope was used (group L).
One hour before inducing anesthesia, glycopyrrolate 0.2 mg was injected IM to the patient as premedication, and after entering the operating room, ECG, NIBP monitor, and pulse oximeter were applied to the patient. The Mallampati score was measured, and heart rate, systolic blood pressure, diastolic blood pressure, and mean arterial pressure were measured in the stable state, directly before inducing anesthesia. Fentanyl 2 mcg/kg was then injected IV, and thiopental 5 mg/kg and rocuronium 0.6 mg/kg were administered to induce anesthesia. Desflurane 6 vol% and O2 5 L/min were inhaled through a face mask, and 2 minutes later endotracheal intubation was attempted. After intubation, anesthesia was maintained with desflurane 6 vol%, N2O 1.5 L/min, and O2 1.5 L/min. An 8.0 mm tube was used for males and a 7.0 mm tube used for females during the endotracheal intubation. All intubations were performed by a single anesthesiologist with more than 2 years' experience who had performed endotracheal intubation with the Optiscope™ more than 30 times.
When using the Optiscope™, intubation was performed through the midline approach. The appropriate endotracheal tube based on the sex of the patient was inserted over the probe. After extending the patient's neck, an access route was obtained by opening the mouth with the left hand and lifting while holding the patient's tongue and lower jaw. Directions for using the Optiscope™ are as follows: Holding the Optiscope™ with the right hand, enter following the center of the palate keeping the end of the stylet perpendicular to the patient's mouth. Here, adjust the angle of the monitor screen with the right thumb to the angle of the stylet for better visibility. When entry is continued while watching the screen, the epiglottis and glottis become visible. When the end of the probe enters the vocal cords, push the endotracheal tube in to the desired depth. Holding the tube with the left hand and checking the screen, smoothly extricate at the set angle in the opposite order of entry.
After the patient arrived in the operating room in a stable state, before anesthesia was induced, the blood pressure and heart rate were measured for the study baseline, and systolic blood pressure, mean arterial pressure, diastolic blood pressure, and heart rate were measured 1, 3, and 5 minutes after endotracheal intubation. The time taken for intubation was measured by another observer, starting when the laryngoscope or Optiscope™ passed the front teeth in the lower jaw in entrance and ending when the instrument passed the front teeth in the lower jaw in extrication. POGO score (Percentage of Glottic Opening) is an expression describing as a percentage the degree of visibility of the glottis after insertion of the laryngoscope. It is considered to be 100% when the entire glottis is visible and 0% when the glottis is not visible at all, and the performing anesthesiologist in this study recorded the score under subjective judgment [9]. 24 hours after surgery, sore throat was evaluated as none, mild, moderate, or severe.
The primary outcome was the systolic blood pressure after endotracheal intubation. To estimate the group size, a pilot study was conducted which measured the systolic blood pressure after endotracheal intubation of 10 patients who had undergone endotracheal intubation using the Macintosh laryngoscope. In this group the standard deviation in systolic blood pressure was 13 mmHg. Hypothesizing that the standard deviation would be equal in the group that underwent endotracheal intubation using the Optiscope™, to sort out a difference of systolic blood pressure of 10 mmHg, results of calculating with α error as 5% and β error as 20% revealed that the number of subjects needed in each group was 27. Hypothesizing that the possibility of intubation failure was 10%, the study was conducted with 30 patients in each group.
In continuous data, the normal distribution of the collected data was verified through the Shapiro-Wilk test.
The normally distributed data is presented here as the mean ± standard deviation and the groups were compared using Student's t test. The non-normally distributed data is expressed as medians (25 quartile-75 quartile) and this data was analyzed using the Mann-Whitney u test.
In the case of categorical data, a chi-squared analysis or Fisher's exact test was performed.
The heart rate and blood pressure of each group were analyzed using two-way repeated measures of ANOVA. Results were considered to be statistically significant when the P value was 0.05 or less. Data in the figure were expressed as mean and standard error. Statistical analysis was performed using SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
Results
The study began with 30 patients in group S and 30 patients in group L, but each group had 1 patient with failed intubation on the first attempt, so excluding these patients, 29 patients in each group were included in the study. There were no statistically significant differences in sex, age, weight, height, BMI, ASA score, Mallampati score, and heart rate and blood pressure before anesthesia between the two groups (Table 1).
There were no statistically significant differences observed between the two groups in systolic blood pressure, mean arterial pressure, diastolic blood pressure, and heart rate before anesthesia and 1, 3, and 5 minutes after endotracheal intubation. In both groups the systolic blood pressure and mean arterial pressure 1 minute after intubation were significantly higher than the blood pressure before anesthesia and gradually decreased, so that at 3 and 5 minutes after anesthesia the blood pressure was lower than before anesthesia (Fig. 2 and 3).
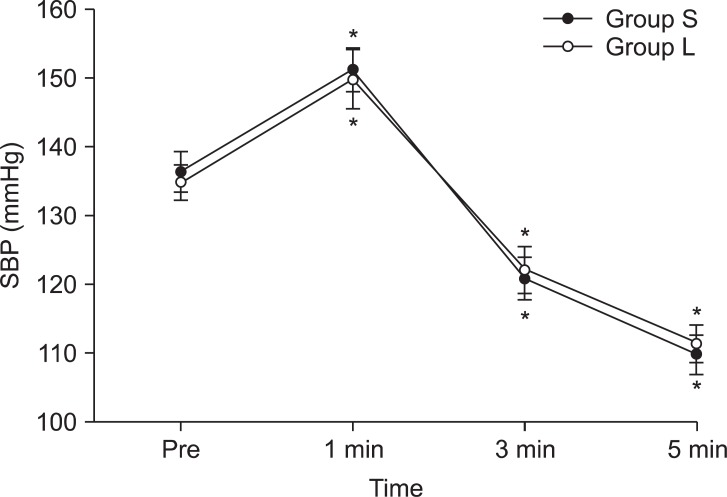
Changes of systolic blood pressure (SBP) before and after intubation (mean ± standard error). Group S: Optiscope using group, Group L: Machintosh laryngoscope using group. Pre: pre-induction value. 1, 3, 5 min: value at 1, 3, 5 minute after intubation. There no significant differences between two groups. *P < 0.05 compared to pre-induction value.
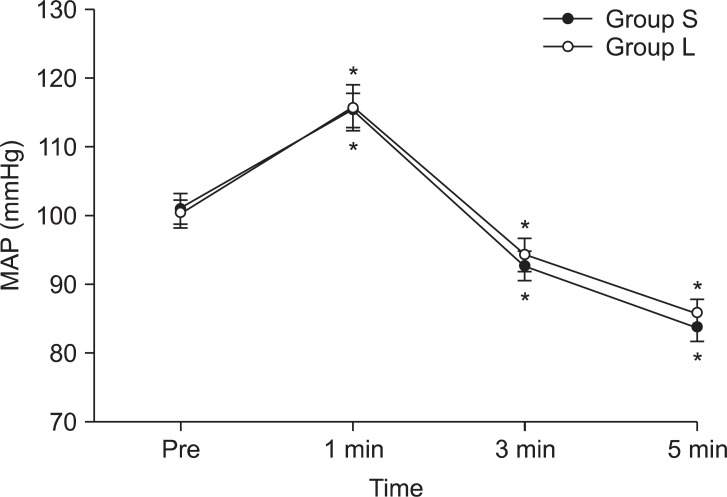
Changes of mean arterial pressure (MAP) before and after intubation (mean ± standard error). Group S: Optiscope using group, Group L: Machintosh laryngoscope using group. Pre: pre-induction value. 1, 3, 5 min: value at 1, 3, 5 minute after intubation. There no significant differences between two groups. *P < 0.05 compared to pre-induction value.
The diastolic blood pressure 1 minute after anesthesia in both groups was higher than the blood pressure before anesthesia and gradually decreased, to have no statistically significant difference at 3 minutes and to be lower than before anesthesia at 5 minutes after anesthesia (Fig. 4).
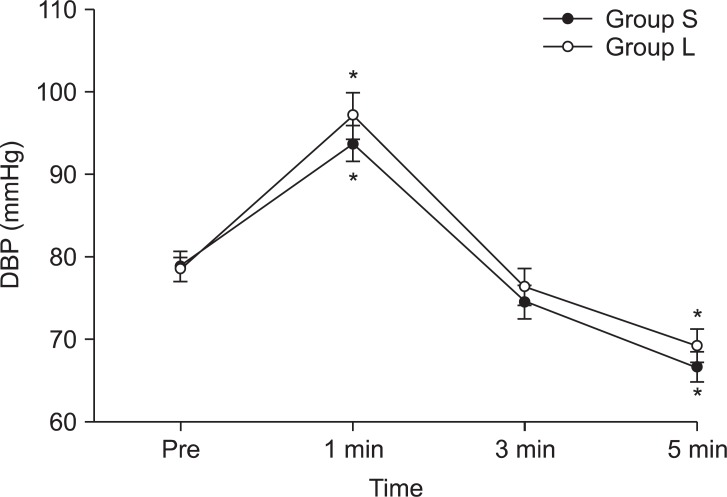
Changes of diatolic blood pressure (DBP) before and after intubation (mean ± standard error). Group S: Optiscope using group, Group L: Machintosh laryngoscope using group. Pre: pre-induction value. 1, 3, 5 min: value at 1, 3, 5 minute after intubation. There no significant differences between two groups. *P < 0.05 compared to pre-induction value.
In both groups the heart rate 1 minute after anesthesia had increased compared to the heart rate before anesthesia, and although it gradually decreased, the heart rate at 3 and 5 minutes after anesthesia was still significantly higher than the heart rate before anesthesia (Fig. 5).
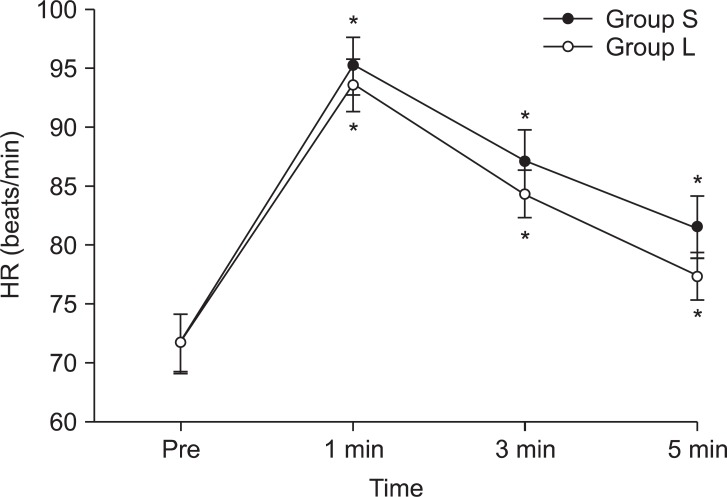
Changes of heart rate (HR) before and after intubation (mean ± standard error). Group S: Optiscope using group, Group L: Machintosh laryngoscope using group. Pre: pre-induction value. 1, 3, 5 min: value at 1, 3, 5 minute after intubation. There no significant differences between two groups. *P < 0.05 compared to pre-induction value.
Success rate of the first intubation attempt was equal in both groups, at 96.7%. The time taken for intubation was significantly longer in group S, at 20.5 seconds (16.75-28.5), compared to group L, at 16.0 seconds (14.75-20.0) (P < 0.01). POGO score was significantly higher in group S (100%) than in group L (65.8%) (P < 0.01). There was no statistically significant difference in sore throat 24 hours after surgery between the groups (Table 1).
None of the patients developed severe bradycardia (heart rate ≤ 45 beats/min) or severe low blood pressure (systolic blood pressure ≤ 60 mmHg) during the study, and oxygen saturation did not fall below 98%. In the 2 patients who were excluded from the study for failing the first intubation attempt, the second attempt was successful in both patients and there were no complications.
Discussion
This study aimed to compare the hemodynamic changes that occurred using the Optiscope™, which is a semi-rigid fiberoscope, and the Macintosh laryngoscope in endotracheal intubation. It was expected that the hemodynamic changes would be smaller with the Optiscope™ compared to the conventional laryngoscope, since accurate intubation is possible through video images and there is no irritation from the laryngoscope blade. Previous studies have reported noticeable increases in blood pressure and blood concentration of catecholamines from just the operation of the laryngoscope, without endotracheal intubation [2], and in a study that compared the lightwand and laryngoscope in endotracheal intubation, it was reported that there were no differences in blood pressure in normal patients, but in patients with hypertension the use of the lightwand in intubation resulted in a smaller increase in blood pressure than that in the group in which the laryngoscope was used [7]. In addition, in a study that used another type of bronchoscope, the Styletscope™, it was reported that there was a smaller increase in heart rate in the group in which the Styletscope™ was used, compared to the group that underwent endotracheal intubation using a laryngoscope [6]. However, in our study, there was no statistically significant difference between group S, in which the Optiscope™ was used, and group L, in which the laryngoscope was used, in blood pressure and heart rate 1, 3, and 5 minutes after endotracheal intubation.
The reason that intubation with the Optiscope™ resulted in similar hemodynamic changes to the laryngoscope, despite no lifting irritation from the laryngoscope, could be, first, that the irritation caused by the tube passing through the vocal cords has a larger effect on blood pressure and heart rate than that caused by the laryngoscope. In previous studies, there were larger hemodynamic changes when endotracheal intubation and laryngoscopy were performed together than when just lifting with the laryngoscope, and it was reported that this was due to the larger effect of irritation on the respiratory tract from the tube than irritation from the laryngoscope [5]. Second, it is possible that lifting the tongue and jaw together when using the Optiscope™ can have a similar effect on heart rate and blood pressure to that of irritation from the laryngoscope. In a previous study comparing the lightwand and laryngoscope, it appeared that there was no difference in the effect on blood pressure and heart rate, and a study comparing the Bonfils intubation fiberoscope or Levitan FPS, which are optical bronchoscopes, with the laryngoscope also showed no difference in the effect on blood pressure and heart rate. The reason for such results was reported to be that lifting the lower jaw for smooth passage of the endotracheal tube is sufficient stimulus to cause hemodynamic changes [5,8,10]. Third, this study was conducted on only patients with normal airways so the differences in hemodynamic changes between the groups could be smaller. More pressure from the laryngoscope is applied in endotracheal intubation in difficult airway, and hemodynamic changes due to the laryngoscope can be more noticeable in difficult airways [3]. Fourth, although the performing anesthesiologist had more than 2 years' experience in using the laryngoscope, the anesthesiologist had less experience in using the Optiscope™ despite the practice of more than 30 procedures, so this difference could have had an influence. In the case of the Bonfils rigid fiberoscope, which is similar to the Optiscope™, one study showed that the learning curve is about 20 cases in normal airways, and 50 cases in difficult airways [11].
The POGO score was higher in group S (100%) than in group L (65.8%), and it resulted in 100% in group S because the tube was inserted while directly observing the glottis. Patients who were anticipated to have difficult endotracheal intubation were excluded from the study, but if they had been included, the POGO score of group L would be expected to be much lower. When research that reports on the usefulness of optical bronchoscopes in difficult endotracheal intubation [12-14] is considered, the Optiscope™ is expected to be helpful in difficult endotracheal intubation as it provides better visibility of the glottis compared to the laryngoscope.
The first attempt of endotracheal intubation did not succeed in 1 patient from each group. In the patient from group L, the glottis was not visible at all after inserting the laryngoscope, so a stylet was used for intubation, and in the patient from group S, there were too many secretions, so after failing the first attempt the secretions were suctioned and the second attempt was successful.
When using an optical bronchoscope, if secretions cover the lens area, visibility deteriorates, which can disrupt the endotracheal intubation, so use of an antisialagogue as premedication is recommended [15]. Therefore when using the Optiscope™, it is considered to be helpful to use an antisialagogue as premedication.
This study has a few limitations. First, it was not a double-blind study, since the performing anesthesiologist was aware of which instrument to use. The fact that the performing anesthesiologist was aware of the type of instrument could have had an effect on the results of this study. Second, it was conducted on normal patients with no accompanying diseases. There could be different results for patients with hypertension, who can have larger hemodynamic changes in endotracheal intubation, or in patients who are expected to have difficult endotracheal intubation. Therefore the results of this study cannot be extended and applied to patients with accompanying diseases.
In conclusion, using the Optiscope™ in endotracheal intubation did not reduce hemodynamic changes, but showed similar hemodynamic changes to the laryngoscope, and success rate and sore throat following surgery also did not show large differences. In the future the Optiscope™ may be considered to be a method to replace the laryngoscope in endotracheal intubation.
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2012R1A1A1003700).

