Effect of anesthetic method on incidence of delirium after total hip replacement arthroplasty in South Korea: a population-based study using National Health Insurance claims data
Article information
Abstract
Background
There are various reports on the effects of the anesthetic method on neurologic complications. A population-based study was conducted to estimate the effect of anesthetic method on the incidence of postoperative delirium in patients that underwent total hip replacement arthroplasty in South Korea.
Methods
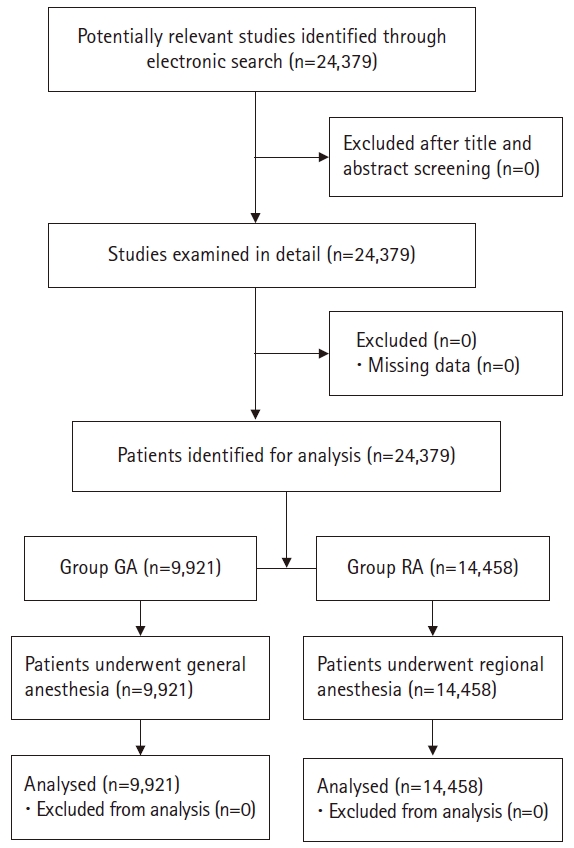
The Korean National Health Insurance claims database was used to retrospectively identify and analyze 24,379 cases of total hip replacement arthroplasty, defined as patients having a claim record with the operation code ‘N0711,’ from January 2008 to December 2017. Patients were divided into two groups, a general anesthesia group (n = 9,921) and a regional anesthesia group (n = 14,458). The incidence of delirium was assessed in cases when patients used medications for delirium, such as haloperidol, chlorpromazine, olanzapine, and risperidone.
Results
Of the 9,921 patients receiving general anesthesia and 14,458 receiving regional anesthesia, 142 (1.43%) and 209 (0.86%) experienced postoperative delirium after total hip replacement arthroplasty, respectively. There was no significant difference between the groups (P = 0.92). In logistic regression analysis, sex (P = 0.038) and patients with acquired immune deficiency syndrome (P = 0.008) were predictors of postoperative delirium.
Conclusions
Our results revealed that the anesthetic method was not associated with the incidence of postoperative delirium. In addition, the results suggest that male patients and patients with acquired immune deficiency syndrome undergoing total hip replacement arthroplasty carefully managed for postoperative delirium after surgery.
Introduction
Delirium is a complex syndrome that affects 7% to 65% of patients after hip-fracture surgery [1-3]. Patients with postoperative delirium have been independently associated with adverse clinical and economic outcomes such as death, decreased functional outcome, and cognitive decline, as well as higher cost of care and longer hospitalization. Therefore, it is important to characterize perioperative risk factors related to the incidence of postoperative delirium and to optimize the quality of care in patients with total hip replacement arthroplasty (THRA).
There have been various reports on the perioperative risk factors of postoperative delirium. The pathogenesis of postoperative delirium is unclear and probably multifactorial. Postoperative hypoxemia, postoperative restorations, metabolic and electrolyte anomalies, and sleep disturbances have been thought to be possible causes, as well as the use of certain drugs such as opioids, anesthetics, anticholinergics, benzodiazepine, antiparkinsonian drugs, and tranquillizers. Mental dysfunction on the third postoperative day and mean SpO2 on the second postoperative night have also been shown to significantly correlate with postoperative delirium [4].
In particular, there is controversy about the effects of general anesthesia (GA) and regional anesthesia (RA) on the incidence of postoperative delirium after THRA. Elderly patients that received general anesthesia displayed more frequent cognitive impairment during the immediate postoperative period compared with those who received regional anesthesia [5]. The mean score of the Mini-Mental State Examination (MMSE) decreased significantly only in patients who received general anesthesia. According to other reports, however, the use of neuraxial anesthesia during surgery did not reduce the incidence of postoperative cognitive dysfunction compared with general anesthesia [6,7]. Even in elderly patients, there was no significant difference in the incidence of cognitive dysfunction three months after the use of either general or regional anesthesia [8].
Therefore, a population-based study was conducted to investigate the effect of anesthetic method on the incidence of postoperative delirium in patients that underwent THRA in South Korea.
Materials and Methods
This study was approved by the Institutional Review Board of our institution (04-2018-015). We retrospectively extracted claim records from The Korean National Health Insurance (NHI) claims database that included the operation code ‘N0711’ and excluded patients who received more than one anesthesia dose (general anesthesia: ‘L1211,’ ‘L1221,’ or regional anesthesia: ‘L1213,’ ‘L1214,’ ‘L1223,’ ‘L1224’), received multiple surgeries with anesthesia, had multiple traumas and fractures (‘S00–S70,’ ‘S73–99,’ ‘T07,’ ‘T14’), or underwent two or more surgeries within the same hospital stay. A total of 24,379 patient cases from January 2008 to December 2017 were extracted.
Baseline characteristics, surgery, disease, and mortality data of the subjects included in the Korean NHI claims database were extracted. Patients were divided into two groups, patients receiving general anesthesia (‘L1211,’ ‘L1221;’ GA group; n = 9,921) and patients receiving regional anesthesia (‘L1213,’ ‘L1214,’ ‘L1223,’ ‘L1224;’ RA group; n = 14,458).
Patients with hypertension were defined by disease code ‘I10–I15’ and patients with diabetes were defined by disease code ‘E10–E14.’ Patients with cardiac disease, including patients with heart failure, were defined by disease code ‘I50,’ patients with cardiovascular disease were defined by specific disease code ‘V192,’ and patients with ischemic heart diseases were defined by disease code ‘I20–I25.’ Patients with respiratory diseases, including patients with chronic pulmonary disease, were defined by disease code ‘J44’ and patients with asthma were defined by disease code ‘J45.’ Patients with Parkinson’s disease were defined by disease code ‘G20–G21’ and patients with mental and behavioral disorder (mood) were defined by disease code ‘F30–34, F38, F39.’ The patient’s disease associated with Charlson comorbidity index was evaluated [9-15].
The diagnosis of patients undergoing THRA was classified into six categories: necrosis with disease code ‘M187,’ unspecified hip arthropathy with disease code ‘M16,’ femur fracture with disease code ‘S72,’ other arthropathy with disease code ‘M19,’ other arthritis with disease code ‘M13.’ and etc.
The incidence of delirium was assessed in cases when diagnosis codes ‘F05.8,’ ‘F05.9,’ ‘F05,’ or ‘F05.0’ were newly added after the operation, or when patients used delirium medications such as haloperidol, chlorpromazine, olanzapine, and risperidone.
Statistical analysis
Data were expressed as mean ± standard deviation, median (25 to 75 percentile), or number of patients (%). The normality test was performed with Shapiro-Wilk W test or Kolmogorov-Smirnov. Baseline and peri-operative characteristics and variables for postoperative outcomes were compared using the independent t-test or the Wilcoxon rank-sum test for continuous variables and the χ2 test or Fisher’s exact test for categorical variables. To identify factors significantly predictive of postoperative delirium, univariate and multivariate logistic regression analyses were performed. All statistical analyses were conducted using SAS® ver. 9.4 (SAS Institute, USA). A P value < 0.05 was considered statistically significant.
Results
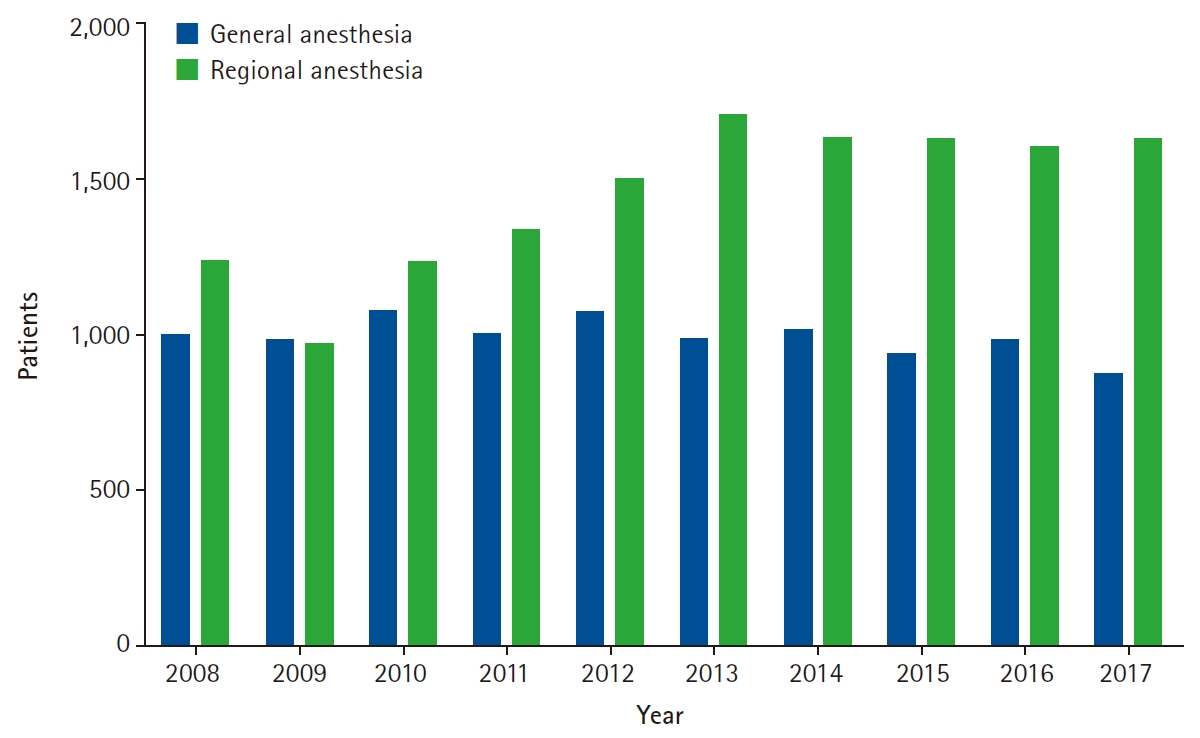
A total of 24,379 cases of patients undergoing THRA were extracted from the NHI claims database, as shown in Fig. 1. The total number of patients undergoing THRA increased annually, and since 2011, patients were approximately 1.5 times more likely to undergo THRA under regional anesthesia than general anesthesia (Fig. 2, P < 0.05). Among the patients undergoing THRA, 1,521 (15.33%) of the patients who received general anesthesia and 2,548 (17.61%) of the patients who received regional anesthesia were aged 65 years and older (Fig. 3).
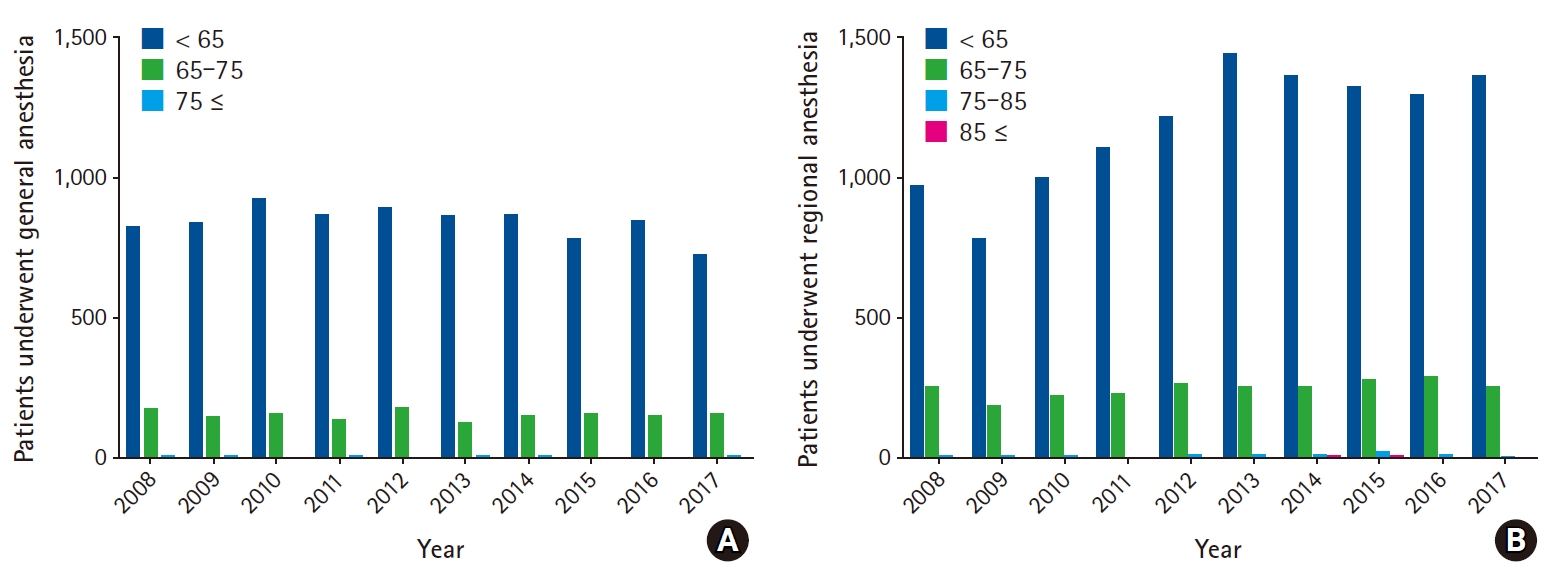
(A) Patients that underwent total hip replacement arthroplasty with general anesthesia classified by age and according to year. (B) Patients that underwent total hip replacement arthroplasty with regional anesthesia classified by age and according to year.
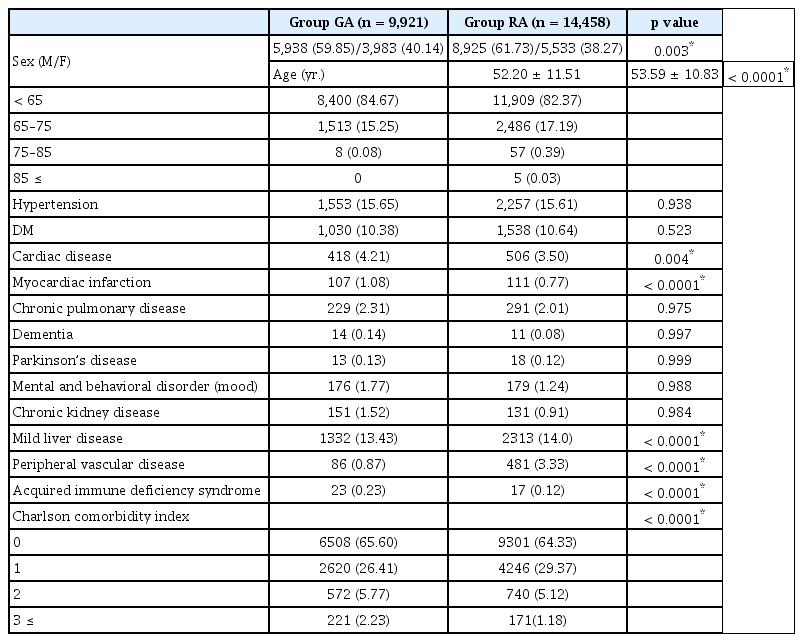
Demographic data are shown in Table 1. In patients undergoing THRA, males (P = 0.003) and elderly patients (P < 0.0001) were more likely to undergo regional anesthesia. Patients with cardiac disease were more likely to undergo general anesthesia (P = 0.004), and no difference in the anesthetic method was observed in patients with respiratory (P = 0.975) or cerebrovascular disease (P = 0.121). GA group were found to have a higher score of Charlson comorbidity index than RA group (P < 0.0001).
The most common diagnosis was necrosis in patients undergoing THRA (Table 2, P < 0.0001). The duration of hospital stay was longer in the RA group than in the GA group (P < 0.0001), and the cost of treatment was higher in the GA group than in the RA group (P < 0.001). The mortality rate during hospitalization did not differ according to the anesthetic method (P = 0.448). Of the 9,921 GA group and 14,458 RA group, 142 (1.43%) and 209 (0.86%) experienced postoperative delirium after THRA, respectively. There was no significant difference in the incidence of postoperative delirium between the groups (P = 0.92).
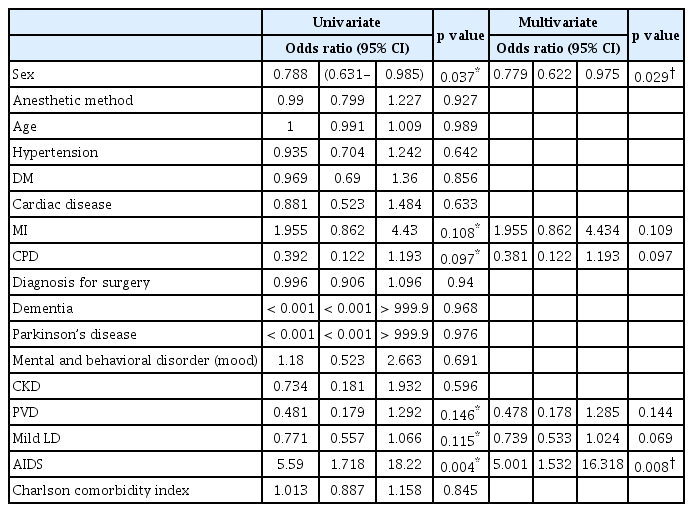
In Table 3, sex, myocardiac infarction, chronic pulmonary disease, peripheral vascular disease, mild liver disease, acquired immune deficiency syndrome (AIDS) were related with postoperative delirium (P < 0.2). Even in multivariate analysis, sex (P = 0.038) and AIDS (P = 0.008) were related with postoperative delirium. Of the patients with delirium, delirium occurred 1.97 times more frequently in men (233 [66.38%]) than in women (118 [33.62%]).
Discussion
Our results revealed that the anesthetic method is not associated with the incidence of postoperative delirium. In addition, our results showed that patients who experienced postoperative delirium after THRA were more likely to be male and patients with AIDS.
The contribution of general anesthesia as an independent risk factor for the development of postoperative delirium remains unclear. In the case of THRA, the choice of anesthesia, general or neuraxial, is decided by the anesthesiologist and is based on the patient’s preference, the clinical experience of the anesthesiologist, comorbidities, and potential postoperative complications.
A previous study [16] showed that general anesthesia with isoflurane and nitrous oxide affects postoperative spatial memory for at least three weeks in aged rats and may adversely influence memory processes in the elderly. It has been suggested that general anesthesia alters brain function, resulting in delirium [16,17]. In fact, during the first three days after surgery, the mean MMSE score was significantly decreased in patients who underwent general anesthesia [5]. Previous studies [18,19] suggest that neuraxial anesthesia reduces cortisol hypersecretion and the intensity of postoperative inflammatory response more effectively than general anesthesia, and that epidural analgesia provides better postoperative pain relief than intravenous analgesia. Neuraxial anesthesia and analgesia reduced the occurrence of postoperative complications and mortality, compared to general anesthesia and intravenous analgesia in high risk patients. Furthermore, patients who underwent general anesthesia during THRA showed significant cognitive decline for several months after surgery [20].
Weinstein and colleagues showed that patients who received neuraxial anesthesia were at a lower risk of postoperative delirium, compared with those receiving general anesthesia [21]. As regional anesthesia uses neuraxial blocks, the use of general anesthetic drugs and opiates that can cause delirium after surgery can be avoided [22]. Neuman et al. [23] reported that general anesthesia can sometimes result in severe anesthetic depth and perioperative hypotension, which increases the risk of death. However, regional anesthesia does not completely eliminate the risk of hypotension and sedation before and after surgery [24,25]. Some studies [23,25] suggest that regional anesthesia may reduce the length of hospital stay slightly. Our study also showed that the duration of hospital stay was longer in the RA group than in the GA group. There is also evidence that respiratory complications and intraoperative hypotension are more common in patients receiving general anesthesia.
However, other studies have shown different results. In one study, the perioperative use of benzodiazepines, narcotics, and anticholinergic agents was not associated with postoperative delirium in an elderly cohort of patients undergoing hip surgery [26]. Patel et al. [27] conducted a systematic review of 104 studies, concluding that anesthesia type had no effect on the development of postoperative delirium. Other studies have found no differences in postoperative morbidity, re-hospitalization rates, in-patient hospitalization costs, and mortality for elderly patients receiving regional or general anesthesia for THRA [24,28]. However, these results are lacking an extensive evidence base. Therefore, rigorous studies with appropriate methodology are required to determine the impact of anesthetic method on patient outcome.
Our study is an analysis of data related to postoperative delirium after THRA in a Korean population. The Korean NHI claims database has the great advantage of being the largest available management database that includes all payers. Moreover, all the people in Korea are covered by medical insurance. Therefore, in cases of illnesses, such as delirium, the Korean NHI claims database can be used to conduct research using a large sample size. In our study, it is likely that postoperative delirium after THRA was underdiagnosed because an incidence of 1.43% and 0.86% in the GA and RA group, respectively, is substantially lower than that reported in other studies [1,2]. This may be a result of differences in the methods of diagnosing delirium. We defined delirium as the use of medication for delirium after surgery as it was not possible to diagnose delirium using MMSE or Confusion Assessment Method. Therefore, in our study, the incidence of mild delirium might have been overlooked and, consequently, the incidence of postoperative delirium underestimated.
In addition, the NHI claims database has 97% of the national medical information of the population in Korea, but there are some limitations for clinical research. Because it is not a clinical data, it lacks detailed information about the patient and may be inaccurate because patient information was only collected using the disease code or operation code. In particular, in the case of delirium, factors such as blood pressure during operation, hypoxemia, underlying condition, American Society of Anesthesiologists physical status classification, etc. may be influenced multifactorially. However, the NHI claims database cannot confirm such data. And, data on drug management is in-hospital information, making it difficult to know exactly when to administer the drug.
In conclusion, our results suggest that anesthesia method is not associated with the incidence of postoperative delirium. Therefore, depending on the patient’s condition and the experience of the anesthesiologist, both anesthetic methods should be considered in THRA.
Notes
No potential conflict of interest relevant to this article was reported.
Funding statement
This research was supported by grant No. KSA-2018-02 from the Korean Society of Anesthesiologists.
Author Contributions
Eun-Ji Choi (Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Resources; Software; Supervision; Visualization; Writing – original draft)
Yoon Ji Choi (Conceptualization; Data curation; Funding acquisition; Investigation; Methodology; Project administration; Software; Supervision; Validation; Visualization; Writing – original draft)
Sang Won Lee (Formal analysis; Resources; Writing – review & editing)
Yun-Mi Choi (Investigation; Project administration; Validation)
Hyun-Su Ri (Funding acquisition; Software)
Ju Yeon Park (Data curation; Writing – review & editing)
Soon Ji Park (Formal analysis; Software)
Jung-Min Son (Data curation; Resources)
Yoon Sook Lee (Supervision; Writing – review & editing)
Acknowledgements
This work was supported by Department of Biostatistics, Clinical Trial Center, Biomedical Research Institute, Pusan National University Hospital.