Video laryngoscope versus USB borescope-aided endotracheal intubation in adults with anticipated difficult airway: a prospective randomized controlled study
Article information
Abstract
Background
Video laryngoscopes are approved equipment for difficult airway intubations. The borescope, which was introduced during the coronavirus disease 2019 (COVID-19) era, is placed over a direct laryngoscope blade to provide an economical video laryngoscope. In the current study, we investigated the use of an endotracheal tube mounted over a USB borescope versus a video laryngoscope in patients with suspected difficult airways.
Methods
After obtaining informed consent, 120 adult patients with suspected difficult airways undergoing elective surgery were included in this study. Patients were randomized into the USB borescope and video laryngoscope groups. The primary outcome was time to successful intubation. The secondary outcomes included hemodynamic changes, anesthetist’s satisfaction, and the incidence of complications.
Results
Intubation time was comparable between the two groups (video laryngoscope: 30.63 s and borescope: 28.35 s; P = 0.166). However, the view was clearer (P = 0.026) and the incidence of fogging was lower (P = 0.015) with the video laryngoscope compared to the borescope. Conversely, anesthetist’s satisfaction frequency was higher with the borescope than with the video laryngoscope (P < 0.001).
Conclusions
The video laryngoscope provided a better view and less fogging with an intubation time that was comparable to that of the borescope; however, the higher cost of the video laryngoscope limits its availability. Therefore, the borescope is a low-cost, readily available device that can be used for intubating patients with potentially difficult airways.
Introduction
Securing the airway with endotracheal intubation has always been one of the most challenging aspects of anesthesia, with an incidence of failed intubation reaching up to six out of every 13,380 patients [1]. Airway difficulty can be assessed using various bedside tests, such as mouth opening, the Mallampati classification of oral opening [2], thyromental distance, and neck circumference [3], among others, including the El-Ganzouri risk index (mouth opening, thyromental distance, Mallampati class, neck movement, prognathism, weight, and history of difficult intubation) [4–6].
Various algorithms have been developed for difficult airway intubations. For example, the Difficult Airway Society algorithm uses a stepwise approach [7]. Difficult airway intubation equipment and skilled personnel should be available whenever difficulties are anticipated. This equipment can be as simple as different blade and tube sizes, stylets, bougies, and intubating laryngeal masks or as sophisticated as video laryngoscopes and fiberoptic bronchoscopes [8]. While the efficacy of video laryngoscope and fiberoptic bronchoscope in the management of challenging airways has been shown, their cost and bulky size limit their availability and the number of skilled personnel trained to use them [9,10]. Therefore, the need for an airway equipment that is available in every operating room to aid whenever unanticipated difficult intubation is encountered is always present.
The introduction of the video laryngoscope has changed how difficult airways are managed. Except for patients with limited mouth opening, for which the flexible fiberoptic bronchoscope is still superior, the video laryngoscope has replaced the fiberoptic bronchoscope for patients with anticipated and unanticipated difficult airways [11].
However, although it has been found to be cost-effective for organ inspection [12], the use of the USB borescope to confirm and aid in endotracheal intubation has only been studied in intubation simulator models and cadavers [13], and only a few case reports have suggested its applicability to confirm intubation [14].
In this study, the video laryngoscope was compared with the conventional laryngoscope aided by a USB borescope in the intubation of adult patients with suspected difficult airways. To our knowledge, this is the first randomized clinical trial to investigate this topic.
Materials and Methods
The institutional research ethics committee of Cairo University El-Kasr Alainy Hospital approved this study (IRB number: N-15-2021/MSC). The trial was registered at clinicaltrials.gov (reference number: NCT 05158088). The study was conducted from December 2021 to April 2022 in accordance with the Helsinki Declaration-2013. All patients who were screened and met the eligibility criteria were invited to participate in the trial, and all the enrolled patients provided written informed consent. Consent was requested from patients upon arrival to the operating suite for surgery or on the ward if they were admitted the night before surgery.
Patients
Patients with an El-Ganzouri score ≥ 4 [4] undergoing elective surgery under general anesthesia between October 2021 and March 2022 met the inclusion criteria. The exclusion criteria were as follows: presence of pulmonary diseases, uncontrolled hypertension, ischemic heart disease, cervical spinal fracture, limited mouth opening, tumors or polyps in the upper airway, and a history of difficult intubation, difficult bag-mask ventilation, or difficult bag-mask ventilation after induction of anesthesia.
Using a computer-generated table, patients were randomly allocated to either the video laryngoscope or the USB borescope group. Patient identifiers were attached to the opened envelopes and secured by a dedicated person, independent of the randomization proceedings. To account for potential dropouts, we recruited 120 patients (60 patients per group).
Procedures
Information on the age, sex, American Society of Anesthesiologists physical status, and body mass index were collecting during the pre-anesthetic visit by an anesthetist not involved in this study. The anesthetist also assessed the airway and measured the common predictive indices for difficult intubation (mouth opening, thyromental distance, modified Mallampati score, neck movement, prognathism, body weight, and history of difficult intubation) according to the El-Ganzouri Risk Index score for difficult intubation [3]. The intubations were performed by an anesthetist with at least one year of intubation experience, with prior experience using a video laryngoscope and at least two practice intubations on a manikin using a borescope.
After the patients arrived in the operating room, they were connected to standard monitoring devices (electrocardiogram, noninvasive blood pressure, and pulse oximetry). A baseline reading was taken, and they received O2 at 100% for at least 3 min using a face mask. Anesthesia induction consisted of intravenous fentanyl 1.5 µg/kg and propofol 2 mg/kg based on the estimated lean body weight. Manual mask ventilation and inflation of the lungs were attempted through a face mask using sevoflurane in O2 before the muscle relaxant was injected. Once the bag-mask ventilation was verified, atracurium 0.5 mg/kg was administered.
For patients allocated into the USB borescope group, a proper-sized endotracheal tube was placed over the USB borescope (T Takmly 5.5-HD, China semi-rigid waterproof borescope with an external diameter of 5.5 mm), with the tip of the borescope receding behind the tip of the endotracheal tube by approximately 1 cm, which was coated externally with a water-soluble sterile lubricant. A properly sized laryngoscope blade was inserted into the patient’s mouth using the operator’s left hand and advanced inward to the oropharynx while elevating the tongue. The USB borescope was placed into the oral cavity using the operator’s right hand and, while being tracked on a mobile phone, it was advanced to the glottic opening. If needed, the USB borescope was rotated and/or external laryngeal manipulation was performed to align it with the vocal cord. A properly sized endotracheal tube was then inserted (Supplementary Video 1).
For patients allocated into the video laryngoscope group, a video laryngoscope (Insighters Insight iS3, China) was placed, a properly size blade was then inserted, and the video laryngoscope gently was introduced, the epiglottis was lifted until the glottis opening was observed. A properly sized endotracheal tube was then inserted.
Correct placement of the endotracheal tube was further confirmed by the presence of an end-tidal carbon dioxide waveform and auscultation. Successful intubation attempts were defined as tracheal tube placement confirmed by a persistent end-tidal carbon dioxide waveform and auscultation of clear and equal bilateral breath sounds with an absence of air sounds over the epigastrium. The patients were then mechanically ventilated, with the end-tidal carbon dioxide levels maintained between 30 and 35 mmHg, and 1% isoflurane in oxygen maintained at 50%.
To ensure patient safety, a maximum of two intubation attempts were conducted. Intubation was considered a failure if desaturation (SpO2 90%) occurred or if the attempt took more than 90 s. In such cases, the attempted intubation was abandoned and bag-mask ventilation was reinitiated. An additional dose of propofol (0.5–1 mg/kg) was then administered and the insertion of a laryngeal mask was attempted. In the case of failure, fiberoptic intubation was then performed.
Complications associated with tracheal intubation, such as hypoxia (SpO2 < 92%), esophageal intubation, lip or dental injury, mucosal bleeding, and postoperative sore throat, were assessed in the anesthesia recovery area. A senior anesthetist who was not involved in the study performed these assessments.
The anesthetist’s overall satisfaction with the intubation experience was assessed and scored as good, satisfactory, or poor based on visualization of the glottis and the need for manipulations to aid in the intubation. The anesthetists also evaluated their overall experience with the video laryngoscope or borescope (3 for good, 2 for satisfactory, and 1 for poor overall experience). The intubation time was recorded as the time from the introduction of the laryngoscope into the oral cavity to the appearance of the end-tidal carbon dioxide waveform. Successful intubation on the first attempt, number of attempts, clarity of the view (Cormack-Lehane grade), presence of fogging during the procedure, and incidence of loss of airway (e.g., esophageal intubation), were noted. Heart rate (HR), systolic and diastolic blood pressure, mean arterial blood pressure (MAP), and SpO2 were documented before induction (baseline), immediately after induction, immediately after intubation, and 5 min after intubation.
Both the borescope and the video laryngoscope were disinfected using a gauze soaked in alcohol at a concentration of 70–90%. They were wiped for 5 min and then rinsed with saline.
Outcomes
The primary outcome was the time of intubation in seconds, assessed as the time from the introduction of the laryngoscope into the oral cavity to the appearance of the end-tidal carbon dioxide waveform.
The secondary outcomes included vital changes during and after intubation, clarity of the view, presence of fogging, incidence of complications, level of experience needed to handle the equipment (all had a minimum of one year of experience in anesthesia, having performed > 100 successful intubation procedures), number of attempts necessary for correct endotracheal intubation, and the anesthetists’ overall intubation experience.
Statistical analysis
In a previous study, the mean intubation time using a video laryngoscope was 77.43 ± 35.55 s. We calculated the sample size that could detect a mean difference of 25% between the study groups. MedCalc Software version 14 (MedCalc Software Bvba, Belgium) was used to calculate the sample size. A minimum of 106 patients (53 per group) were estimated to have a study power of 80% and an alpha error of 0.05. We increased the target number to 120 patients (60 per group) to account for possible dropouts.
All measurement indices were expressed as the mean ± SD or number (%). After the normality of the data distribution was analyzed, normally distributed data were compared using the independent sample t-test. Unpaired quantitative variables were evaluated using the Student’s t-test and analysis of variance. The Mann-Whitney U test was used for intergroup comparisons, and the Wilcoxon signed-rank test was used to compare different time points within the same group. Intergroup comparisons of categorical variables were performed using the chi-squared test. The P value was set at < 0.05. All data were statistically analyzed by statisticians using SPSS software (version 16.0; IBM Corp., USA).
Results
After written informed consent was obtained, 130 patients were initially screened for suitability and 120 who met the inclusion criteria were randomly assigned to the video laryngoscope and borescope groups. All enrolled patients were followed up successfully, and no patients were lost to follow-up. The Consolidated Standards of Reporting Trials (CONSORT) flow diagram for this trial is shown in Fig. 1.
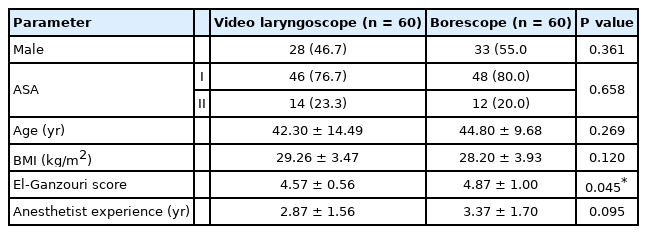
The patients’ demographic and operative data were comparable between the two groups (Table 1). The time of intubation (primary outcome) was also comparable between the two groups (P = 0.166).
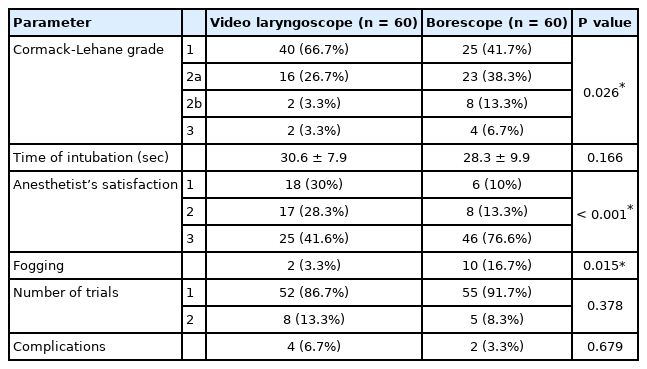
The view was clearer (Cormack-Lehane grade) with the video laryngoscope than with the borescope (P = 0.026). However, the anesthetist’s satisfaction with the intubation experience was better with the borescope than with the video laryngoscope, and there was a lower incidence of fogging with the video laryngoscope (P = 0.015). However, the incidence of complications, level of experience needed to handle the equipment, and number of trials to correct endotracheal intubation were comparable between the two groups (Table 2). There were no major adverse events related to the use of the intubation techniques in either group apart from mucosal bleeding (borescope group = 2 cases; video laryngoscope group = 4 cases) (P = 0.679), and there was no need for more advanced airway equipment, such as fiberoptic intubation, or intubation failure for any patient in the study.
The HR and MAP were comparable between the two groups except for the time immediately after intubation (P = 0.039) and 5 min after intubation (P = 0.021), where the HR was significantly higher in the video laryngoscope group than in the borescope group (Table 3).
Discussion
In the current study, the time of intubation between the video laryngoscope and borescope groups was not statistically significant. However, the Cormack-Lehane grade was statistically significantly better with the video laryngoscope, and there was a lower incidence of fogging. However, the number of trials and incidence of complications were not statistically significantly different between the groups. Considering how complex and expensive the video laryngoscope is, this lack of statistical significance provides favorable support for the borescope as an inexpensive and safe device to use for intubating patients with an anticipated difficult airway.
Previous studies assessing the effectiveness of the video laryngoscope in the intubation of patients with suspected difficult airways have shown a higher success rate with the video laryngoscope from the first attempt than with the direct laryngoscope, yet the intubation time was found to be longer, with an average of 46 s in the video laryngoscope group versus 33 s in the direct laryngoscope group [15]. In a Cochrane systematic review comparing video laryngoscopy and direct laryngoscopy, video laryngoscopy was found to result in a statistically significant reduction in the number of failed intubation trials in participants with an anticipated difficult airway (though not in those without an anticipated difficult airway), and the Cormack-Lehane view was better with the video laryngoscope. However, the review found insufficient data regarding the incidence of complications, such as hypoxia and laryngeal and airway trauma [16]. Additionally, with the video laryngoscope, reduced movement in the cervical spine has been reported during intubation of patients with an unsecured cervical spine [17].
There is an increasing need for intubation equipment, such as video laryngoscopes, that cause less particle dispersion and thus result in a lower incidence of airborne infections, especially in the coronavirus disease 2019 (COVID-19) era [18]. We believe that these benefits are anticipated with the borescope.
The use of the borescope started with the COVID-19 pandemic, and it has been tested and compared to the video laryngoscope in terms of the time to intubation. However, to the best of our knowledge, it has not been tested except in one study that was performed and tested on mannequins [19].
A previous case report has also shown that, given the direct visualization during intubation, the borescope could be used to confirm intubation when capnography fails to show any trace [14]. Other previous studies have shown that the borescope can be mounted over a direct laryngoscope to create a low-cost video laryngoscope [20,21]. In the current study, the tube was mounted over the borescope and a direct laryngoscope was used to lift the tongue, providing a better view and allowing for the tube to be manipulated to improve the view and confirm intubation above the carina level.
Although the view was clearer with the video laryngoscope, as evidenced by the lower incidence of fogging than with the borescope, anesthetists’ satisfaction was higher with the borescope than with the video laryngoscope. This could be explained by the advantages of the borescope over the video laryngoscope as an economical, pocket-sized device that requires no battery charging or sophisticated software. Moreover, the fact that the borescope (but not the video laryngoscope) can be navigated behind the vocal cords could increase the anesthetist’s confidence regarding correct endotracheal tube placement, in addition to the benefit of examining the airway until the tracheal carina.
One limitation of this study was the anesthetists’ initial unfamiliarity with the borescope. However, we overcame this by demonstrating the procedure and requiring the anesthetist to perform two trials on mannequins prior to the performing any intubations on patients. This led to better orientation with the borescope.
In conclusion, the video laryngoscope provided a better view and less fogging than the borescope with comparable intubation time; however, the high price associated with the video laryngoscope limits its availability. Therefore, the borescope is a low-cost, readily available device that can be used for intubating patients with potentially difficult airways. Further studies are needed to confirm the effectiveness of the borescope in other aspects of intubation in emergency settings.
Notes
Funding
This study was funded by the Department of Anesthesia, Surgical ICU, and Pain Management, Faculty of Medicine, Cairo University, Cairo, Egypt.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Mohamed Elshazly (Data curation; Investigation; Methodology; Project administration; Supervision; Writing – review & editing)
Mark Medhat (Conceptualization; Methodology; Writing – original draft)
Sahar Marzouk (Supervision; Writing – review & editing)
Enas M. Samir (Conceptualization; Writing – review & editing)
Supplementary Material
Supplemental Video 1.
A demonstrative video of endotracheal intubation using USB borescope.