Accuracy of cardiac output measurements during off-pump coronary artery bypass grafting: according to the vessel anastomosis sites
Article information
Abstract
Background
During beating heart surgery, the accuracy of cardiac output (CO) measurement techniques may be influenced by several factors. This study was conducted to analyze the clinical agreement among stat CO mode (SCO), continuous CO mode (CCO), arterial pressure waveform-based CO estimation (APCO), and transesophageal Doppler ultrasound technique (UCCO) according to the vessel anastomosis sites.
Methods
This study was prospectively performed in 25 patients who would be undergoing elective OPCAB. Hemodynamic variables were recorded at the following time points: during left anterior descending (LAD) anastomosis at 1 min and 5 min; during obtuse marginal (OM) anastomosis at 1 min and 5 min: and during right coronary artery (RCA) anastomosis at 1 min and 5 min. The variables measured including the SCO, CCO, APCO, and UCCO.
Results
CO measurement techniques showed different correlations according to vessel anastomosis site. However, the percent error observed was higher than the value of 30% postulated by the criteria of Critchley and Critchley during all study periods for all CO measurement techniques.
Conclusions
In the beating heart procedure, SCO, CCO and APCO showed different correlations according to the vessel anastomosis sites and did not agree with UCCO. CO values from the various measurement techniques should be interpreted with caution during OPCAB.
Introduction
Coronary artery bypass grafting (CABG) on the beating heart without the use of a pump oxygenator, has been offered as an alternative to the standard on-pump technique. Several clinical results have shown that off-pump CABG (OPCAB) is a safe and effective method in selected cases. OPCAB has great potential advantages compared to the standard on-pump technique, such as no activation of proteolytic and inflammatory systems, depression of the immune system, or consumption of clotting factors and platelets [1].
OPCAB may significantly disrupt circulatory homeostasis and challenge the anesthesiologist to preserve stable hemodynamics during the procedure. Beating heart surgery involves lifting, rotating, compressing, and placing pads under the heart to achieve adequate exposure to construct the anastomosis [2]. These maneuvers may result in major hemodynamic changes, necessitating adequate intraoperative monitoring. Accordingly, reliable monitoring tools are prerequisites for adequate hemodynamic management ; however, consensus about which techniques to use for this purpose has yet to be reached.
Several methods of continuous measurement of cardiac output (CO) are available, including computerized pulmonary arterial (PA) thermodilution such as the stat CO mode (SCO) and continuous CO mode (CCO), arterial pressure waveform-based CO estimation (APCO), and the transesophageal Doppler ultrasound technique (UCCO). During hemodynamically stable periods, many studies have shown good to excellent agreement among these methods [3-12]. However, during beating heart surgery, the accuracy of these measurement techniques may be influenced by several factors [8,13-17]. Tricuspid regurgitation and high quantities of infusate during direct manipulation and dislocation of the heart reduce the accuracy of variables measured via computerized PA thermodilution in beating heart surgery [18,19]. In addition, OPCAB patients had unique intraoperative periods (in particular, the period of coronary artery graft surgery), which is characterized by rapid changes in vascular volume and compliance. These factors can have a marked influence on APCO accuracy [16,20,21]. UCCO measurements give true pulse-wave signals from the descending aorta [22], and these factors do not influence UCCO accuracy. Nevertheless, the accuracy and precision of SCO, CCO and APCO estimations and their comparison with UCCO during beating heart surgery, especially during vessel anastomosis, have yet to be reported. Therefore, this study was conducted to analyze the clinical agreement among SCO, CCO, APCO, and UCCO during OPCAB.
Materials and Methods
Upon Institutional Review Board approval and patient's consent, this study was prospectively conducted on 25 patients who were scheduled to undergo elective OPCAB. Patients with dysrhythmia or a left ventricular ejection fraction ≤ 35%, any evidence of valvular heart disease (greater than grade 2), ventricular aneurysm, or emergent operation were excluded.
All patients were premedicated with intramuscular 0.1 mg/kg of morphine one hour before anesthesia. Five ECG leads were attached, and leads II and V5 with ST segment trend analysis were simultaneously monitored once patients arrived in the operating room. A 20-gauge catheter was inserted into the right radial artery for direct arterial pressure monitoring and blood gas analysis. A thermodilution pulmonary artery catheter (PAC: Swan-Ganz CCOmbo V Model 774HF75w: Edwards Lifesciences LLC, Irvine, CA, USA) was introduced through the right internal jugular vein. The CCOmbo V catheter was connected to the CCO/oxymetry/volumetric monitor (Vigilance Monitor: Edwards Lifesciences LLC, Irvine, CA, USA).
Following anesthesia induction using intravenous 2.0-3.0 mg midazolam, 0.5-1.0 µg/kg sufentanil, and 0.1 mg/kg vecuronium, the trachea was intubated. Anesthesia was maintained by the inhalation of medical oxygen-air-sevoflurane (< 0.5 MAC) and continuous sufentanil infusion. Mechanical ventilation was adjusted so that the carbon dioxide partial pressure in the arterial blood was maintained at 35-40 mmHg.
A radial arterial line was connected to FloTrac™ sensors (Edwards Lifesciences LLC, Irvine, CA, USA), after which the CO was determined using the algorithm provided in the commercially available Vigileo™ APCO system (Edwards Lifesciences LLC; software version 3.0). An esophageal Doppler probe (Hemosonic; Arrows International, Everett, MA, USA) was inserted orally and advanced into the esophagus to approximately the sixth thoracic vertebra to measure the UCCO. The depth of the probe insertion in each patient was selected to obtain the best signal quality; therefore, the position may have varied between patients. The echo signal was adjusted to the maximum signal height and the probe was positioned until both the anterior and the posterior wall of the aorta were visible on the screen. The echo probe was readjusted if loss of the aortic wall was detected by M-mode ultrasound.
Intravenous heparin 1 mg/kg was administered after dissection of the internal mammary artery to maintain the activated clotting time at 250 s during anastomosis. Using the pad, the heart was displaced in various directions and angles along the vessel for grafting to expose the coronary territories and a tissue stabilizer (Octopus Tissue Stabilization System: Medtronic, Minneapolis, MN, USA) was applied. During displacement of the beating heart, the patients were placed in a 10-20° head-down tilt position and norepinephrine 0.03-0.05 µg/kg per minute was infused intermittently if the mean systemic arterial pressure (MAP) decreased to < 60-65 mmHg.
Hemodynamic variables were recorded at the following time points: during left anterior descending (LAD) anastomosis at 1 min (T1) and 5 min (T2); during obtuse marginal (OM) anastomosis at 1 min (T3) and 5 min (T4); and during right coronary artery (RCA) anastomosis at 1 min (T5) and 5 min (T6). The variables measured included SCO, CCO, APCO, and UCCO.
All data were expressed as the number of patients or means ± SD. Sample size calculation was conducted based on a study conducted to evaluate the accuracy of cardiac output (CO) measurements during OPCAB [8], and the number patients required to analyze the clinical agreement between measurement techniques with α = 0.05 and β = 0.2 was found to be 18. Pearson's correlation among SCO, CCO, APCO, and UCCO during OPCAB was evaluated using SPSS 12.01. Agreement among the CO measurement methods was quantified by calculating the bias and precision as recommended by Bland and Altman [23]. Bias represents the mean difference between consecutive UCCO and SCO, UCCO and CCO, and UCCO and APCO. Precision was defined as the SD of the average of the biases. A paired t-test was also applied to test the differences of the means between SCO, CCO, APCO, and UCCO. A P value < 0.05 was considered statistically significant.
Results
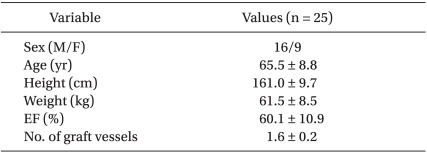
Twenty five patients were enrolled in this study. Their demographic data are shown in Table 1. OM anastomoses and RCA anastomoses were not conducted in six patients and five patients, respectively. Of the 19 patients that received OM anastomoses, SCO measurement results were not seen in two patients at 1 min in one patient at 5 min. In one patient that received OM anastomoses, CCO measurement results at 5 min was not seen. Of the 20 patients that received RCA anastomoses, CCO measurement results at 1 and 5 min during anastomosis in one patient and SCO measurements at 1 min in three patients and 5 min in one patient were not seen. No adverse effects were observed during the entire study period.
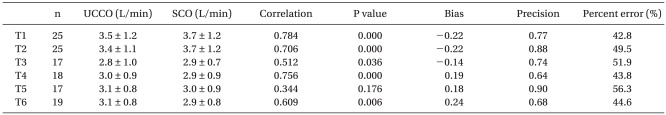
SCO were closely correlated with UCCO during LAD and OM anastomoses. During RCA anastomoses, the correlation between UCCO and SCO was significant only at 5 min (Table 2).
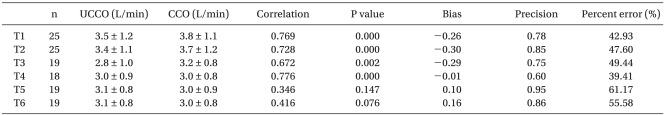
The measurement of UCCO and CCO during LAD and OM anastomoses was also well correlated. However, UCCO and CCO during RCA anastomoses showed low correlation throughout the study period (1 min: r = 0.346, P = 0.147; 5 min: r = 0.416, P = 0.076) (Table 3).
The correlations between UCCO and APCO were significant at 1 and 5 min during LAD anastomoses and at 1 min during RCA anastomosis. The correlations between UCCO and APCO were not significant in other periods (Table 4).
Using the Bland-Altman method, the percent error did not meet the criteria of 30% suggested by Critchley during any of the study periods for all of the CO measurement techniques. Additionally, a paired t-test showed that the mean values of SCO, CCO, and UCCO did not differ. However, the mean values of APCO and UCCO differed significantly (P = 0.000) during all study periods.
The results of the statistical analyses are summarized in Table 2-4.
Discussion
In the current study, the accuracy and precision of estimation by SCO, CCO, and APCO and their comparison with UCCO during beating heart surgery was conducted. The results revealed that CO values estimated from SCO, CCO, and APCO were well correlated with UCCO during LAD anastomosis. The values of UCCO and SCO, CCO during OM anastomosis were also well correlated, but the CO values estimated from both UCCO and APCO were not. The correlations among SCO, CCO, APCO, and UCCO during RCA anastomosis did not provide consistent results. However, the percent error observed was higher than the criteria of 30% defined by Critchley and Critchley [24] during all study periods for all CO measurement techniques. Therefore, there were fewer agreements between the three methods and UCCO during vessel anastomoses in OPCAB.
Intermittent bolus thermodilution cardiac output (ICO) with ice saline via a PAC is currently "the method of choice" for the measurement of CO in clinical practice [4]. However, in a large study, PAC was found to increase mortality, hospital stay, and cost [25]. Therefore, alternative methods such as CCO and SCO that are less invasive and/or allow realistic calculation of CO have been developed [4]. There are many factors that could reduce the accuracy of the methods [13,15]. For example, the response time of CCO measurement has a delay. Specifically, a trended CCO measurement is displayed every 30 to 60 s, which reflects an average flow over the previous 3-6 min. Because CCO takes 3-6 min to show a change in its value, there is the potential for a delay in the monitoring of acute CO changes and subsequent therapeutic intervention. To minimize the response time, the SCO mode can be used to average CO over the last three measurements [14]. Many studies have shown that SCO and CCO are well correlated with ICO and can replace the ICO [6,8,26,27].
The Vigileo/FloTrac calculates CO using arterial waveform characteristics and a patient's demographic data. The relationship between pressure pulse and stroke volume depends on the characteristics of the arterial vascular tree. Several studies concerning the accuracy of Vigileo CO monitoring in a variety of patients have been conducted. Many studies demonstrated clinically acceptable precision compared with a standard technique of known accuracy [3,21,28].
These CO measurement methods are available in clinical practice, and many studies have shown good to excellent agreement among them [3-12]. However, the studies that have been conducted to date were performed during the entire surgical period or physiologically stable periods [3-6]. The design of the present study is unique in that the accuracy of different CO measurement techniques was assessed according to the period in which each vessel was being manipulated. During the positioning for the grafting of the circumflex artery and posterior descending artery branches, the heart must be displaced anteriorly, which results in the apex of the heart being pointed more upward compared with LAD anastomoses [1,15]. Thus, hemodynamic changes are more pronounced with displacement of the heart to access the circumflex artery or posterior coronary artery than anterior vessels, which influences the accuracy of different CO measurement techniques.
Although CO measurement using the PAC is considered the gold standard method, during beating heart surgery, this catheter has some limitations. First, tricuspid regurgitation, which was developed or aggravated during direct manipulation and dislocation of the heart [15], permits backflow of both blood and the indicator, thereby possibly causing inaccurate readings using PAC [18]. Secondly, during continuous CO measurement (SCO, CCO), relatively small quantities of heat are used to calculate the CO. Thus, infusion of high quantities of infusate, which may often be required to maintain hemodynamics, may influence this method's accuracy and reliability [19]. APCO is also considered a clinically applicable method for CO assessment, but this agreement has not been observed in patients under unstable hemodynamic condition. For example, bolus administration of inotropes or vasopressors resulting in a sudden change in vascular tone was found to be associated with the lowest agreement between APCO and thermodilution CO [16]. OPCAB surgery results in the geometry of the heart being incompatible with effective ejection and venous return due to obstructions caused by torque cardiac positioning during anastomosis. Accordingly, vasopressors, inotropes, and volume expanders have routinely been administered to support hemodynamics during OPCAB surgery [16] and influence APCO accuracy. Therefore, we proposed that UCCO be judged against the accuracy of the reference method during beating heart surgery. This is based on the assumption that UCCO measurements are more accurate than other modalities for CO measurement during heart positioning in OPCAB because true pulse-wave signals are obtained from the descending aorta by M-mode ultrasound representing the true stroke volume [22].
Overall, these findings suggest that the correlation among SCO, CCO, and APCO likely differ according to the time periods in which each vessel is manipulated. Access to the different coronary arteries during OPCAB requires heart displacement. This displacement causes hemodynamic changes that may vary depending on the vessel to be bypassed [1,15]. During positioning for grafting of the circumflex artery and posterior descending artery, factors that influence the accuracy of CO measurement techniques are more pronounced with heart displacement. In the present study, we found that the correlations between SCO, CCO, APCO and UCCO were better during LAD anastomoses than OM and RCA anastomoses. This was especially true during RCA anastomoses, as the correlation among the three different CO measurement techniques was inconsistent. However, the SCO, CCO, and APCO values did not agree with the UCCO data during any of the vessel manipulation periods. Therefore, we speculate that when the positioning for vessels anastomoses, the correlation and agreement of SCO, CCO, and APCO with UCCO decreased due to the factors mentioned above.
The limitations of this study should be noted. First, UCCO has inconsistent results in the literature. Initial studies showed significant variability between the UCCO and thermodilution measurements, and the technique was found to be unacceptable because of operator dependency and the frequently necessary readjustment of the echo probe [29]. In the current study, the operators were trained to obtain an optimal signal before commencement of the study and were considered proficient in the use of the device. We also used an echo probe (Hemosonic; Arrow International, Everett, MA, USA), which offers the advantage of determining the true aortic diameter by M-mode ultrasound, thus avoiding errors introduced by nomogram-derived calculations. Measurements performed with this device are in good agreement with PA thermodilution CO [4,5,7,9-12].
Second, the authors did not compare various CO measurements with ICO. While ICO is currently the method of choice for measurement of CO in clinical practice, it has well-known pitfalls related to operator variation. In addition, ICO requires a set of hands to shoot the output, and the injection of iced saline can cause short-lived cardiodepressant effects [30] at the critical time of repositioning, when the patient is most likely to have an unstable hemodynamic condition. Although computerized continuous CO (SCO, CCO) has its own limitations, validation studies have shown that these techniques can replace the ICO [6,8,26,27]. In our opinion, the repeated thermodilution measurements conducted during this study may be impractical and unnecessary.
In summary, during vessel anastomosis in OPCAB, the SCO, CCO, and APCO showed different correlations with UCCO according to the coronary artery being grafted at the moment. Futhermore, no agreement was shown between the CO measurements during the artery grafts. Therefore, the CO values from various techniques should be interpreted with caution during graft anastomosis in OPCAB.