 |
 |
| Korean J Anesthesiol > Volume 76(4); 2023 > Article |
|
Dear Editor,
Pain management in patients with Duchenne muscular dystrophy (DMD) is complex. Considering that most treatment options are insufficient at managing the hip pain caused by severe joint deformity and contractures, an increasing importance has been placed on denervation methods for the hip joint [1].
The anterior capsule of the hip joint is densely innervated and plays an essential role in the formation of pain sensations [2]. Sensory innervation of this region is provided by the femoral nerve (FN), obturator nerve (ON), and accessory obturator nerve (AON). A recent anatomical study revealed that the anterior hip joint capsule is more innervated by the FN and AON than that by the ON [3]. Therefore, the FN and AON are considered appropriate targets for hip analgesia and denervation.
This case report aimed to present a successful pericapsular nerve group (PENG) block and FN and AON radiofrequency (RF) denervation method using ultrasonography (USG) imaging in a patient with DMD.
A 19-year-old male patient diagnosed with DMD was admitted to our clinic with throbbing and stabbing-like pain localized to the anterior of the right hip for one year that increased with movement. The patient’s numeric rating scale (NRS) score was 10/10 during movement and 8/10 at rest. The hip pain did not improve after various conservative treatments. The patient had a 70° right hip joint flexion contracture and on physical examination, the range of motion of the hip joint was limited and painful in all directions. Pelvic computed tomography revealed a significant increase in intraarticular fluid in both femoroacetabular joints. Therefore, we decided to administer a PENG diagnostic block under USG guidance. The patient was informed about the procedure, and consent was obtained.
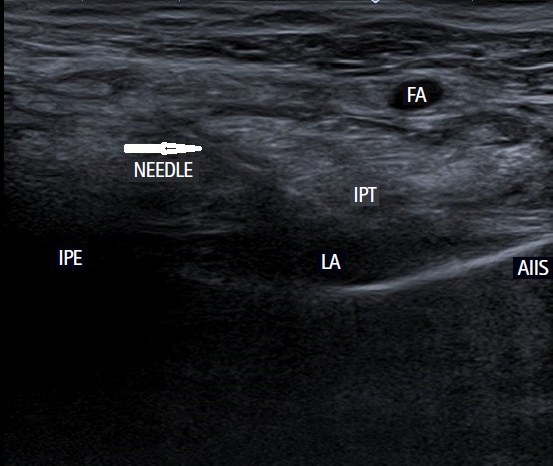
A sterile 8–13 MHz linear USG probe was first placed on the anterior superior iliac spine and then caudally on the anterior inferior iliac spine. The probe was obliquely rotated by approximately 45° and placed on the pubic ramus. The iliopubic eminence; femoral artery, vein, and nerve; and iliopsoas muscle tendon were visualized. A 22-gauge 100-mm needle was inserted in-plane from the lateral to the medial direction, and 15 ml of 0.25% bupivacaine was injected between the iliopsoas tendon and pubic ramus, as described by Girón-Arango et al. [2] (Fig. 1).
In the first 48 h following the injection, the patient reported that his pain had decreased by more than 50% and his capacity to perform activities of daily living had improved. Therefore, RF denervation was performed. A 100-mm, 22-gauge, 10-mm active-tipped RF needle was placed in the area where the PENG block was administered, targeting the same structures (articular branches of the FN and AON). Swelling, fullness, and tingling sensations towards the hip joint were observed with sensory stimulation at 50 Hz, and no movement was observed with motor stimulation at 2 Hz. Tissue impedance was below 300 ohms. After obtaining appropriate stimulus responses, 3 ml of 2% lidocaine was administered into the injection site. RF thermal coagulation at 80°C was performed at three separate points in the area where the PENG block was performed for 60 s. On the first day after the procedure, the NRS score had decreased, and at the first-, third-, and sixth-month follow-ups, the NRS score was 3 with movement. There were no complications following the procedure.
Common symptoms of DMD include muscle weakness and limited movement. As these symptoms progress, the risk of pain in patients with DMD increases. Many treatment modalities provide temporary pain relief, especially in large joints such as the hip joint. However, long-term use of nonsteroidal anti-inflammatory drugs and opioids in this patient group is limited because of their side effects. Surgical treatment options carry a relatively high risk of mortality and may be inadequate for pain management. Therefore, the importance of hip joint denervation methods have increased [1].
The RF denervation method has been successfully applied in patients with hip pain who cannot undergo total hip arthroplasty because of comorbidities. Although the optimal anatomical targets, technical aspects, selection criteria, and efficacy for treatment of hip pain have not been clarified, the number of publications on RF denervation of the hip joint has increased. Considering that the articular branches of the FN and AON play primary roles in conveying the pain sensation of the hip joint, Girón-Arango et al. [2] described a PENG block performed using USG targeting the articular sensory branches of the FN and AON for analgesia after a hip fracture. Although these tiny articular branches are very difficult to see on ultrasound, they have been observed in cadaveric studies. In one cadaveric study, dye was injected into the iliopsoas plane under USG and was detected around the articular nerve branches of the hip joint after dissection [4]. Another cadaveric study showed that the space between the anterior inferior iliac spine and the iliopubic eminence is an effective region for applying RF to the sensory fibers of the hip joint [3].
Hip joint RF denervation methods were first conducted under fluoroscopy. However, multiple needle insertions may be required to identify the appropriate sensory responses during RF application under fluoroscopy. After insertion, the needle can be redirected. However, as the innervation of the joint is complex, using the same guide points may not always be appropriate [3]. Redirecting the needle can also increase the risk of arterial and venous injuries. In one study, fluoroscopy and USG were used together for hip denervation. After inserting the needle under fluoroscopy, the distance between the needle and vascular structures was measured using USG. A distance of 0.55 cm was observed between the femoral vein and needle tip [5]. Under fluoroscopy, the vessel can be injured with minor redirections of the needle after insertion.
In conclusion, denervation methods should be considered in patients who have hip pain with advanced functional limitations and comorbidities. The articular sensory branches of the femoral and AON may be appropriate targets for hip joint analgesia.
Fig. 1.
Pericapsular nerve group (PENG) block sonogram image. FA: femoral artery, IPT: iliopsoas tendon, IPE: iliopubic eminence, LA: local anesthetic, AIIS: anterior inferior iliac spine.
References
1. Bhatia A, Hoydonckx Y, Peng P, Cohen SP. Radiofrequency procedures to relieve chronic hip pain: an evidence-based narrative review. Reg Anesth Pain Med 2018; 43: 72-83.


2. Girón-Arango L, Peng PW, Chin KJ, Brull R, Perlas A. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med 2018; 43: 859-63.


3. Short AJ, Barnett JJ, Gofeld M, Baig E, Lam K, Agur AM, et al. Anatomic study of innervation of the anterior hip capsule: implication for image-guided intervention. Reg Anesth Pain Med 2018; 43: 186-92.


4. Nielsen ND, Greher M, Moriggl B, Hoermann R, Nielsen TD, Børglum J, et al. Spread of injectate around hip articular sensory branches of the femoral nerve in cadavers. Acta Anaesthesiol Scand 2018; 62: 1001-6.



5. Kapural L, Jolly S, Mantoan J, Badhey H, Ptacek T. Cooled radiofrequency neurotomy of the articular sensory branches of the obturator and femoral nerves - combined approach using fluoroscopy and ultrasound guidance: technical report, and observational study on safety and efficacy. Pain Physician 2018; 21: 279-84.











