 |
 |
| Korean J Anesthesiol > Volume 73(5); 2020 > Article |
|
Abstract
Rebound pain after regional anesthesia can be defined as transient acute postoperative pain that ensues following resolution of sensory blockade, and is clinically significant, either with regard to the intensity of pain or the impact on psychological well-being, quality of recovery, and activities of daily living. Current evidence suggests that it represents an unmasking of the expected nociceptive response in the absence of adequate systemic analgesia, rather than an exaggerated hyperalgesic phenomenon induced by local anesthetic neural blockade. In the majority of patients, it does not appear to significantly impact cumulative postoperative opioid consumption, quality of recovery, or patient satisfaction, and is not associated with longer-term sequelae such as persistent post-surgical pain. Nevertheless, it must be considered whenever regional anesthesia is incorporated into perioperative management. Strategies to mitigate the impact of rebound pain include routine prescribing of a systemic multimodal analgesic regimen, as well as patient education on appropriate expectations regarding block offset and expected surgical pain, and timely initiation of analgesic medication. Prolonging the duration of action of regional anesthesia with continuous catheter techniques or local anesthetic adjuncts may also help alleviate rebound pain, although further research is required to confirm this.
Regional anesthesia (RA) techniques have been shown to reduce perioperative opioid requirements [1], postoperative length of stay [2,3], and positively impact long-term outcomes such as the risk of persistent postsurgical pain (PPSP) [4], morbidity, and mortality [5]. RA is thus an important component of multimodal anesthetic and analgesic strategies. However, rebound pain after RA is increasingly recognized as an adverse effect [6] that can compromise analgesic benefit. This phenomenon is incompletely understood but appears more evident with RA techniques designed to provide surgical anesthesia or to otherwise completely abolish pain perception well into the early postoperative period; most commonly, single-injection peripheral nerve blockade (PNB) [2,7,8]. In this article we will provide an overview of our current understanding of rebound pain, discuss prevention strategies, and provide practical recommendations for the management of acute postoperative pain arising after the use of RA.
Several definitions of rebound pain have been published in the literature (Table 1). The essential characteristics of rebound pain are that it (1) is acute postoperative pain, (2) ensues following resolution of PNB, and (3) is clinically significant [9], either with regard to the intensity of pain or the impact on psychological well-being, quality of recovery, and activities of daily living. Rebound pain frequently occurs at night [10,11] but this is likely related to the 8 to 12 h duration of most single-injection PNB and the fact that most elective surgery is completed during daytime hours [12]. Rebound pain is also often described as ŌĆśburningŌĆÖ in nature [9] but lacks other neuropathic features such as allodynia. It often remains severe for 2ŌĆō6 h, but the subsequent pain trajectory is consistent with the expected recovery and healing process from the surgical insult. Rebound pain is therefore a transient phenomenon and distinct from PPSP [13].
A fundamental question is whether rebound pain merely represents an unmasking of the expected nociceptive response in the absence of adequate systemic analgesia, or if it reflects an exaggerated nociceptive response for which RA may be partially responsible. Hyperalgesia to heat stimuli has in fact been documented after PNB in animal studies. Subparaneural sciatic nerve blockade with ropivacaine in rats induced transient heat hyperalgesia of their hindpaws that lasted 5ŌĆō7 h after sensory block resolution [14]. Similar findings have been reported in subsequent animal studies [15,16]. However, the clinical significance of the intensity and duration of this hyperalgesic response is questionable. It is also unclear if these findings are generalizable to human subjects. As previously mentioned, although patients receiving PNB often describe the subsequent breakthrough pain as having ŌĆśburningŌĆÖ characteristics [9], this does not necessarily reflect the presence of heat hyperalgesia as described in animal studies [14ŌĆō16].
More importantly, hyperalgesia to heat stimuli occurs as a consequence of surgical trauma even in the absence of RA, and is part of a well-recognized spectrum of post-incisional primary hyperalgesia that can last up to 7 days after surgery [17]. Secondary hyperalgesia is a similar response that occurs in the uninjured tissue surrounding the site of trauma. This represents the general phenomenon of peripheral sensitization to pain that is a normal physiologic response [18]. Tissue injury initiates a local inflammatory cascade, and the various inflammatory mediators (e.g., calcitonin gene-related peptide, cyclooxygenase [COX]-1, COX-2, prostaglandins [PGE], cytokines, interleukines, neurotrophins) activate peripheral nociceptors both at the site of injury and in surrounding tissues [19].
RA, and more specifically PNB, prevents the perception of pain by blocking impulse propagation in peripheral nerves from tissue nociceptors to second-order neurons in the dorsal horn of the spinal cord, and onward via ascending pathways in the lateral spinothalamic tract and subsequent thalamocortical pathways in the brain. As a result, RA will inhibit central sensitization to pain that is upregulation of the activity and responsiveness of spinal dorsal horn neurons [17,20]. However, PNB will not have a significant effect on peripheral sensitization, and this inflammatory process will continue unabated in the absence of systemically-administered medications [18]. Therefore, as peripheral neural blockade resolves, the nociceptive input from the hyperalgesic area at the site of injury will become apparent as rebound pain. This distinction between the effect of RA on peripheral and central sensitization may also be responsible for the lack of any observed association between acute rebound pain and the subsequent development of PPSP.
Laboratory research in cellular and animal models has reported several effects of local anesthetic administration that may affect acute nociception. Mice receiving sciatic nerve block with bupivacaine had microscopic evidence of early-phase peripheral nerve injury secondary to Wallerian degeneration and axonal demyelination [21]. Local anesthetics have also been implicated in neurotoxicity [22,23] and cytotoxicity [24] via disruption of mitochondrial membrane potentials and release of cytochrome C, accompanied by activation of caspases ultimately leading to cell apoptosis [24,25]. Proinflammatory effects such as COX-2 gene expression and subsequent increases in PGE2 production at the surgical site, as well as in cerebrospinal fluid, have been documented after local infiltration [26] and intrathecal [27] administration of bupivacaine, respectively. However, pain resulting from structural damage to neural tissue would be expected to be more prolonged than is typical of rebound pain. The relevance of these experimentally-derived neurotoxic and proinflammatory effects of local anesthetics to the clinical application of RA is therefore currently uncertain.
In summary, it appears unlikely that RA contributes to postoperative hyperalgesia to any clinically significant extent, and consequently it can be assumed that rebound pain does not represent an exaggerated nociceptive physiological response.
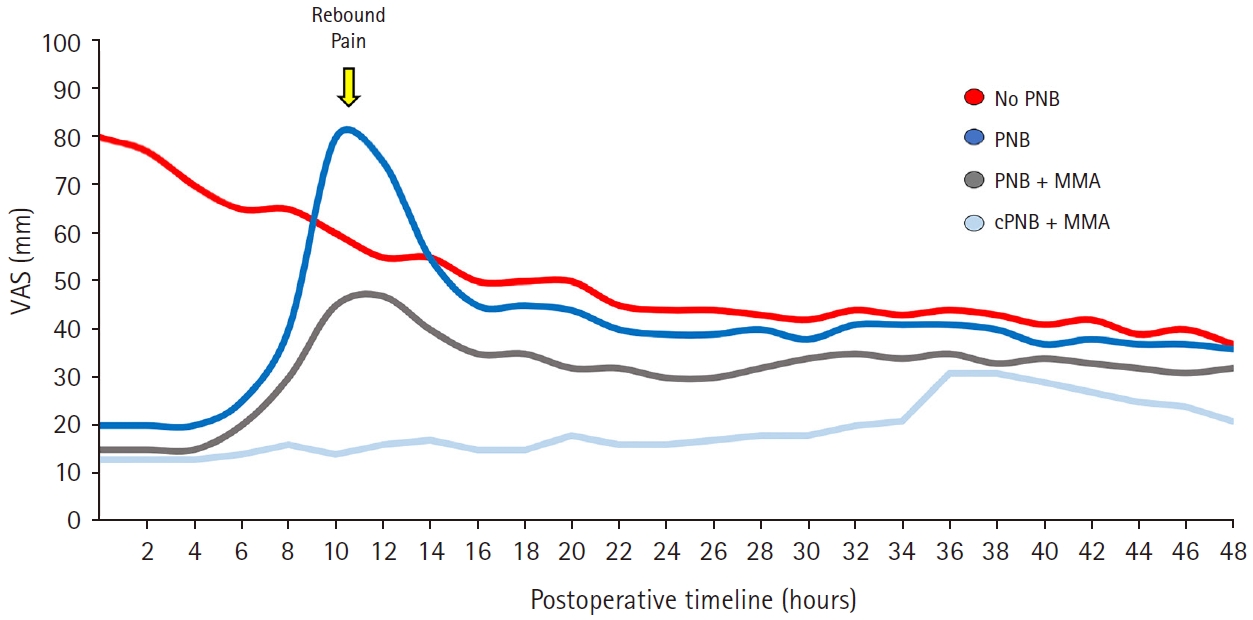
By definition, rebound pain is characterized by a delayed increase in patient-reported pain scores, often accompanied by increased analgesic consumption, that corresponds to the resolution of the analgesic effect of RA [28]. As discussed above, this does not necessarily reflect exaggerated hyperalgesia. It is instead largely related to the unexpected termination of conduction blockade and unmasking of the nociceptive response to surgery in the absence of adequate systemic analgesia [13,29]. This is in fact analogous to the situation in which a patient emerges from general anesthesia (GA) and abruptly becomes aware of wound pain ŌĆō initial pain scores on admission to the postoperative care unit (PACU) are often high, and then decline as the patient receives appropriate analgesic therapy. Thus, the difference in pain trajectories between patients who receive RA and those who do not is largely a function of the timing of unmasking of the underlying acute post-surgical pain (Fig. 1).
The important question, therefore, is not whether there is a delayed peak in reported pain scores and opioid consumption, but rather, what the relative height of this peak is compared to the pain experienced after GA alone, and what factors may influence this. This can be quite variable. For example, in comparing patients undergoing shoulder surgery with or without PNB, multiple studies have reported increased pain scores between 12 and 24 h after single-injection interscalene blocks with ropivacaine [2,7,10,30,31] that roughly corresponds to the expected resolution time for this block (Table 2). A 2015 meta-analysis reported a statistically significant difference in rest pain scores 24 h postoperatively in favor of the GA-only group, but the mean difference was only 0.96 on a 0ŌĆō10 visual analog scale and thus of limited clinical significance [32]. Furthermore, pain scores and opioid consumption were lower or similar in both groups at all other time points and patients who received an interscalene block were more satisfied with their analgesia at 24 h.
A more marked difference in rebound pain scores, as reported in other studies of supraclavicular [13] and infraclavicular brachial plexus block [13,29] as well as lower extremity RA techniques [3], may be at least partially explained by the postoperative analgesic regimen in place. Patients who do not undergo RA receive carefully titrated analgesic medication in the PACU to achieve satisfactory analgesia as a condition of discharge, and this is maintained thereafter with further doses as needed. In contrast, patients who have had effective RA usually require and receive little to no additional analgesics in PACU prior to discharge. Pain scores will naturally rise as the sensory block wears off and may reach or even exceed the levels experienced by GA-only patients at emergence, if they do not receive timely or appropriate doses of systemic multimodal analgesics. Patients who receive RA thus usually have significantly lower cumulative opioid consumption in the first 12 h postoperatively, and this difference becomes less marked (but not higher) in the 24ŌĆō48 h time period [32].
Balanced against this evidence for the occurrence of rebound pain are several studies that report the opposite results: compared to no block, single-injection PNBs (e.g., femoral [33,34] or combined axillary/suprascapular [12]) actually result in decreased pain scores even after the effect has worn off, and may also decrease primary and secondary hyperalgesia [35]. How do we account for these widely disparate findings? An individualŌĆÖs pain trajectory and experience are clearly dependent not only on the analgesic strategy utilized, but also on the type of surgery [36] and patient factors. Pain is ultimately a subjective experience that is influenced to varying degrees by biological, social, and psychological factors [37].
Cognitive and other higher-order cortical processes exert a powerful influence on the perception of acute pain. A cognitive bias [38] is a systematic pattern of deviation from rational judgment [39] that may lead to perceptual distortion. In the ŌĆścontrast effectŌĆÖ bias, a given stimulus is perceived as more intense when it is contrasted with a prior stimulus of lower intensity. The abrupt appearance of pain after a period of relative comfort, as the effect of a PNB wears off, can, therefore, cause a patient to rate the intensity of rebound pain higher than usual.
Patient expectations can also significantly influence pain perception [40ŌĆō42]. Cumulative evidence shows that subjects who have been primed to expect good pain relief subsequently exhibit decreased pain perception and associated cerebral activity in response to noxious stimulation ŌĆō a phenomenon known as placebo analgesia [43ŌĆō47]. However, if the expectation of low pain intensity is not met, the disappointment may instead bias them towards reporting higher pain scores. This is relevant as patients who receive a PNB are often advised that they can expect excellent postoperative analgesia [13]; however, the finite duration of the sensory block may not be sufficiently emphasized and thus they are unpleasantly surprised by the pain that is unmasked.
Poorly managed postoperative pain can result in adverse consequences including impaired quality of recovery, opioid dependence, PPSP, and increased medical costs [48]. It is therefore important to examine if rebound pain may have a significant impact on other health-related outcomes.
Despite the issue of rebound pain, the use of RA for outpatient surgery results in increased patient satisfaction stemming from the avoidance of GA, effective postoperative analgesia with reduced opioid requirements, and decreased incidence of postoperative nausea and vomiting [49]. In a detailed study that interviewed patients who received PNB for ankle fracture surgery, Henningsen et al. [9] confirmed that despite the presence of rebound pain, patients reported high levels of satisfaction with RA and a preference for a similar technique in the future. These findings are mirrored in other studies that find that even though patients describe increased pain scores after PNB resolution, satisfaction scores remain high and similar to the GA-only group [2,8,50]. It, therefore, appears that from the patientŌĆÖs perspective, rebound pain does not outweigh the early postoperative benefits of a pain-free interval [49], reduced opioid consumption and side-effects, superior recovery profile, and a shorter time to readiness for discharge [2].
Although poorly controlled acute postoperative pain has been implicated as a risk factor for the development of PPSP [51], there is no evidence to indicate that rebound pain per se predisposes to PPSP [13]. On the contrary, a recent Cochrane review reported that RA may instead reduce the incidence of PPSP after breast surgery and cesarean section [4]. As described above, the transitory nature of rebound pain, coupled with the early conduction block of nociceptive transmission, makes it unlikely that central sensitization will be exacerbated.
Rebound pain after RA has been implicated in higher rates of unanticipated health care resource utilization [13]. A retrospective study of 195 patients undergoing surgery for wrist fracture reported a higher incidence of unplanned physician visits (12% vs. 4%) because of severe pain in the first 48 h by those who received RA versus GA [13]. This may be partly explained by the fact that RA patients were far less likely to have received opioid and non-opioid analgesics prior to discharge, and there was no systematic patient education plan in place regarding post-discharge management of the postoperative transition from RA to systemic analgesia. A negative impact of RA (and the associated rebound pain) on healthcare utilization was not however borne out in a much larger retrospective study of over 59,000 patients undergoing outpatient shoulder surgery [52]. Patients who received a PNB, in fact, had a significantly lower rate of unplanned admissions, readmissions, or emergency department visits (9% vs. 12%) in the first seven postoperative days. Nevertheless, it is only logical that risk factors for rebound pain should be identified when performing RA for individual patients and strategies should be implemented to prevent and mitigate any potential impact on their postoperative recovery. This will be the focus of the remainder of this article.
The presence of preoperative pain [53] and younger age have been identified as patient risk factors for severe acute postoperative pain and PPSP [54]. Both of these have also been associated with a predisposition to rebound pain. Patients with pre-existing joint pain were more likely to report rebound pain following the use of PNB in total hip or knee arthroplasty [53]. Rebound pain following ankle fracture surgery with PNB as the primary anesthetic was also more common and more severe in patients under 60 years of age [55]. The mechanisms for this are incompletely understood, but include age-related differences in deep tissue (muscle) and superficial tissue (skin) nociception [56], increases in sensitivity of peripheral nerves to local anesthetics, and cationic acceptor site availability to local anesthetics [57], along with lower peripheral nerve conduction velocities in the elderly [58].
There is a perception that certain surgical procedures (e.g., shoulder, foot, and ankle) confer a higher risk of rebound pain. At present there is no data on the relative incidence of rebound pain among different surgeries; however, there are several logical contributing factors to consider. These include outpatient surgery, procedures associated with moderate-to-severe postoperative pain, and the use of single-injection PNBs (rather than continuous catheters) that provide near-complete analgesia [11,32]. Outpatient surgery patients are often discharged with a ŌĆśone size fits allŌĆÖ pain prescription that may be inadequate, and those who have received an effective single-injection PNB will usually have the first onset of breakthrough pain at home, where professional guidance and titration of analgesia is not available [13]. Patients often lack understanding of optimal medication dosing or timing and may also inappropriately limit the use of opioids at home because of fears of addiction or side-effects [13].
Rebound pain is a phenomenon that primarily manifests following PNB that provide dense sensory blockade (e.g., brachial plexus [2,7,10], popliteal sciatic [3,9] nerve blocks). Dramatic increases in pain scores and opioid consumption related to block offset are not usually seen in studies of fascial plane blocks such as transversus abdominis plane [59], pectoral nerves [60], erector spinae plane, [61] and quadratus lumborum [62,63] blocks. This requires further investigation for confirmation, but it may be related to factors that include a degree of visceral contribution to both pain and analgesic effect, an expectation of incomplete analgesic coverage by the block, and routine incorporation of these techniques into a multimodal analgesic regimen [64ŌĆō66].
Extending the duration of sensory blockade to allow more time for healing and subsidence of the inflammatory process, as well as a less precipitous offset of block, should mitigate the impact of rebound pain. It is therefore not surprising that continuous catheter RA techniques with an infusion of dilute local anesthetic for 48 h or longer will preserve all of the early postoperative benefits of single-injection PNB while largely abolishing the phenomenon of rebound pain. Salviz et al. [67] randomized patients undergoing outpatient arthroscopic rotator cuff repair to receive GA alone, or GA combined with either a single-injection or continuous interscalene block. Compared to the GA-only group, both RA groups had shorter PACU stays, were discharged home earlier, and had a longer interval to first analgesic use. Most notably, the incidence of severe pain (8ŌĆō10/10 on a numerical rating scale) on the first postoperative day was only 15% in the continuous interscalene block group, compared to 78% and 40% in the single-injection and GA-only groups respectively. By the second postoperative day, the single-injection and GA-only groups had similar pain profiles, but the continuous catheter group continued to exhibit lower pain scores with only 10% reporting severe pain compared to 35% in the other two groups. A similar effect was reported for continuous versus single-injection popliteal sciatic PNB in patients undergoing ankle fracture surgery. The peak in pain score trajectory was both delayed and attenuated in the continuous catheter group, and at 48 and 72 h postoperatively, pain scores were similar in both groups. However, the overall value of outpatient PNB catheters is controversial [68]. Continuous RA techniques are technically more challenging to perform, have an inherent failure rate [69], are time and labor-intensive to manage, and consequently are likely to remain under-utilized in this setting [68].
A more accessible alternative to continuous catheter techniques is the use of local anesthetic adjuncts to prolong the duration of single-injection PNBs. In a mouse model of sciatic nerve block with bupivacaine, the addition of perineural (but not intramuscular) dexamethasone prevented the appearance of a rebound hyperalgesic response to thermal stimulation [21]. Research indicates that perineural dexamethasone prevents bupivacaine-induced demyelination and Schwann cell degeneration [21], suggesting that any protective effect against rebound pain may be mediated by both anti-neurotoxic and anti-nociceptive mechanisms and effects. At present though, while it is well-established that dexamethasone (perineural more so than intravenous) [70] can prolong the analgesic benefit of PNB, there are no clinical studies specifically examining its impact on rebound pain per se.
Perineural buprenorphine is another local anesthetic adjunct used to prolong block duration, but again no studies have specifically investigated if it attenuates rebound pain compared to a control group. There is also a question of what constitutes an effective dose. In a retrospective cohort study describing their experience with a perineural combination of bupivacaine, clonidine, dexamethasone, and buprenorphine, Williams et al. [53] reported that a reduction in rebound pain after PNBs for total hip and knee arthroplasty was associated with > 300 ╬╝g buprenorphine but not lower doses.
Finally, although liposomal bupivacaine has been touted as an effective strategy to prolong the duration of analgesia (up to 72 h) with single-injection PNB [71], current evidence fails to support its routine use. Superior analgesia and opioid-sparing compared to conventional long-acting local anesthetics has not been demonstrated to date [72,73], and no studies have examined if it reduces the incidence and magnitude of rebound pain.
As discussed above, PNB only blocks the transmission of nociceptive input to the spinal cord and higher centers. Peripheral sensitization and other physiological responses mediated by the humoral inflammatory response to surgery remain unaffected. Combining RA with systemic multimodal analgesia is therefore recommended for the potential additive or even synergistic benefits [74ŌĆō76] in improving postoperative pain and related outcomes. Nevertheless, many studies investigating rebound pain after PNB do not routinely incorporate perioperative systemic multimodal analgesia, and outpatient surgery patients usually receive significantly less analgesic medication prior to discharge [13,29,77].
Although there is no direct evidence that a consistent and comprehensive multimodal analgesic regimen will reduce rebound pain, it should be prescribed on a routine basis as part of good clinical practice [3,11ŌĆō13,29,67,78]. This should include a combination of acetaminophen, non-steroidal anti-inflammatory drugs/COX-2 inhibitors, and oral opioids [28,53,67,79ŌĆō81], in the absence of any patient or surgical contraindications.
As already mentioned, patients and caregivers should be clearly informed about both the advantages and limitations of RA. Day surgery patients should receive preoperative education on the finite duration of analgesia provided by PNBs, and depending on the surgical procedure, should specifically be warned to expect moderate/severe pain commensurate with the surgical procedure as the block wears off. They should be instructed to begin taking analgesic medication earlier rather than later, with an emphasis on the 15ŌĆō20 min onset time for most oral analgesics versus the rapid offset of sensory block. A discussion of the expected interindividual variability [82] in block duration, pain thresholds, and response to analgesic therapy is also useful in assisting patients to self-titrate their medication. Supplementing verbal instructions with written or multimedia educational material will help improve compliance and lower perioperative anxiety and uncertainty [83].
Rebound pain is a transient perceptual phenomenon that occurs when the sensory blockade of RA resolves and unmasks ongoing nociceptive stimuli. Fortunately, in the majority of patients, it does not appear to significantly impact cumulative postoperative opioid consumption, quality of recovery, or patient satisfaction, and is not associated with longer-term sequelae such as PPSP. Rebound pain can, therefore, be viewed as a side-effect of RA but one that usually does not negate its favorable benefit-risk ratio. Nevertheless, rebound pain can cause acute distress and is an important consideration when formulating a perioperative management plan that involves RA, especially in outpatient surgery. Preoperative education is essential for setting appropriate patient expectations and coaching them on the importance of early preemptive initiation of systemic multimodal analgesia therapy. Prolonging the duration of action of PNB with continuous catheter techniques or with local anesthetic adjunctive medication may help alleviate rebound pain, although further research is required to confirm this.
NOTES
Author Contributions
Felipe Mu├▒oz-Leyva (Conceptualization; Data acquisition and analysis; Investigation; Methodology; Formal analysis; Writing ŌĆō original draft; Writing ŌĆō review & editing)
Javier Cubillos (Conceptualization; Validation; Visualization; Writing ŌĆō review & editing)
Ki Jinn Chin (Conceptualization; Supervision; Formal analysis; Validation; Writing ŌĆō review & editing)
Fig.┬Ā1.
Graph showing typical expected pain trajectories for the first 48 postoperative hours using four different strategies for acute pain management. Generally speaking, pain intensity is much lower in the immediate and early postoperative period in patients who receive a single-injection peripheral nerve block (PNB) or continuous peripheral nerve block (cPNB). Patients who do not receive a single-injection PNB may initially experience more pain, but this gradually decreases with administration of systemic analgesics and normal wound healing. As the effect of a single-injection PNB wears off, there can be an abrupt increase in pain intensity or ŌĆśrebound painŌĆÖ (yellow arrow). The magnitude and timing of this increase will vary depending on patient, surgery, and block-related factors. The magnitude of this rise can be attenuated if the PNB is complemented with optimal multimodal analgesia (MMA) initiated before its effect wears off. Compared to other strategies, effective cPNB plus MMA will also attenuate rebound pain and lower pain scores for as long as cPNB is continued. VAS: visual analogue scale for pain.
Table┬Ā1.
Proposed Definitions for Rebound Pain
| Author | Year | Definition |
|---|---|---|
| Williams et al. [28]. | 2007 | ŌĆśQuantifiable difference in pain scores when the block is working versus the increase in acute pain encountered during the first few hours after the effects of peri-neural single-injection or continuous infusion local anesthetics resolve.ŌĆÖ |
| Kolarczyk and Williams [14]. | 2011 | ŌĆśMechanical-surgical pain that results from the resolution of a nerve block with unopposed nociceptive input.ŌĆÖ |
| Galos et al. [29]. | 2016 | ŌĆśPoorly described entity, commonly defined as a dramatic increase in pain once regional anesthesia has dissipated.ŌĆÖ |
| LavandŌĆÖhomme [11]. | 2018 | ŌĆśMechanical ŌĆō surgical pain caused by unopposed nociceptive inputs that are uncovered after peripheral nerve blockade resolutionŌĆÖ |
| Dada et al. [6]. | 2019 | ŌĆśState of hyperalgesia with an onset between 8 and 24 h after block administration.ŌĆÖ |
Table┬Ā2.
Examples of Studies Reporting Increased Pain Scores and/or Increased Pain Medication Requirements after Resolution of Regional Anesthesia Techniques
| Reference | Type of surgery | PNB | Timing of block | Local anesthetic | Study design | Number of patients |
Rebound pain |
Observations/Limitations | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Increased pain scores* | Increased analgesic consumption* | Increased patient satisfaction with PNB | ||||||||
| Shoulder Surgery | ||||||||||
| ŌĆāDeMarco et al., 2011 [10] | Arthroscopic shoulder surgery | Interscalene (SS, analgesic) | Preincisional | Ropivacaine 0.5% | RCT | 53 | Yes | Yes | N/A | Postoperative continuous subacromial infusion with bupivacaine was used in all patients |
| ŌĆāHadzic et al., 2005 [2] | Open rotator cuff repair | Interscalene (SS, operative) | Preincisional | Ropivacaine 0.75% | RCT | 50 | Yes | Yes | YesŌĆĀ | Underpowered sample size for the determination of most purported disadvantages of PNB vs. GA (e.g., time required for PNB performance, PNB failure rates, or increased pain scores after PNB wears off) |
| ŌĆāKim et al., 2018 [7] | Arthroscopic rotator cuff reconstruction | Interscalene (SS or C, analgesic) | SS preincisional, C postincisional | Ropivacaine 0.75% + 2% Lidocaine | RCT | 154 | Yes | No | N/A | All groups had lower VAS pain scores at 24 h compared to baseline. No rebound pain in C group |
| ŌĆāLee et al., 2012 [30] | Arthroscopic rotator cuff reconstruction | Interscalene (SS, analgesic) | Preincisional | Mepivacaine 2% + Ropivacaine 0.75% | Non-randomized prospective trial | 61 | Yes | No | No | Non-randomized study. Large VAS fluctuations observed with ISB after hour 8 |
| ŌĆāLehmann et al., 2015 [8] | Arthroscopic shoulder surgery | Interscalene (SS operative or analgesic) | Preincisional | Mepivacaine 1% + Ropivacaine 0.375% | RCT | 120 | Yes | No | YesŌĆĀ | Included operative and analgesic PNBs |
| ŌĆāOh et al., 2007 [31] | Arthroscopic shoulder surgery | Interscalene (SS, analgesic) | Preincisional | Ropivacaine 0.25% | RCT | 84 | Yes | YesŌĆĀ | Yes | Lowest VAS rating at 16 h and 48 h after surgery was obtained only when combining ISB with LA instillation |
| ŌĆāSalviz et al., 2013 [67] | Arthroscopic rotator cuff reconstruction | Interscalene (SS or C, operative) | Preincisional | Ropivacaine 0.5% with/without infusion | RCT | 71 | Yes | Yes | N/A | Patients receiving GA without ISB may have already received an effective analgesic regimen through oral opioids immediately after surgery |
| ŌĆāPark et al., 2016 [12] | Arthroscopic rotator cuff reconstruction | Suprascapular +/- Axillary Nerve (SS, analgesic) | Preincisional | Ropivacaine 0.75% | RCT | 114 | YesŌĆĀ | N/A | N/A | All groups experienced increased pain scores at postoperative 12ŌĆō36 h |
| Distal Upper Limb | ||||||||||
| ŌĆāGalos et al., 2016 [29] | Distal radius fracture fixation | Infraclavicular (SS, operative) | Preincisional | Lidocaine 2% + 0.25% Bupivacaine | RCT | 40 | YesŌĆĀ | YesŌĆĀ | N/A | Greater dose of pain medication administered early in PACU in patients not receiving PNB |
| ŌĆāSunderland et al., 2016 [13] | Wrist fracture surgery | Supraclavicular/infraclavicular (SS, operative) | Preincisional | N/A | Retrospective cohort | 195 | YesŌĆĀ | N/A | N/A | Greater dose of pain medication administered in PACU in patients not receiving PNB. Non-statistical significance in unplanned resource utilization secondary to rebound pain |
| Lower Limb | ||||||||||
| ŌĆāGoldstein et al., 2012 [3] | Ankle fracture open reduction + internal fixation | Popliteal sciatic nerve block (SS, analgesic) | Preincisional | Bupivacaine 0.25% | RCT | 51 | YesŌĆĀ | N/A | N/A | Patients not receiving PNB experienced steady decrease in pain scores. Patients who received PNB had rebound pain between 12 and 24 h |
Local anesthetic details are shown for single-injection techniques. C: continuous, GA: general anesthesia, ISB: interscalene block, LA: local anesthetic, N/A: no data available, PACU: post anesthesia care unit, PNB: peripheral nerve block, RCT: randomized controlled trial, SS: single-shot or single-injection techniques, VAS: visual analogue scale.
References
1. Chan EY, Fransen M, Parker DA, Assam PN, Chua N. Femoral nerve blocks for acute postoperative pain after knee replacement surgery. Cochrane Database Syst Rev 2014; 2014: CD009941.



2. Hadzic A, Williams BA, Karaca PE, Hobeika P, Unis G, Dermksian J, et al. For outpatient rotator cuff surgery, nerve block anesthesia provides superior same-day recovery over general anesthesia. Anesthesiology 2005; 102: 1001-7.


3. Goldstein RY, Montero N, Jain SK, Egol KA, Tejwani NC. Efficacy of popliteal block in postoperative pain control after ankle fracture fixation. J Orthop Trauma 2012; 26: 557-62.


4. Weinstein EJ, Levene JL, Cohen MS, Andreae DA, Chao JY, Johnson M, et al. Local anaesthetics and regional anaesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children. Cochrane Database Syst Rev 2018; 4: CD007105.


5. Perlas A, Chan VW, Beattie S. Anesthesia technique and mortality after total hip or knee arthroplasty. Anesthesiology 2016; 125: 724-31.


6. Dada O, Zacarias AG, Ongaigui C, Echeverria-Villalobos M, Kushelev M, Bergese SD, et al. Does rebound pain after peripheral nerve block for orthopedic surgery impact postoperative analgesia and opioid consumption? A narrative review. Int J Environ Res Public Health 2019; 16: 3257.



7. Kim JH, Koh HJ, Kim DK, Lee HJ, Kwon KH, Lee KY, et al. Interscalene brachial plexus bolus block versus patient-controlled interscalene indwelling catheter analgesia for the first 48 hours after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 2018; 27: 1243-50.

8. Lehmann LJ, Loosen G, Weiss C, Schmittner MD. Interscalene plexus block versus general anaesthesia for shoulder surgery: a randomized controlled study. Eur J Orthop Surg Traumatol 2015; 25: 255-61.



9. Henningsen MJ, Sort R, M├Ėller AM, Herling SF. Peripheral nerve block in ankle fracture surgery: a qualitative study of patientsŌĆÖ experiences. Anaesthesia 2018; 73: 49-58.


10. Demarco JR, Componovo R, Barfield WR, Liles L, Nietert P. Efficacy of augmenting a subacromial continuous-infusion pump with a preoperative interscalene block in outpatient arthroscopic shoulder surgery: a prospective, randomized, blinded, and placebo-controlled study. Arthroscopy 2011; 27: 603-10.


11. LavandŌĆÖhomme P. Rebound pain after regional anesthesia in the ambulatory patient. Curr Opin Anaesthesiol 2018; 31: 679-84.


12. Park JY, Bang JY, Oh KS. Blind suprascapular and axillary nerve block for post-operative pain in arthroscopic rotator cuff surgery. Knee Surg Sports Traumatol Arthrosc 2016; 24: 3877-83.



13. Sunderland S, Yarnold CH, Head SJ, Osborn JA, Purssell A, Peel JK, et al. Regional versus general anesthesia and the incidence of unplanned health care resource utilization for postoperative pain after wrist fracture surgery: results from a retrospective quality improvement project. Reg Anesth Pain Med 2016; 41: 22-7.


14. Kolarczyk LM, Williams BA. Transient heat hyperalgesia during resolution of ropivacaine sciatic nerve block in the rat. Reg Anesth Pain Med 2011; 36: 220-4.



15. Brummett CM, Amodeo FS, Janda AM, Padda AK, Lydic R. Perineural dexmedetomidine provides an increased duration of analgesia to a thermal stimulus when compared with a systemic control in a rat sciatic nerve block. Reg Anesth Pain Med 2010; 35: 427-31.


16. Brummett CM, Padda AK, Amodeo FS, Welch KB, Lydic R. Perineural dexmedetomidine added to ropivacaine causes a dose-dependent increase in the duration of thermal antinociception in sciatic nerve block in rat. Anesthesiology 2009; 111: 1111-9.



17. Zahn PK, Brennan TJ. Primary and secondary hyperalgesia in a rat model for human postoperative pain. Anesthesiology 1999; 90: 863-72.


18. Pogatzki-Zahn EM, Segelcke D, Schug SA. Postoperative pain ŌĆö from mechanisms to treatment. Pain Rep 2017; 2: e588.



19. Arias JI, Aller MA, Arias J. Surgical inflammation: a pathophysiological rainbow. J Transl Med 2009; 7: 19.




20. Pogatzki EM, Gebhart GF, Brennan TJ. Characterization of Adelta- and C-fibers innervating the plantar rat hindpaw one day after an incision. J Neurophysiol 2002; 87: 721-31.


21. An K, Elkassabany NM, Liu J. Dexamethasone as adjuvant to bupivacaine prolongs the duration of thermal antinociception and prevents bupivacaine-induced rebound hyperalgesia via regional mechanism in a mouse sciatic nerve block model. PLoS One 2015; 10: e0123459.



22. Johnson ME. Neurotoxicity of lidocaine: implications for spinal anesthesia and neuroprotection. J Neurosurg Anesthesiol 2004; 16: 80-3.


23. Verlinde M, Hollmann MW, Stevens MF, Hermanns H, Werdehausen R, Lirk P. Local anesthetic-induced neurotoxicity. Int J Mol Sci 2016; 17: 339.



24. Perez-Castro R, Patel S, Garavito-Aguilar ZV, Rosenberg A, Recio-Pinto E, Zhang J, et al. Cytotoxicity of local anesthetics in human neuronal cells. Anesth Analg 2009; 108: 997-1007.


25. Chang YC, Hsu YC, Liu CL, Huang SY, Hu MC, Cheng SP. Local anesthetics induce apoptosis in human thyroid cancer cells through the mitogen-activated protein kinase pathway. PLoS One 2014; 9: e89563.



26. Gordon SM, Chuang BP, Wang XM, Hamza MA, Rowan JS, Brahim JS, et al. The differential effects of bupivacaine and lidocaine on prostaglandin E2 release, cyclooxygenase gene expression and pain in a clinical pain model. Anesth Analg 2008; 106: 321-7.


27. Kroin JS, Buvanendran A, Watts DE, Saha C, Tuman KJ. Upregulation of cerebrospinal fluid and peripheral prostaglandin E 2 in a rat postoperative pain model. Anesth Analg 2006; 103: 334-43.


28. Williams BA, Bottegal MT, Kentor ML, Irrgang JJ, Williams JP. Rebound pain scores as a function of femoral nerve block duration after anterior cruciate ligament reconstruction: retrospective analysis of a prospective, randomized clinical trial. Reg Anesth Pain Med 2007; 32: 186-92.



29. Galos DK, Taormina DP, Crespo A, Ding DY, Sapienza A, Jain S, et al. Does brachial plexus blockade result in improved pain scores after distal radius fracture fixation? A randomized trial. Clin Orthop Relat Res 2016; 474: 1247-54.




30. Lee SM, Park SE, Nam YS, Han SH, Lee KJ, Kwon MJ, et al. Analgesic effectiveness of nerve block in shoulder arthroscopy: comparison between interscalene, suprascapular and axillary nerve blocks. Knee Surg Sports Traumatol Arthrosc 2012; 20: 2573-8.



31. Oh JH, Kim WS, Kim JY, Gong HS, Rhee KY. Continuous intralesional infusion combined with interscalene block was effective for postoperative analgesia after arthroscopic shoulder surgery. J Shoulder Elbow Surg 2007; 16: 295-9.


32. Abdallah FW, Halpern SH, Aoyama K, Brull R. Will the real benefits of single-shot interscalene block please stand up? A systematic review and meta-analysis. Anesth Analg 2015; 120: 1114-29.


33. Williams BA, Kentor ML, Vogt MT, Irrgang JJ, Bottegal MT, West RV, et al. Reduction of verbal pain scores after anterior cruciate ligament reconstruction with 2-day continuous femoral nerve block: a randomized clinical trial. Anesthesiology 2006; 104: 315-27.


34. Youm YS, Cho SD, Cho HY, Hwang CH, Jung SH, Kim KH. Preemptive femoral nerve block could reduce the rebound pain after periarticular injection in total knee arthroplasty. J Arthroplasty 2016; 31: 1722-6.


35. Pedersen JL, Crawford ME, Dahl JB, Brennum J, Kehlet H. Effect of preemptive nerve block on inflammation and hyperalgesia after human thermal injury. Anesthesiology 1996; 84: 1020-6.


36. Mariano ER, El-Boghdadly K, Ilfeld BM. Using postoperative pain trajectories to define the role of regional analgesia in personalised pain medicine. Anesthesiology 2020 Advance Access published on May 5, 2020. doi: 10.1111/anae.15067

37. Gatchel RJ. Comorbidity of chronic pain and mental health disorders: the biopsychosocial perspective. Am Psychol 2004; 59: 795-805.



38. Korteling JE, Brouwer AM, Toet A. A neural network framework for cognitive bias. Front Psychol 2018; 9: 1561.



39. Haselton MG, Nettle D, Andrews PW. The evolution of cognitive bias. Edited by Buss DM: Hoboken, John Wiley & Sons, Inc. 2015, pp 724-46.
40. Wiech K. Deconstructing the sensation of pain: the influence of cognitive processes on pain perception. Science 2016; 354: 584-7.


41. Shih YW, Tsai HY, Lin FS, Lin YH, Chiang CY, Lu ZL, et al. Effects of positive and negative expectations on human pain perception engage separate but interrelated and dependently regulated cerebral mechanisms. J Neurosci 2019; 39: 1261-74.



42. Freeman S, Yu R, Egorova N, Chen X, Kirsch I, Claggett B, et al. Distinct neural representations of placebo and nocebo effects. Neuroimage 2015; 112: 197-207.



43. Wager TD, Rilling JK, Smith EE, Sokolik A, Casey KL, Davidson RJ, et al. Placebo-induced changes in fMRI in the anticipation and experience of pain. Science 2004; 303: 1162-7.


44. Wager TD, Atlas LY. The neuroscience of placebo effects: connecting context, learning and health. Nat Rev Neurosci 2015; 16: 403-18.




45. Watson A, El-Deredy W, Vogt BA, Jones AK. Placebo analgesia is not due to compliance or habituation: EEG and behavioural evidence. Neuroreport 2007; 18: 771-5.


46. Tracey I. Getting the pain you expect: mechanisms of placebo, nocebo and reappraisal effects in humans. Nat Med 2010; 16: 1277-83.



47. B├╝chel C, Geuter S, Sprenger C, Eippert F. Placebo analgesia: a predictive coding perspective. Neuron 2014; 81: 1223-39.


48. Tan M, Law LS, Gan TJ. Optimizing pain management to facilitate enhanced recovery after surgery pathways. Can J Anaesth 2015; 62: 203-18.



49. Liu SS, Strodtbeck WM, Richman JM, Wu CL. A comparison of regional versus general anesthesia for ambulatory anesthesia: a meta-analysis of randomized controlled trials. Anesth Analg 2005; 101: 1634-42.


50. Gurger M, Ozer AB. A comparison of continuous interscalene block versus general anesthesia alone on the functional outcomes of the patients undergoing arthroscopic rotator cuff repair. Eur J Orthop Surg Traumatol 2019; 29: 1659-66.



51. Fregoso G, Wang A, Tseng K, Wang J. Transition from acute to chronic pain: evaluating risk for chronic postsurgical pain. Pain Physician 2019; 22: 479-88.

52. Hamilton GM, Ramlogan R, Lui A, McCartney CJ, Abdallah F, McVicar J, et al. Peripheral nerve blocks for ambulatory shoulder surgery: a population-based cohort study of outcomes and resource utilization. Anesthesiology 2019; 131: 1254-63.


53. Williams BA, Ibinson JW, Mangione MP, Modrak RT, Tonarelli EJ, Rakesh H, et al. Research priorities regarding multimodal peripheral nerve blocks for postoperative analgesia and anesthesia based on hospital quality data extracted from over 1,300 cases (2011-2014). Pain Med 2015; 16: 7-12.



54. Gerbershagen HJ, Pogatzki-Zahn E, Aduckathil S, Peelen LM, Kappen TH, van Wijck AJ, et al. Procedure specific risk factors for the development of severe postoperative pain. Anesthesiology 2014; 120: 1237-45.


55. Sort R, Brorson S, G├Čgenur I, Nielsen JK, M├Ėller AM. Rebound pain following peripheral nerve block anaesthesia in acute ankle fracture surgery: an exploratory pilot study. Acta Anaesthesiol Scand 2019; 63: 396-402.


56. Lautenbacher S, Kunz M, Strate P, Nielsen J, Arendt-Nielsen L. Age effects on pain thresholds, temporal summation and spatial summation of heat and pressure pain. Pain 2005; 115: 410-8.


57. Tsui BC, Wagner A, Finucane B. Regional anaesthesia in the elderly: a clinical guide. Drugs Aging 2004; 21: 895-910.


58. Verd├║ E, Ceballos D, Vilches JJ, Navarro X. Influence of aging on peripheral nerve function and regeneration. J Peripher Nerv Syst 2000; 5: 191-208.


59. Baeriswyl M, Zeiter F, Piubellini D, Kirkham KR, Albrecht E. The analgesic efficacy of transverse abdominis plane block versus epidural analgesia. Medicine (Baltimore) 2018; 97: e11261.



60. Versyck B, van Geffen GJ, Chin KJ. Analgesic efficacy of the Pecs II block: a systematic review and meta-analysis. Anaesthesia 2019; 74: 663-73.


61. Abu Elyazed MM, Mostafa SF, Abdelghany MS, Eid GM. Ultrasound-guided erector spinae plane block in patients undergoing open epigastric hernia repair: a prospective randomized controlled study. Anesth Analg 2019; 129: 235-40.


62. Xu M, Tang Y, Wang J, Yang J. Quadratus lumborum block for postoperative analgesia after cesarean delivery: a systematic review and meta-analysis. Int J Obstet Anesth 2020; 42: 87-98.


63. Jin Z, Liu J, Li R, Gan TJ, He Y, Lin J. Single injection quadratus lumborum block for postoperative analgesia in adult surgical population: a systematic review and meta-analysis. J Clin Anesth 2020; 62: 109715.


64. Akerman M, Pej─Źi─ć N, Veli─Źkovi─ć I. A review of the quadratus lumborum block and ERAS. Front Med 2018; 5: 44.

65. Pirrera B, Alagna V, Lucchi A, Berti P, Gabbianelli C, Martorelli G, et al. Transversus abdominis plane (TAP) block versus thoracic epidural analgesia (TEA) in laparoscopic colon surgery in the ERAS program. Surg Endosc 2018; 32: 376-82.



66. Kim AJ, Yong RJ, Urman RD. The role of transversus abdominis plane blocks in enhanced recovery after surgery pathways for open and laparoscopic colorectal surgery. J Laparoendosc Adv Surg Tech A 2017; 27: 909-14.


67. Salviz EA, Xu D, Frulla A, Kwofie K, Shastri U, Chen J, et al. Continuous interscalene block in patients having outpatient rotator cuff repair surgery: a prospective randomized trial. Anesth Analg 2013; 117: 1485-92.


68. Pawa A, Devlin AP, Kochhar A. Interscalene catheters - should we give them the cold shoulder? Anaesthesia 2016; 71: 359-62.


69. Hauritz RW, Hannig KE, Balocco AL, Peeters G, Hadzic A, B├Ėrglum J, et al. Peripheral nerve catheters: a critical review of the efficacy. Best Pract Res Clin Anaesthesiol 2019; 33: 325-39.


70. Heesen M, Klimek M, Imberger G, Hoeks SE, Rossaint R, Straube S. Co-administration of dexamethasone with peripheral nerve block: intravenous vs perineural application: systematic review, meta-analysis, meta-regression and trial-sequential analysis. Br J Anaesth 2018; 120: 212-27.


71. Lambrechts M, OŌĆÖBrien MJ, Savoie FH, You Z. Liposomal extended-release bupivacaine for postsurgical analgesia. Patient Prefer Adherence 2013; 7: 885-90.


72. Abildgaard JT, Chung AS, Tokish JM, Hattrup SJ. Clinical efficacy of liposomal bupivacaine: a systematic review of prospective, randomized controlled trials in orthopaedic surgery. JBJS Rev 2019; 7: e8.


73. Hamilton TW, Athanassoglou V, Trivella M, Strickland LH, Mellon S, Murray D, et al. Liposomal bupivacaine peripheral nerve block for the management of postoperative pain. Cochrane Database Syst Rev 2016; 2016: CD011476.



74. Brown EN, Pavone KJ, Naranjo M. Multimodal general anesthesia: theory and practice. Anesth Analg 2018; 127: 1246-58.



75. Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg 2017; 152: 691-7.


76. Rosero EB, Joshi GP. Preemptive, preventive, multimodal analgesia: what do they really mean? Plast Reconstr Surg 2014; 134: 85S-93S.


77. Rundgren J, Mellstrand Navarro C, Ponzer S, Regberg A, Serenius S, Enocson A. Regional or general anesthesia in the surgical treatment of distal radial fractures: a randomized clinical trial. J Bone Joint Surg Am 2019; 101: 1168-76.


78. Toma O, Persoons B, Pogatzki-Zahn E, Van de Velde M, Joshi GP, Schug S, et al. PROSPECT guideline for rotator cuff repair surgery: systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia 2019; 74: 1320-31.



79. Chou R, Gordon DB, De Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of AnesthesiologistsŌĆÖ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain 2016; 17: 131-57.


80. Stiglitz Y, Gosselin O, Sedaghatian J, Sirveaux F, Mol├® D. Pain after shoulder arthroscopy: a prospective study on 231 cases. Orthop Traumatol Surg Res 2011; 97: 260-6.


81. Trompeter A, Camilleri G, Narang K, Hauf W, Venn R. Analgesia requirements after interscalene block for shoulder arthroscopy: the 5 days following surgery. Arch Orthop Trauma Surg 2010; 130: 417-21.












