Reading beyond quantitative electroencephalography-based indices: a case of erroneously high entropy values during ophthalmic surgery
Article information
The maintenance of an adequate depth of anesthesia (DoA) is important for patients undergoing general anesthesia. Quantitative electroencephalography (EEG) - based monitors, such as the bispectral (BIS) index and entropy, have been established to assess DoA. However, these measures can be affected by various factors, and the processed numerical output can often be misleading; therefore, quantitative EEG-based indices should be interpreted with caution. We report a case of a patient with abnormally high entropy values during ophthalmic surgery with no evidence of intraoperative awareness. Written informed consent was obtained.
A 61-year-old woman was scheduled for retinal detachment repair. Monitoring systems included electrocardiography, noninvasive blood pressure testing, pulse oximetry, end-tidal carbon dioxide, entropy (Entropy™ monitor; GE Healthcare, Finland), and neuromuscular transmission (E-NMT-01; GE Healthcare, Finland). General anesthesia was induced with intravenous injections of fentanyl (75 µg), lidocaine (100 mg), propofol using a target-controlled infusion system (Fresenius Orchestra Primea; Fresenius Kabi AG, Germany) to an effect-site concentration (Ce) of 4.0 µg/ml, and rocuronium (40 mg). General anesthesia was initially maintained with a propofol Ce of 3.0 µg/ml and rocuronium (20 mg/h). However, during the procedure, the entropy values were extremely high (response entropy [RE] > 90, state entropy [SE] between 80 and 90). The train-of-four count of the neuromuscular transmission monitor was 0. Since we assumed there was inadequate DoA, we titrated the propofol Ce to 3.5 µg/ml and administered sevoflurane at a minimal alveolar concentration of 0.5. However, even after titrating the anesthetic doses to deepen the DoA, the entropy values remained abnormally high even though there were no clinical signs of inadequate DoA, such as tachycardia or hypertension. Additionally, the raw EEG waveform changed from ‘fuzzy’ high frequency beta and gamma waves before anesthetic induction to the slow frequency waves of sleep spindles (Fig. 1) normally present during anesthesia maintenance. Meanwhile, the RE values were still > 90 and the SE values were between 80 and 90, even though the patient was unconscious according to the change in the raw EEG waveform. Since we were certain that the patient was adequately anesthetized, we discontinued the sevoflurane. The operation was completed uneventfully, and the patient recovered well with no memory of intraoperative awareness.
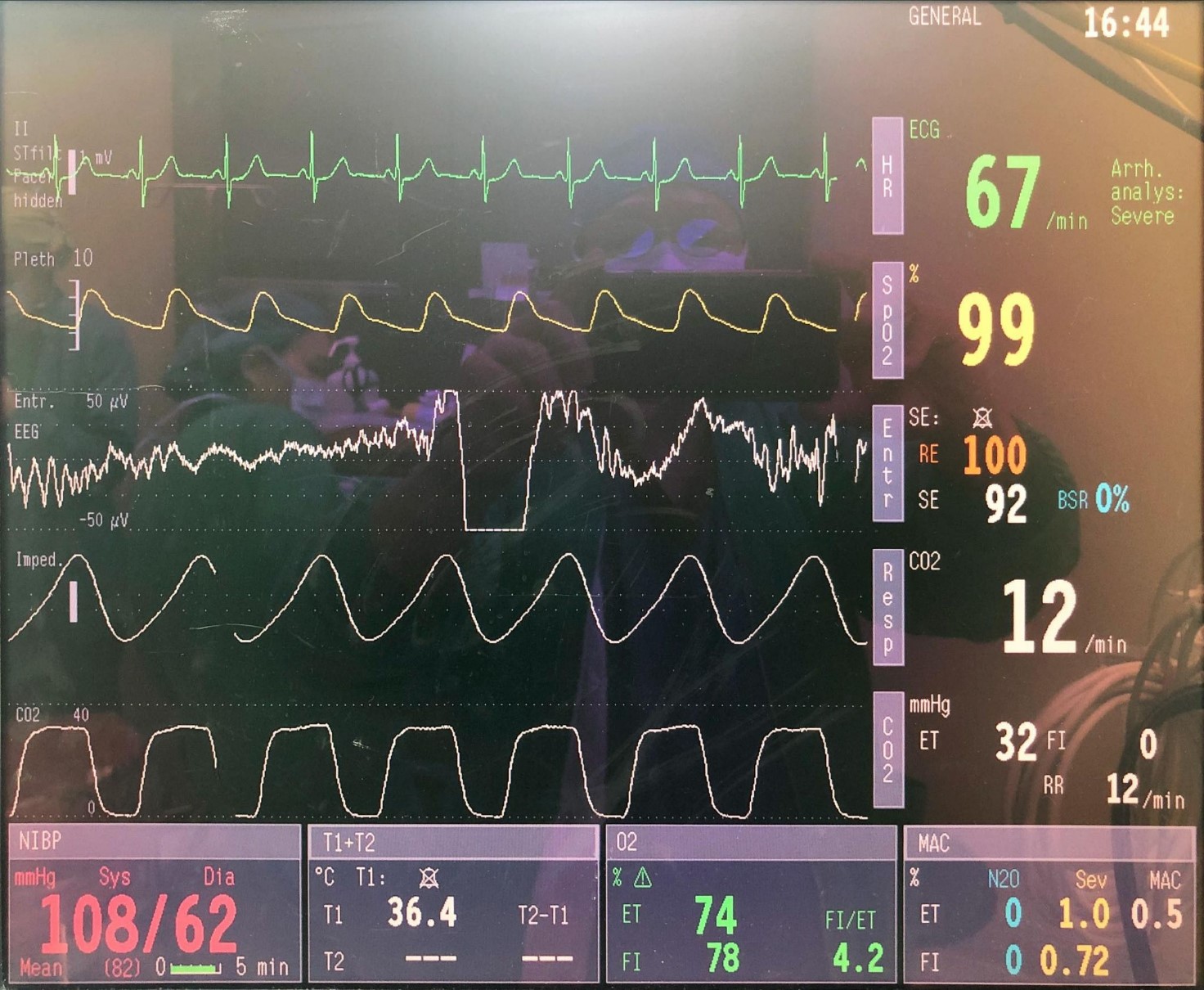
High RE and SE value. This case of a 61-year-old female patient undergoing detached retinal repair shows RE and SE values of 100 and 92, respectively; EEG waveforms showing sleep spindles throughout the trace with a consistent and repetitive slow wave background; and stable vital signs. RE: response entropy, SE: state entropy, EEG: electroencephalography.
This case study demonstrates the importance of examining raw EEG waves in real time rather than relying solely on quantitative EEG-derived indices. Despite the common use of quantitative EEG-based monitors for assessing DoA, the values shown on the monitors can potentially be misleading. For instance, in circumstances with elevated electrode impedance caused by erroneous placement or reduced adherence, the cause of the low-frequency electromyography signals can be misinterpreted as high-frequency EEG signals, iatrogenic movement of the limbs, interference from strong vibration-producing instruments or electrical equipment (such as electric scalpels, electrocautery, or thermal blankets), or a pathological EEG [1–3]. Hypothermia and hypoglycemia have also been found to alter EEG-based indices [3]. In addition, one EEG-based monitor will not necessarily perform the same as another model, and thus can influence the interpretation of the results [3].
Common causes of erroneously high entropy values during ophthalmic surgery include electrocautery, electro-oculography, and electromyographic activity. Alternatively, the surgeon’s hand on the patient’s frontal region, where the entropy sensing lead is placed, may affect electromyography readings and indirectly affect entropy values. However, throughout the reported operation, both RE and SE values remained > 80 despite temporarily ceasing electrocautery. Additionally, the difference between the RE and SE values remained < 8 and the train-of-four count of the neuromuscular transmission monitor was 0, indicating that neither electro-oculographic nor electromyographic activity was the cause of elevated entropy values in this case. All these measurements suggest that none of the common causes of falsely elevated entropy values during ophthalmic surgery were the culprit in this case. Moreover, the particular entropy monitor that was used was presumed to function normally, as no other patients had erroneous results with the model.
The algorithm used to calculate entropy is the mathematical normalization of the overall frequency range of values between 1 (maximum irregularity) and 0 (complete regularity). The theoretical assumption is that irregularities in the EEG signal decrease under anesthesia [1]. In our case, the EEG signals revealed random wavelengths and amplitudes from general anesthesia induction to emergence, which might have contributed to the erroneously high entropy values. On the other hand, 5–10% of the population has genetically determined EEG variants, meaning their EEG-based indices do not coincide with their clinical state of sedation, and are not associated with any actual cerebral dysfunction [3]. However, we were unable to determine whether our patient had a genetic EEG variant.
Since BIS and entropy values are calculated using different algorithms, BIS and entropy values that are concomitantly recorded may occasionally show discordant trends during general anesthesia. Aho et al. [4] reported that 11% of the concurrent pairs they analyzed had discrepancies between the BIS and entropy values. Pilge et al. [2] also reported more false classifications of the clinical state at transition with SE compared to the BIS index (14% vs. 9%). We do not intend to claim that one index is superior to the other; however, whenever a discrepancy exists between EEG-based indices and the actual clinical condition, the use of two concurrent monitoring devices with different EEG algorithms may allow for a more accurate assessment. In addition, as Akavipat et al. [5] have suggested that for neurosurgery, the postauricular placement of a BIS electrode can be a practical alternative to frontal lobe placement, we support the use of this modality during ophthalmic surgery.
While we are still uncertain of the factors that caused the erroneously high entropy values in this case, we cannot overemphasize the importance of interpreting the raw EEG waveform and considering the patient’s clinical condition rather than relying solely on quantitative EEG-based indices for assuming an inadequate DoA. We suggest that two EEG-based monitors with different algorithms be employed, since this may provide a more accurate assessment when numerical data are inconsistent with the clinical condition. Moreover, we recommend that, as a practical alternative, the EEG sensing electrode be placed at the posterior auricular position during ophthalmic surgery.
Notes
Funding
None.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Yuh-Shyan Wu (Writing – original draft)
Po-Nien Chen (Supervision)
Gwo-Ching Sun (Visualization)
Kuang-I Cheng (Conceptualization)
Zhi-Fu Wu (Writing – review & editing)
