 |
 |
| Korean J Anesthesiol > Volume 76(5); 2023 > Article |
|
Abstract
Background
Methods
Results
NOTES
Conflicts of Interest
Jung-Hee Ryu has been an editor for the Korean Journal of Anesthesiology since 2018. However, she was not involved in the review process of this article, including peer reviewer selection, evaluation, or decision-making. There were no other potential conflicts of interest relevant to this article.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
Chang-Hoon Koo (Data curation; Formal analysis; Investigation; Methodology; Visualization; Writing ŌĆō original draft)
Insung Hwang (Data curation; Investigation; Methodology; Writing ŌĆō original draft)
Hyun-Jung Shin (Data curation; Formal analysis; Methodology; Supervision; Validation; Writing ŌĆō review & editing)
Jung-Hee Ryu (Conceptualization; Data curation; Formal analysis; Investigation; Supervision; Validation; Writing ŌĆō review & editing)
Supplementary Materials
Supplementary┬ĀFig.┬Ā1.
Supplementary┬ĀFig.┬Ā2.
Supplementary┬ĀFig.┬Ā3.
Supplementary┬ĀFig.┬Ā4.
Supplementary┬ĀFig.┬Ā9.
Fig.┬Ā1.

Fig.┬Ā2.
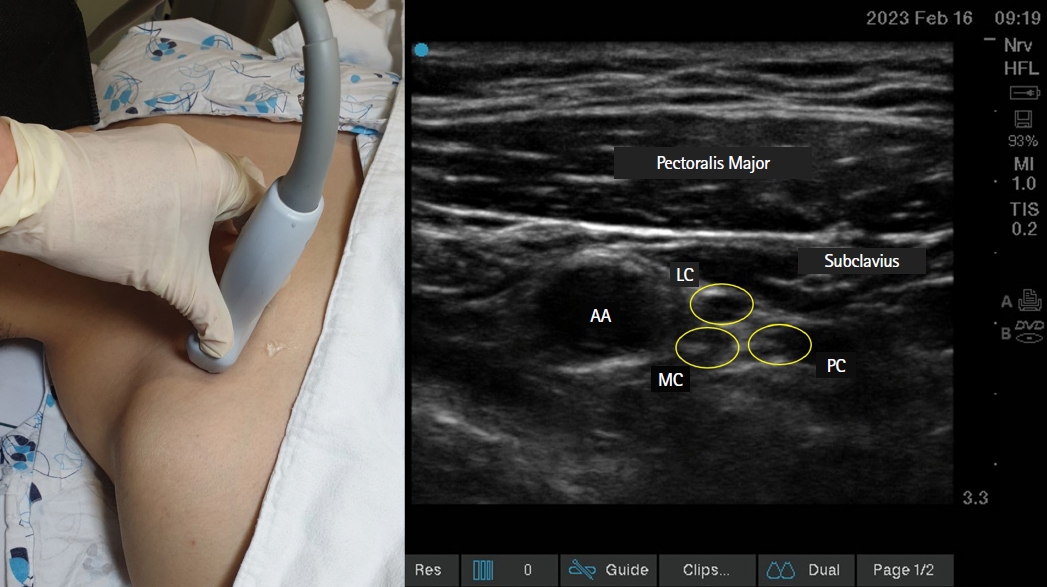
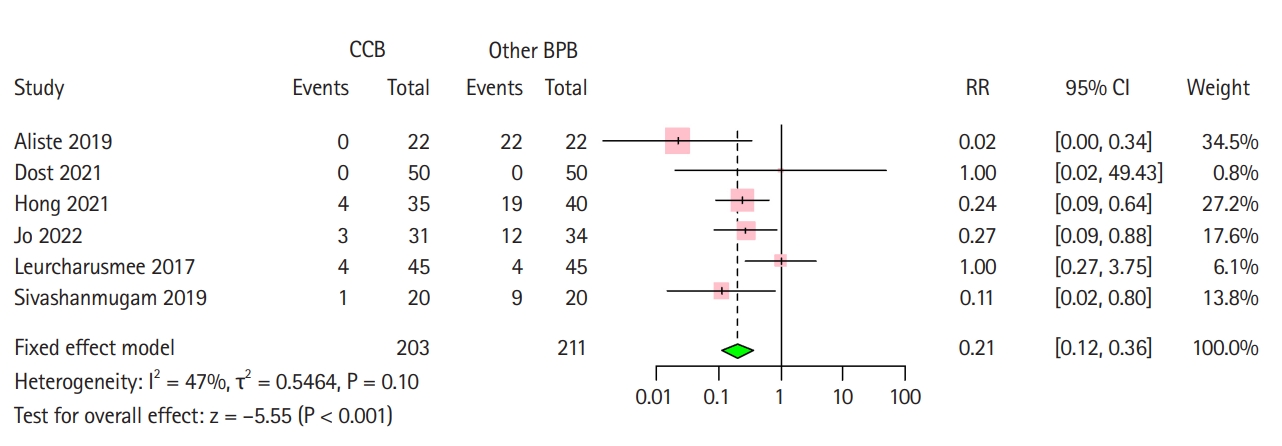
Fig.┬Ā3.
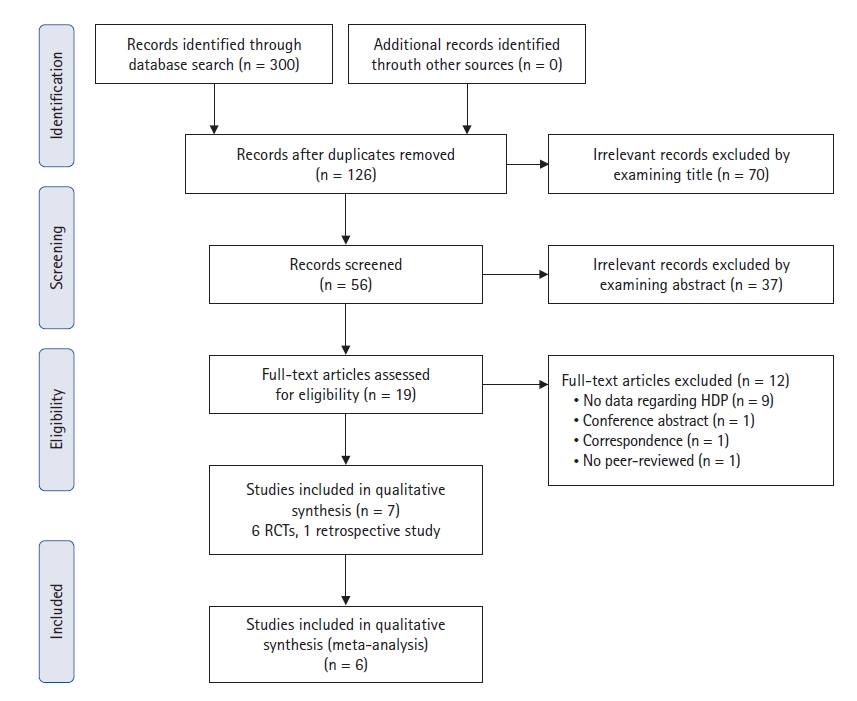
Fig.┬Ā4.
Table┬Ā1.
| Author & year | Study design | Sample size | Control block | Assessment of HDP | Local anesthetics | |
|---|---|---|---|---|---|---|
| CCB | Other BPB | |||||
| Aliste 2019 [27] | RCT | 22 | 22 | Interscalene block | US | 0.5% levobupivacaine, 20 ml |
| Dost 2021 [26] | RCT | 50 | 50 | Lateral sagittal block | Not described | 0.5% bupivacaine, 20 ml |
| Hong 2021 [6] | RCT | 35 | 40 | Supraclavicular block | US | 1:1 mixture of 1% lidocaine and 0.75% ropivacaine, 20 ml |
| Jo 2022 [28] | RCT | 31 | 34 | Superior trunk block | US | 0.5% ropivacaine, 20 ml |
| Leurcharusmee 2017 [8] | RCT | 45 | 45 | Paracoracoid block | US | 1:1 mixture of 1% lidocaine and 0.25% bupivacaine, 35 ml |
| Oh 2020 [29] | Retrospective cohort study | 118 | 118 | Supraclavicular block | Chest radiograph | 1:1 mixture of 1% lidocaine and 0.75% ropivacaine, 20ŌĆō30 ml |
| Sivashanmugam 2019 [7] | RCT | 20 | 20 | Supraclavicular block | US | 1:1 mixture of 2% lidocaine and 0.5% bupivacaine, 20 ml |









