 |
 |
| Korean J Anesthesiol > Volume 76(4); 2023 > Article |
|
Patients with myotonic dystrophy (MD) have greater sensitivity to general anesthetics and neuromuscular blocking (NMB) agents; therefore, critical issues associated with general anesthesia have been reported, such as delayed emergence from anesthesia and postoperative cardiovascular and respiratory complications [1]. As volatile anesthetics may induce malignant hyperthermia in patients with MD [2], total intravenous anesthesia (TIVA) is commonly used for general anesthesia in this patient population. However, propofol, which is commonly used in TIVA, may induce delayed emergence from anesthesia and respiratory depression even at low maintenance doses in this population [1,3]. Morimoto et al. [3] reported that the effect-site propofol concentration at which patients with MD recovered from anesthesia was lower than the institutional average for healthy adults, suggesting that sensitivity to propofol might be higher in patients with MD.
Remimazolam is a benzodiazepine receptor agonist that was approved as a general anesthetic in Japan in 2022. This ultrashort-acting anesthetic can produce hemodynamic stability with a fast onset and offset and can be fully antagonized with flumazenil. Herein, we report the successful anesthetic management of a patient with MD using remimazolam and remifentanil with local anesthetics, without NMB agents, as a preventive measure for delayed emergence from anesthesia and postoperative respiratory failure. Written informed consent was obtained from the patient for publication of this case.
A 59-year-old man with a one-year history of MD was scheduled to undergo temporomandibular joint arthroplasty. His MD symptoms included eyelid dropping, mild anarthria, and mild lower-extremity muscle weakness. He was also diagnosed with a complete atrioventricular block and had subsequently undergone pacemaker implantation. The pacemaker was set in the DDD mode at 80 beats/min. Preoperative pulmonary function test results revealed values at the lower limit of normal. The routine preoperative tests showed no other abnormal findings. Considering the possibility of malignant hyperthermia induced by volatile anesthetics, aberrant sensitivity to NMB agents [1,2], and sensitivity to the respiratory depressant effects of propofol and opioids [1,3,4] in patients with MD, we planned to use TIVA with remimazolam and remifentanil, which are ultrashort acting and supplementary local anesthetics, without NMB agents, to reduce the risk of delayed emergence from anesthesia and postoperative respiratory insufficiency.
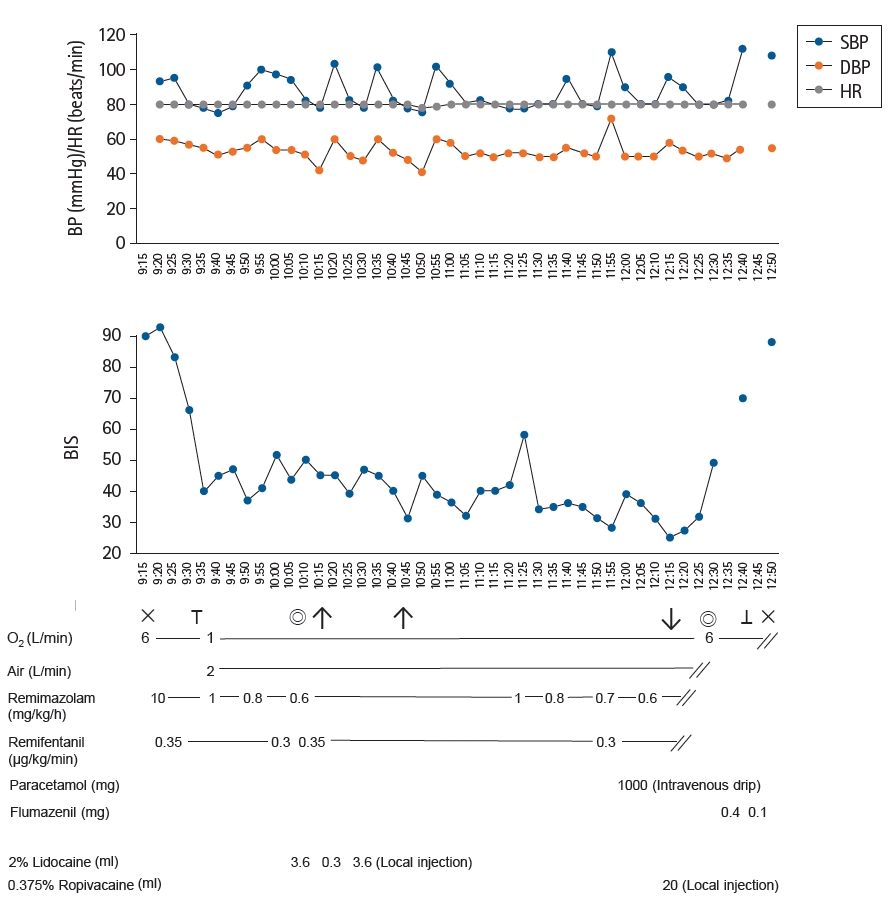
We administered 10 mg/kg/h of remimazolam and 0.35 ┬Ąg/kg/min of remifentanil for approximately 3 min until the patient was unresponsive to verbal commands and his bispectral index (BIS) was below 60. After establishing adequate mask ventilation, we confirmed that the intubating condition was excellent and subsequently performed nasal intubation successfully without body motion using a McGRATH┬« MAC laryngoscope (Covidien, Medtronic Inc., Japan). After nasal intubation was successfully completed, an infusion dose of remimazolam at 1.0 mg/kg/h was initiated. During surgery, we administered a continuous infusion of remimazolam (0.6ŌĆō1.0 mg/kg/h) and remifentanil (0.3ŌĆō0.35 ┬Ąg/kg/min) to maintain adequate anesthesia depth (BIS < 60) and stable hemodynamics. Additionally, the surgeons injected 2% lidocaine into the surgical site during surgery for analgesia. We maintained the core body temperature over 36.0┬░C using a forced-air warming system to prevent the patient from shivering after emergence from anesthesia. We stopped the infusion of all anesthetics approximately 10 min before termination of surgery because of the patientŌĆÖs low BIS. At the end of the surgery, in addition to the intravenous administration of 1,000 mg of paracetamol, 20 ml of 0.375% ropivacaine was injected bilaterally into the surgical sites to ensure postoperative analgesia. Approximately 3 min after the termination of surgery, the patient was responding to verbal commands with sufficient spontaneous breathing. Subsequently, flumazenil (0.5 mg) was administered to boost emergence from anesthesia, and the patient was immediately extubated uneventfully (Fig. 1). During surgery, no bolus administration of remimazolam or remifentanil was required, and the total consumption of remimazolam and remifentanil was 128 mg and 4.1 mg, respectively. The surgeons were satisfied with the condition of the surgical sites and muscle relaxation was considered adequate. The patient did not complain of pain and the postsurgical course was uneventful. After rehabilitation, the patient was discharged on postoperative day 15.
Patients with MD can develop critical complications after general anesthesia, such as prolonged recovery from anesthesia and postoperative respiratory failure [1]. Previous to this case, we had encountered a patient with MD who developed delayed postoperative respiratory failure three days after open cholecystectomy under general anesthesia with propofol-based TIVA, and neuromuscular blocks were fully reversed with sugammadex [1]. Compared to propofol, which can induce prolonged emergence from anesthesia and respiratory depression in patients with MD [1,3], the benefits of remimazolam include ultrashort-acting features, a less pronounced muscle relaxant effect, less circulatory depression, and the availability of flumazenil to fully reverse the anesthetic effect [5]. Thus, remimazolam appears to be more appropriate for patients with neuromuscular disease with aberrant sensitivity to general anesthetics, especially because delayed emergence from anesthesia can be avoided using the antagonist flumazenil.
In this case, we decided not to use non-ultrashort-acting opioids (e.g., fentanyl or morphine) or N-methyl-D-aspartate receptor antagonists (e.g., ketamine) for postoperative analgesia to avoid possible postoperative respiratory depression. Instead, we used local anesthetics at the surgical sites and intravenous paracetamol. This appeared to have less of an effect on the postoperative respiratory condition of this patient while also providing sufficient postoperative analgesia. Depending on the surgical procedure, in addition to local anesthetic infiltration at the surgical sites, peripheral and central nerve blocks can also be used instead of non-ultrashort-acting opioids for analgesia under general anesthesia with remimazolam and remifentanil in patients with neuromuscular disease to avoid delayed emergence from anesthesia and postoperative respiratory insufficiency.
In conclusion, general anesthesia using remimazolam and remifentanil in combination with regional anesthesia may be a better option for patients with MD to reduce the risk for delayed emergence from anesthesia and postoperative respiratory insufficiency.
NOTES
Author Contributions: Yukihide Koyama (Data curation; Writing ŌĆō original draft); Haruko Nishikawa (Data curation; Writing ŌĆō review & editing); Yoriko Murase (Data curation; Writing ŌĆō review & editing); Kei Morita (Data curation; Writing ŌĆō review & editing); Koichi Tsuzaki (Supervision; Writing ŌĆō review & editing)
Fig.┬Ā1.
Anesthesia record for this patient. BP: blood pressure, HR: heart rate, SBP: systolic blood pressure, DBP: diastolic blood pressure, BIS: bispectral index, ├Ś: start of anesthesia or termination of anesthesia, ŌÅē: tracheal intubation, ŌÅŖ: extubation, Ōåæ: skin incision, Ōåō: skin closure, and ŌŚÄ: start or termination of surgery.
References
1. Koyama Y, Kohno M, Tsuzaki K, Kamiyama K, Morimoto Y. Bilevel positive airway pressure therapy in a patient with myotonic dystrophy and postoperative respiratory failure: a case report. Saudi J Anaesth 2020; 14: 241-3.



2. Yoo SW, Baek SJ, Kim DC, Doo AR. A case report of malignant hyperthermia in a patient with myotonic dystrophy type I: a CARE-compliant article. Medicine (Baltimore) 2021; 100: e25859.



3. Morimoto Y, Mii M, Hirata T, Matayoshi H, Sakabe T. Target-controlled infusion of propofol for a patient with myotonic dystrophy. J Anesth 2005; 19: 336-8.



4. Gaszynski T. Opioid-free general anesthesia in patient with Steinert syndrome (myotonic dystrophy): case report. Medicine (Baltimore) 2016; 95: e4885.



5. Antonik LJ, Goldwater DR, Kilpatrick GJ, Tilbrook GS, Borkett KM. A placebo- and midazolam-controlled phase I single ascending-dose study evaluating the safety, pharmacokinetics, and pharmacodynamics of remimazolam (CNS 7056): Part I. Safety, efficacy, and basic pharmacokinetics. Anesth Analg 2012; 115: 274-83.


- TOOLS
-
METRICS

-
- 1 Crossref
- Scopus
- 1,860 View
- 134 Download








