Ramped versus sniffing position in the videolaryngoscopy-guided tracheal intubation of morbidly obese patients: a prospective randomized study
Article information
Abstract
Background
Ramped positioning is recommended for intubating obese patients undergoing direct laryngoscopy. However, whether the use of the ramped position can provide any benefit in videolaryngoscopy-guided intubation remains unclear. This study assessed intubation time using videolaryngoscopy in morbidly obese patients in the ramped versus sniffing positions.
Methods
This is a prospective randomized study in patients with morbid obesity (n = 82; body mass index [BMI] ≥ 35 kg/m2). Patients were randomly allocated to either the ramped or the standard sniffing position groups. During the induction of general anesthesia, difficulty in mask ventilation was assessed using the Warters scale. Tracheal intubation was performed using a C-MAC® D-Blade videolaryngoscope, and intubation difficulty was assessed using the intubation difficulty scale (IDS). The primary endpoint was the total intubation time calculated as the sum of the laryngoscopy and tube insertion times.
Results
The percentage of difficult mask ventilation (Warters scale ≥ 4) was significantly lower in the ramped (n = 40) than in the sniffing group (n = 41) (2.5% vs. 34.1%, P < 0.001). The percentage of easy intubation (IDS = 0) was significantly higher in the ramped than in the sniffing group (70.0% vs. 7.3%, P < 0.001). The total intubation time was significantly shorter in the ramped than in the sniffing group (22.5 ± 6.2 vs. 40.9 ± 9.0, P < 0.001).
Conclusions
Compared with the sniffing position, the ramped position reduced intubation time in morbidly obese patients and effectively facilitated both mask ventilation and tracheal intubation using videolaryngoscopy.
Introduction
With the worldwide increase in the prevalence of obesity, anesthesiologists are encountering an increasing number of obese patients in the operating room [1,2]. Although increased body mass index (BMI) itself poorly predicts difficult laryngoscopy [3–5], obese patients tend to have other predictors of difficult intubation, such as a large neck circumference [6,7]. Many studies have reported that laryngoscopy and tracheal intubation are more difficult to perform in obese patients than in lean patients [3,8,9].
For successful intubation under direct laryngoscopy, appropriate positioning is increasingly emphasized in obese patients [10,11]. Collins et al. [12] suggested placing morbidly obese patients in a ramped position rather than in the standard sniffing position. The ramped position is achieved by arranging blankets under the patient’s upper body and head to obtain a horizontal alignment between the external auditory meatus and sternal notch [13]. This position produces proper alignment of the oral, pharyngeal, and laryngeal axes (the three axes of intubation) in obese patients, similar to the sniffing position in lean patients. Subsequent studies have demonstrated that the ramped position significantly improved the laryngeal view in morbidly obese patients during direct laryngoscopy [14–16].
Videolaryngoscopy is another useful option for tracheal intubation in obese patients. A recent meta-analysis of 13 randomized controlled trials showed that videolaryngoscopy was superior to direct laryngoscopy in terms of intubation success rate, intubation time, and glottic visualization in obese patients [17]. Only four of these 13 trials described the use of the ramped position for intubation, while the others did not describe patient positioning or did not use the ramped position. Unlike direct laryngoscopy, videolaryngoscopy does not require eye alignment with the three axes of intubation to visualize the glottis and facilitate tracheal intubation [18]. Considering this advantage, it seems possible that the implementation of videolaryngoscopy could lead to successful intubation in obese patients, even without the use of the ramped position.
However, it remains unclear whether the use of the ramped position confers any benefit to videolaryngoscopy-guided intubation in obese patients. Therefore, this study was conducted to compare videolaryngoscopy-guided intubation of morbidly obese patients in the ramped versus sniffing position. The hypothesis of the study was that the intubation time in the ramped position might be shorter than that in the sniffing position. The primary outcome was intubation time (the time required for successful intubation); the secondary outcomes were difficulties in mask ventilation and intubation.
Materials and Methods
This prospective, randomized, parallel-group study was approved by the Institutional Review Board of the Chonnam National University Hospital (IRB no. 2019-361). The study has been registered at the Clinical Research Information Service of the Korea National Institute of Health (https://cris.nih.go.kr) under the registration number KCT0004589. The study was conducted in a university hospital between December 2019 and March 2021, in accordance with the principles of the 2013 Declaration of Helsinki. Written informed consent was obtained from all participants prior to enrollment.
This study enrolled patients with BMI ≥ 35 kg/m2, age 20–80 years, and an American Society of Anesthesiologists physical status classification of I–III who were scheduled to receive general anesthesia for surgery with orotracheal intubation. Patients with a history of difficult intubation, cervical spine defect, previous head and neck surgery, or risk of pulmonary aspiration were excluded. Preoperative airway evaluation was conducted the day before surgery and included Mallampati classification, neck circumference, sternomental distance, thyromental distance, and inter-incisor distance.
Patients were divided into two groups: a sniffing position group and a ramped position group. Position allocation was based on a computer-generated random number list with random block sizes of 2 and 4, which was prepared by an investigator with no clinical involvement in the trial. In the sniffing group, the patient was placed in the supine position with a 7-cm-high pillow placed under the occiput. For the ramped group, pillows were placed under the patient’s upper body and head such that the external auditory meatus and sternal notch were horizontal. The height of the operating table for patients in both groups was adjusted to ensure that the patient’s head was located between the anesthesiologist’s lower xiphoid process and the upper part of the umbilicus.
Upon arrival in the operating room, the patient was placed in the assigned position (sniffing or ramped position) with standard monitors, including for electrocardiogram, non-invasive blood pressure, pulse oximetry, and capnography. All patients were preoxygenated with 100% oxygen for 3 min, after which anesthesia was induced with propofol and remifentanil. After loss of consciousness, repetitive train-of-four (TOF) stimulation was started and rocuronium (0.6–1.0 mg/kg of ideal body weight) was administered.
The difficulty in manual mask ventilation was assessed using the Warters scale, which assigns points based on escalating levels of intervention to achieve a target tidal volume of 5 ml/kg of ideal body weight (Table 1) [19]. If the target tidal volume was not achieved, an airway device, increased inspiratory pressure, and two-person ventilation were used. The mask ventilation score was recorded when the TOF count reached zero. Difficult mask ventilation was defined as a score ≥ 4 on the Warters scale [20].
Tracheal intubation was performed using a C-MAC® D-Blade videolaryngoscope (Karl Storz, Germany) (Fig. 1). The videolaryngoscope blade has a large upward curvature at its distal end [21]. The internal diameter of the endotracheal tube was 8 mm for men and 7 mm for women; each stylet was pre-shaped to resemble the curvature of the C-MAC D-blade. All mask ventilation and tracheal intubation procedures were performed by a single faculty anesthesiologist who had experience in anesthesia for more than 10 years and was experienced with the use of the C-MAC D-blade videolaryngoscope.

The conventional C-MAC videolaryngoscope blade (Macintosh size 3, [A]) and the hyperangulated C-MAC D-blade (B).
The difficulty in tracheal intubation was assessed using the Intubation Difficulty Scale (IDS) [22]. The IDS score was derived from the sum of seven variables, which consisted of the number of intubation attempts, number of additional operators, number of alternative intubation techniques used, Cormack grade of laryngeal view, use of increased lifting force during laryngoscopy, application of external laryngeal pressure, and position of the vocal cord under laryngoscopic view. The degree of difficulty was categorized as easy (IDS = 0), slightly difficult (IDS = 1 to 5), moderate to major difficulty (IDS > 5), or impossible intubation (IDS = infinity) according to the IDS score.
Laryngoscopy and tube insertion times were measured separately to distinguish between difficult laryngoscopy and difficult tube insertion. Laryngoscopy time was measured from the time when the blade tip touched the patient’s lip until the best glottic view was achieved on the video laryngoscope monitor. Tube insertion time was measured from the time the endotracheal tube was inserted into the patient’s mouth until the passage of the tube through the glottis. The total intubation time was calculated as the sum of the laryngoscopy and tube insertion times. Intubation failure was defined as a total intubation time > 90 s or esophageal intubation.
Sample size was determined based on the mean intubation time estimated in a pilot study (n = 12 for each group), reporting a mean difference of 7.6 s and a standard deviation of 11.6 s. Power analysis showed that a sample size of 76 patients (38 patients in each group) would provide a statistical power of 0.8 with a two-sided level of 0.05 to detect significant differences. Considering possible dropouts, a total sample size of 82 patients was calculated.
The Kolmogorov–Smirnov test was performed to examine the assumption of normality. Normally distributed continuous variables were compared using the Student’s t-test; non-normally distributed continuous variables and ordinal variables were compared using the Mann–Whitney U test. Categorical variables were compared using the chi-square test or Fisher’s exact test. Data are presented as the number of patients, mean ± SD, or median (Q1, Q3). Statistical significance was set at P < 0.05.
Results
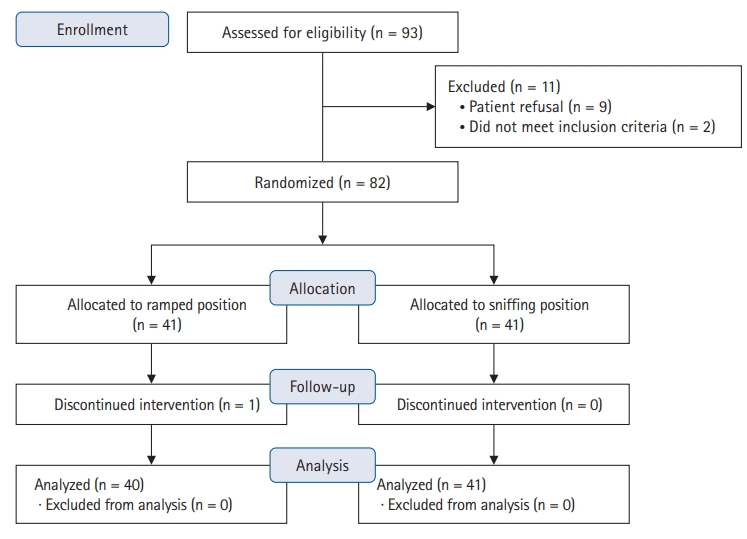
Among the 93 patients screened for eligibility, 11 were excluded for the reasons shown in Fig. 2. Eighty-two patients were randomized in the study, but one patient in the ramped group was excluded because the operation was canceled. Thus, the study population comprised of 81 patients (40 patients for the ramped group and 41 patients for the sniffing group). There were no significant differences in the demographic data and airway parameters between the two groups (Table 2).
The incidence of difficult mask ventilation was significantly lower in the ramped than in the sniffing group (2.5% vs. 34.1%, P < 0.001) (Table 3). The rate of easy intubation was significantly higher in the ramped than in the sniffing group (70.0% vs. 7.3%, P < 0.001). The rate of Cormack grade I was higher in the ramped than in the sniffing group (95.0% vs. 63.4%, P = 0.001), although poor visualization of the glottis (Cormack grade ≥ 3) under videolaryngoscopy was not observed in either group. Increased lifting force to expose the glottis during videolaryngoscopy was less frequent in the ramped than in the sniffing group (5.0% vs. 80.5%, P < 0.001). Neither group had failed mask ventilation or intubation.
The total intubation time, which was the primary outcome of the study was significantly shorter in the ramped than in the sniffing group (22.5 ± 6.2 vs. 40.9 ± 9.0 s; mean difference [95% CI] 18.4 [15.0, 21.8], P < 0.001) (Fig. 3). Two components of the total intubation time were also significantly shorter in the ramped than in the sniffing group, respectively (10.0 ± 2.7 vs. 18.9 ± 4.5 s for laryngoscopy time, P < 0.001; 12.5 ± 4.9 vs. 22.0 ± 7.3 s for tube insertion time, P < 0.001).
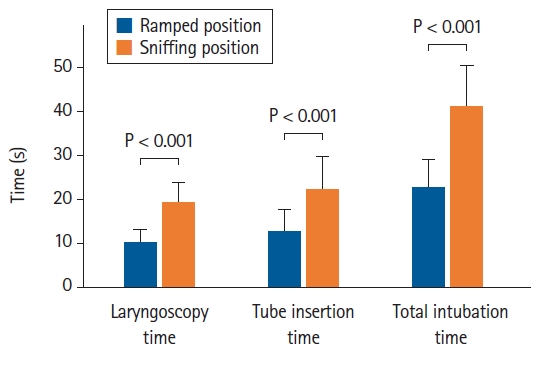
Comparison of laryngoscopy time, tube insertion time, and the total intubation time during videolaryngoscopy in the ramped versus sniffing position. Laryngoscopy time: from the insertion of the blade to the best glottic visualization, Tube insertion time: from the insertion of the endotracheal tube to the passage of the tube through the glottis, Total intubation time: laryngoscopy time + tube insertion time.
Discussion
In the present study, intubation time using a videolaryngoscope was compared between morbidly obese patients placed in the ramped versus the sniffing position. All intubations were completed successfully in both positions. However, the total intubation time was significantly shorter in the ramped than in the sniffing group. Laryngoscopy and tube insertion times (components of the total intubation time) were also shorter in the ramped group. Additionally, mask ventilation and tracheal intubation were easier in the ramped than in the sniffing group. These results suggest that despite the advantage conferred by videolaryngoscopy in all patients, the ramped position remains useful for tracheal intubation in obese patients.
The long laryngoscopy time of the patients in the sniffing position can be explained by the difficult insertion of the laryngoscope blade. During laryngoscope insertion into the oral cavity, the tip of the laryngoscope handle moves towards the patient’s chest. For morbidly obese patients in the sniffing position, laryngoscope insertion and manipulation are often impeded by the anterior expansion of the chest cavity, which results from increased fat deposition (Fig. 4). A similar problem frequently occurs in pregnant patients, in whom the use of a short laryngoscope handle has been clinically accepted because pregnancy-related breast enlargement could be an impediment to intubation with a standard laryngoscope handle [23].

Comparison of the difficulty of the videolaryngoscope blade insertion between the sniffing position (A) and the ramped position (B). In the sniffing position, laryngoscope insertion could be impeded by anterior expansion of the chest cavity in morbidly obese patients. In the ramped position, there might be more space for laryngoscope insertion and manipulation.
However, a short-handle design is not available for most videolaryngoscopes, including the C-MAC® D-Blade videolaryngoscope used in the present study. Furthermore, the C-MAC® D-Blade has a hyperangulation of 40°, in contrast to the 18° angulation of conventional C-MAC blades [21]. Hyperangulation may further increase the difficulty of blade insertion because the handle must be more sloped to allow the hyperangulated blade to enter the oral cavity [24]. For patients in the sniffing position, a longer laryngoscopy time may be required for additional manipulations, including 90° rotation of the handle to the right or blade orientation in the reverse direction [24,25]. In contrast, patient placement in the ramped position provides more space for conventional handling of the laryngoscope.
The tube insertion time was also significantly shorter in the ramped than in the sniffing group, although videolaryngoscopy provided adequate exposure of the glottis (Cormack grade 1 or 2) for all patients. This finding demonstrated that the tube tip movement toward the glottic opening and tube advancement into the trachea are easier when obese patients are placed in the ramped position.
One possible explanation for this finding is that the oropharyngeal airway may widen in the ramped position. Obese patients have a smaller upper airway cavity, which tends to collapse as fat accumulates in the upper respiratory tract and tongue [26–29]. A large amount of soft tissue around the neck may also affect upper-airway patency [30]. For non-obese patients, elevating the head from the table in the sniffing position produces an increased distance between the mentum and cervical column compared to the neutral position, resulting in a wider oropharyngeal airway [31]. For obese patients, however, this distance might not be increased adequately in the standard sniffing position because of their increased fat deposition in the back. The head is more elevated in the ramped position than in the sniffing position, which increases the distance between the mentum and the cervical column. Thus, the ramped position may provide wider space for tube advancement to the glottic opening. This mechanism is supported by the IDS score, which indicates a lower need for an abnormally increased lifting force during laryngoscopy in patients in the ramped position.
An alternative explanation for the difference in tube insertion time is the disparity between the view and the tracheal axes. During direct laryngoscopy, the view axis (the operator’s eye) and tracheal axis are generally similar if the three airway axes exhibit good alignment. During videolaryngoscopy, the view axis (with the camera at the distal tip of the blade) and tracheal axis usually form a large angle, especially if the airway axes are not aligned [32]. Increasing the angle between the blade and trachea can complicate tube advancement into the trachea, regardless of adequate laryngeal exposure during videolaryngoscopy [33–35]. For obese patients in the ramped position, this angle is probably smaller because the alignment of the airway axes is similar to that in normal-weight patients who are placed in the sniffing position.
Morbid obesity is an independent risk factor of difficult mask ventilation [36–38]. In the present study, the ramped position not only facilitated faster and easier tracheal intubation but also made mask ventilation easier in morbidly obese patients when compared with the sniffing position. This finding is consistent with a previous study by Cattano et al. [16], which showed that mask ventilation was easier in 35% of the patients upon shifting from the neutral position to the ramped position. Prolonged intubation time with difficult mask ventilation is expected to be more problematic in morbidly obese patients because the altered respiratory mechanics of these patients can lead to arterial desaturation even after a brief period of apnea, despite adequate preoxygenation [39–41]. Therefore, the present study suggests that morbidly obese patients need to be placed in the ramped position during the induction of anesthesia, regardless of whether videolaryngoscopy is used or not.
This study has several limitations. First, a crossover design was not used due to safety concerns. In anesthetized obese patients, multiple position changes and prolonged induction time with an unsecured airway increase the risk of positioning injury or hypoxemia. Second, the assessor could not be blinded due to the nature of interventions used in this study. Third, only one type of videolaryngoscope (with a hyperangulated blade) was used. Thus, caution is needed when generalizing these results to other videolaryngoscopes. Fourth, this was a single-center study, which may limit the applicability of the results to other institutions. Fifth, the time for intubation and the difficulty of intubation were significantly different between the groups in the present study. Thus, the incidence of complications related to tracheal intubation, such as postoperative sore throat or hoarseness, might be different between the groups. However, we did not collect data on the complications of tracheal intubation.
In conclusion, the present study demonstrated that the ramped position could reduce intubation time and achieve easy intubation using videolaryngoscopy in morbidly obese patients. Regardless of videolaryngoscopy usage, the ramped position should be considered to improve airway management in morbidly obese patients.
Acknowledgements
The authors thank all the patients who participated in the study and the research staff.
Notes
Funding
None.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author Contributions
Seongheon Lee (Formal analysis; Methodology; Writing – original draft)
Eun-A Jang (Investigation; Writing – review & editing)
Minjae Hong (Data curation; Investigation)
Hong-Beom Bae (Validation; Writing – review & editing)
Joungmin Kim (Conceptualization; Investigation; Writing – review & editing)