Does a single dose of intravenous nicardipine or nimodipine affect the bispectral index following rapid sequence intubation?
Article information
Abstract
Background
Theoretically, L-type calcium channel blockers could modulate anesthetic effects. Nicardipine does not affect the bispectral index (BIS), but nimodipine, which can penetrate the blood-brain barrier, has not been studied. The aim of this study was to evaluate whether a single dose of intravenous nicardipine or nimodipine could affect BIS following rapid sequence intubation.
Methods
This study was done in a double-blind, randomized fashion. Anesthesia was induced with fentanyl 2 µg/kg, thiopental sodium 5 mg/kg, and 100% oxygen. After loss of consciousness, patients received rocuronium 1.0 mg/kg and either a bolus of 20 µg/kg nicardipine, nimodipine, or a comparable volume of normal saline (n = 20). Intubation was performed 1 min after study drug administration. BIS, mean blood pressure (MBP), and heart rate (HR) were measured before anesthetic induction, after loss of consciousness, before intubation, during intubation, and 1, 2 and 5 min after intubation.
Results
BIS dropped rapidly after induction but increased to 60 before intubation in all groups irrespective of study drug. In nimodipine, the increase in BIS during intubation was not significant compared to pre-intubation, in contrast to the other two groups, but there was no difference in BIS during intubation. HR significantly increased, but MBP just rose to pre-induction values after intubation in nicardipine and nimodipine groups. BIS, MBP, and HR following intubation increased in control group.
Conclusions
A single dose of intravenous nicardipine or nimodipine could attenuate blood pressure increases but not affect BIS increases in rapid sequence intubation.
Introduction
Theoretically, L-type calcium channel blockers (CCB) could influence anesthetic potency through modulating intracellular messenger function and post synaptic neuronal excitability, affecting secretion of neurotransmitters, or indirectly altering hemodynamics. L-type calcium channels exist in sensory neurons in the spinal cord and the brain [1,2]. L-type CCB potentiate the action of sedatives [3], opioids [4], and anesthetics [5] and several anesthetics act on L-currents in neurons [6-8]. However, CCB activity on anesthesia is still controversial [9,10]. If CCB is administered via a peripheral intravenous route, it needs to cross the blood-brain barrier (BBB) to show anesthetic effects. Nicardipine weakly crosses the BBB, whereas nimodipine crosses better [11].
Intubation causes a peripheral nociceptive response that can induce central arousal [12]. Endotracheal intubation can increase the bispectral index (BIS) and change hemodynamics [12,13]. We compared BIS and hemodynamic changes for nicardipine and nimodipine, which cross the BBB differently, after rapid sequence endotracheal intubation.
Materials and Methods
This study was approved by the Institutional Review Board of our hospital, and written informed consent was obtained from each patient. We enrolled ASA physical status I patients who were scheduled for elective surgery under general anesthesia. Patients with a history of hypertension, diabetes mellitus, body weight >130% of ideal body weight, cardiovascular or cerebrovascular disease, and those receiving medications that affect cardiovascular and psychological function were excluded. The age range was from 18-60 years. Patients were randomly allocated into 3 groups using a computer-generated sequence (n = 20, each).
No premedication was administered. All patients were monitored with noninvasive blood pressure, electrocardiogram, temperature, and peripheral oxygen saturation. BIS was monitored using an Aspect A-1000 EEG monitor, version 3.12 (Aspect Medical Systems, Natick, USA). Baseline values of BIS and vital signs were recorded before induction of anesthesia. Rapid sequence intubation was designed to increase BIS in the control group. Under monitoring, intravenous fentanyl 2 µg/kg was given and anesthesia was induced with thiopental sodium 5 mg/kg and 100% oxygen. After loss of consciousness, patients received rocuronium 1.0 mg/kg and at the same time either a bolus of nicardipine 20 µg/kg, nimodipine 20 µg/kg, or a comparable volume of normal saline. One minute after study drug administration, the trachea was intubated with a direct laryngoscope by a second-year anesthesia resident. Only one attempt was allowed for tracheal intubation. Intubation was accomplished within 30 sec in all cases. After intubation, ventilation was controlled with 1 vol% sevoflurane in 100% oxygen for 5 min. End-tidal carbon dioxide concentration was maintained between 35-40 mmHg throughout the study. Mean blood pressure (MBP), heart rate (HR), and BIS value were recorded before induction of anesthesia (B0), after loss of consciousness (B1), before intubation, during intubation (L0), 1, 2 and 5 min after intubation (L1, 2, and L5). We allocated 16 patients to each group to detect a 5-point increase in BIS after intubation, with α = 0.05 and β = 0.2 [14]. To compensate for drop out, we targeted 20 patients in each group. Data are presented as mean ± SD. SPSS version 12.5 (SPSS Inc, Chicago, IL) was used for analysis.
Statistical analysis was performed using the chi-square test or one-way analysis of variance followed by the Tukey test. One-way analysis of variance for repeated measures followed by multiple comparisons was performed for time-dependent variables. P < 0.05 was considered statistically significant.
Results
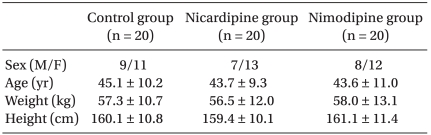
A total of 63 patients were included in the study. Two patients in the nicardipine group and one patient in the control group were excluded from the study due to difficult intubation. No differences were observed in demographic data, baseline hemodynamics, and BIS values before induction of anesthesia (Table 1).
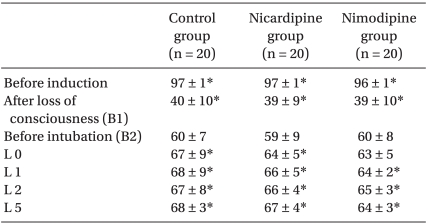
BIS values rapidly fell after induction of anesthesia (B1) and then increased up to 60 just before intubation in all groups. Nicardipine or nimodipine injection did not affect BIS values 1 min after drug injection. BIS values significantly increased by 7-8 after intubation in controls compared to baseline (B2) (P < 0.05, Table 2). Nicardipine injection did not block the increase in BIS following intubation. In the nimodipine group, the increase in BIS during intubation (L0) was not significantly different than baseline (B2), in contrast to the other two groups. However, there was no difference in BIS during intubation (L0) in any group (P = 0.09 vs. control) (Table 2).
MBP fell before intubation in all groups (B2), with larger changes in the nimodipine group (P < 0.05 compared to controls). Intubation increased MBP in controls, but the MBP at 1 or 2 min after intubation (L1, 2) in nimodipine or nicardipine group was similar to before anesthetic induction (P < 0.05 compared to control group) (Table 3).
HR significantly rose 1 min after intubation and remained elevated in the control group (P < 0.05 compared to pre-induction value). HR rose at 1 min after administration of nicardipine or nimodipine, and remained elevated until 5 min after intubation in the nicardipine or nimodipine group. The nicardipine group showed the highest HR during intubation and 2 min after intubation (L0 and L2) (Table 3).
Discussion
Here, a single dose of intravenous nicardipine or nimodipine blocked blood pressure increases after rapid sequence endotracheal intubation, but did not change BIS increases. CCB may modify anesthetic effects. Dihydropyridine CCB and nitrendipine potentiate the anesthetic effects of benzodiazepine, and Bay K 8644 (an L-type calcium channel activator) reduced the anesthetic potency of midazolam [3]. Verapamil decreased the MAC of halothane in dogs [15], and intrathecally administered L-type calcium channel blockers produce anti-nociceptive effects in rats [16]. Intravenous nicardipine and diltiazem did not affect BIS under general anesthesia in hypertensive patients [17]. Intravenous nicardipine did not affect anesthetic depth in response to endotracheal intubation [13,18]. Generally, passage of nicardipine across the BBB is limited, whereas nimodipine is relatively permeable to the BBB. L-type CCB are more effective anesthetics when used via the intrathecal or epidural route than intravenously. Intravenously administered nimodipine enhanced the analgesic effect of epidural morphine and epidural nimodipine alone produced brief but intense analgesia [19].
We found that intravenous nimodipine could block the increase in BIS during intubation, but the BIS differences of 4-5 before and during intubation were not sufficient to show any statistical or clinical significance compared to controls. Nicardipine has a rapid onset of action of 1-2 min. Nicardipine 15-30 µg/kg is usually used at 1 min prior to intubation to reduce the hemodynamic response associated with endotracheal intubation. We chose a 20 µg/kg single dose of nicardipine and nimodipine. Other administration routes such as continuous intravenous or intrathecal administration may increase the interactions with anesthetics.
Changes of BIS values after stimulation are caused by direct effects on neuronal function [20] or by indirectly affecting cerebral blood flow [21,22]. Intubation releases central and peripheral catecholamine and increases BIS, MBP, and HR [12,23]. In general, peripheral catecholamine does not cross the BBB. High MBP raises cerebral blood flow and might open the BBB to improve drug effects [24-26]. Peripherally administered nicardipine or nimodipine blocked the increase in MBP associated with endotracheal intubation, but failed to block the increase in BIS, implying little indirect action on BIS through affecting hemodynamics or blocking movement of peripheral catecholamine.
Intravenous epinephrine can influence BIS [27]. In BIS 50, the BIS value did not change in response to intravenous epinephrine, but the BIS 70 value rose after epinephrine treatment [27]. Esmolol can blunt the increase in BIS after endotracheal intubation during sevoflurane anesthesia but not desflurane anesthesia [28], probably via the sympathetic stimulation of desflurane. The same stimulation induces different BIS responses according to the underlying conditions. We evaluated the effects of nicardipine and nimodipine on BIS in rapid sequence intubation, which might increase BIS values. However, nicardipine and nimodipine did not affect pre-intubation BIS values in the range of 57-60.
In conclusion, a single dose of intravenous nicardipine or nimodipine decreased the blood pressure response to endotracheal intubation, but did not affect the BIS increase. These results suggest that a single dose of intravenous nicardipine or nimodipine can blunt the hemodynamic response associated with endotracheal intubation but does not affect anesthetic depth in rapid sequence intubation.