The effect of anesthetic techniques on neutrophil to lymphocyte ratio in patients undergoing infraumbilical surgeries
Article information
Abstract
Background
Neutrophil to lymphocyte ratio (NLR) is a simple marker in peripheral blood and is used to assess inflammatory response and physiological stress during the peri-operative period. Anesthetic technique may influence NLR, thereby modulating the inflammatory response and surgical outcomes. The study aimed to evaluate the relationship between blood NLR and anesthetic techniques in patients undergoing infraumbilical surgeries.
Methods
Institutional ethical committee approval and patient consent were obtained. A prospective randomized double- blinded study was conducted between July 2017 and November 2017, involving 80 patients classified as the American Society of Anesthesiologists grade 1 and 2, aged 18–60 years, and scheduled for elective infraumbilical surgeries. Unwilling and those with infections were excluded. The patients were randomly divided into two groups: Group G (general anesthesia) and Group S (spinal anesthesia) as per the standardized protocol. Differential counts of leukocytes and NLR in the peripheral blood were obtained pre-operatively on the morning of surgery and at 2 h and 24 h after surgery in both the groups. The data were analyzed using appropriate statistical tests.
Results
The demographic parameters, basal total leukocyte count (TLC), and NLR were comparable between the groups. TLC and NLR were significantly higher in Group G as compared to that in Group S post-operatively. The post-operative rise in TLC and NLR from the basal values was significantly higher in Group G as compared to that in Group S.
Conclusions
General anesthesia was associated with a greater increase in TLC and NLR when compared with spinal anesthesia.
Introduction
The neuroendocrine system is activated during anesthesia and surgery resulting in the release of neuroendocrine hormones and cytokines [1–3]. Systemic leukocytic alterations, including leukocytosis, neutrophilia, and lymphopenia may occur in response to surgery by various hormones, cytokines, and acute-phase reactants; apoptosis of lymphocytes; or inhibition of apoptosis of neutrophils [4,5]. During anesthesia and surgery, there are changes in every stage of the immune system secondary to the changes in the general physiological response, which are linked to the extent of surgery, age of the patient, general health conditions, medications used, and blood transfusions (if performed). There are various investigations for assessing the neuroendocrine response, such as interleukin measurements (IL-6, TNF-α), cortisol levels, C-reactive protein (CRP), and leptin levels; however, these investigations are expensive.
Neutrophil to lymphocyte ratio (NLR) is a simple and inexpensive marker of inflammatory response and can provide the relationship between the inflammatory environment and physiological stress [6]. NLR has been found to be a simple predictor of outcomes in patients with cancers and patients with stable coronary artery disease [7,8]. NLR is not only affected by surgical trauma but also by the anesthetic method [6,9]. The normal NLR is found to vary across different populations from 1.65 ± 0.79 to 2.8 ± 1.6 [10,11]. The effects of neuroendocrine changes induced by different anesthetic techniques could influence NLR but the effect remains largely unknown. Very few studies have been conducted to evaluate the effects of general and spinal anesthesia on NLR [6]. Therefore, this study was conducted to evaluate the effects of different anesthetic techniques on NLR.
Materials and Methods
After obtaining approval from the ethical committee (BMCRI/PS/56/2017-18 dated: 06.07.2017) and informed written consent from the patients, a prospective double-blind randomized-controlled study was conducted involving 80 patients aged 18–60 years, classified the American Society of the Anesthesiologists grade I and II, and who were scheduled for elective open infraumbilical surgeries from July 2017 to November 2017. The study was enrolled in the Clinical Trials Registry - India (CTRI/2018/05/013826).
Patients with existing acute infections, morbid obesity; patients on chronic treatment with steroids or immunosuppressants, patients on recent chemotherapy; patients with endocrine diseases, electrolyte imbalance, hepatic and renal dysfunctions; chronic alcohol abusers; and patients with a history of undertaking surgery that lasted for > 90 min were excluded from the study. The patients were randomly allocated to one of the two groups using random numbers generated from www.random.org: Group G received general anesthesia, and Group S received spinal anesthesia for infraumbilical surgeries. Allocation concealment was ensured using sequentially numbered sealed envelopes which were opened after shifting the patients to the operation table.
All patients were assessed pre-operatively and informed thoroughly about both the techniques of anesthesia and their risks and benefits. The patients were kept fasting for 8 h before surgery. Alprazolam 0.5 mg and ranitidine 150 mg were administered orally on the previous night of surgery. Pre-operative hemoglobin level, total count, differential count, and NLR were evaluated apart from other necessary investigations. On the day of surgery, intravenous (IV) access was established and IV Ringer lactate infusion was started. Once the sealed envelopes were opened, the patients were informed about the anesthesia they would be receiving, and they were given choices to opt out of the study if they were not happy with the anesthesia technique. Routine standard of care was planned for patients who opted out of the study.
In group G, monitoring included electrocardiography (ECG), peripheral oxygen saturation (SpO2), non-invasive blood pressure (NIBP), end-tidal carbon dioxide, and train of four (TOF). The monitors were connected to the patients, and the baseline hemodynamic parameters were recorded. The patients were premedicated with glycopyrrolate 10 μg/kg, midazolam 0.03 mg/kg, and fentanyl 2 μg/kg and were pre-oxygenated for 3 min. The patients were induced with propofol (2 mg/kg) IV followed by vecuronium 0.1 mg/kg IV. After 3 min, intubation was performed with an appropriate-sized endotracheal tube. Anesthesia was maintained with 33% oxygen in 66% nitrous oxide and 1–2% isoflurane, which was titrated to maintain the hemodynamic parameters within 20% of the basal readings. Adequate muscle relaxation was ensured by maintaining the TOF count < 2 with intermittent injections of vecuronium (0.02 mg/kg). At the end of the surgery, muscle relaxation was reversed with glycopyrrolate 10 μg/kg and neostigmine 0.05 mg/kg IV, and the patients were extubated when the TOF ratio became > 0.9.
In group S, ECG, NIBP, and SpO2 monitors were connected and the baseline hemodynamic parameters were recorded. An intravenous line was started using 18 G IV cannula through which 500 ml of Ringers lactate solution was infused and midazolam 0.03 mg/kg was administered IV before administration of spinal anesthesia. Using a 25 G spinal needle, lumbar puncture was performed between L2–L3 or L3–L4 intervertebral space. After confirming the free flow of cerebrospinal fluid, 0.5% hyperbaric bupivacaine (12.5 mg) was injected into the space.
Hemodynamic parameters (heart rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure, and SpO2) were continuously monitored and recorded every 5 min till the end of surgery in both the groups. Intraoperative fluid management was guided by hemodynamic changes and intraoperative blood loss. Post-operatively, intravenous fluids, antibiotics, and other drugs were administered as per the standard institutional protocol. The pain was treated with paracetamol 1 g intravenous infusion every 6 h. Tramadol 50 mg IV was administered as a rescue analgesic if the pain persisted even after paracetamol administration. Post-operative nausea and vomiting were managed by administration of ondansetron 4 mg IV. Blood samples were collected from the antecubital vein pre-operatively on the morning of surgery and then at 2 h and 24 h after surgery. Neutrophil and lymphocyte counts were derived from differential percentages of leukocytes measured by automatic cell counters. The calculation of NLR was entrusted to one of the anesthesiologists who was blinded to the study groups. The anesthesiologist administering anesthesia to the subjects was unaware of the baseline or follow up values of the blood counts and NLR.
The sample size was calculated based on a previous study. We hypothesized that NLR would be lower in patients receiving spinal anesthesia as compared to general anesthesia. Keeping two-tailed type I (α) error at 0.05, at least 36 patients in each group were required to detect a minimum difference of 1 in NLR between the two groups with a power of 80%, assuming a standard deviation of 1.5 and NLR under general anesthesia to be 10 (based on the previous study). We enrolled 40 patients in each group to compensate for the dropouts.
The data were entered into a Microsoft excel datasheet and were analyzed using SPSS 22 version software (IBM SPSS Statistics for Windows version 22, IBM Corp., USA). Shapiro-Wilk test was applied to assess normalilty of the distribution of continuous variables. The categorical data are expressed as frequencies, and the continuous and discrete variables as mean ± SD or median (interquartile range, IQR). Chi-square test and Fisher-exact test were used for comparing the categorical data. Independent sample t-test and Mann Whitney U test were applied for continuous data with normal and skewed distribution, respectively. Paired t-test was used for intragroup comparison of normally distributed data, whereas the skewed data were compared using the Wilcoxon sign rank test. A P value of < 0.05 was considered significant.
Results
Eighty patients were included in the study (CONSORT flow-diagram, Fig. 1). There were no dropouts. The demographic characteristics, duration of surgery and the type of surgeries in both the groups were comparable at baseline (Table 1). The maximum level of sensory block attained in Group S was between T6 and T8 in most of the patients (T4 in 7 patients, T6 in 17 patients, T8 in 12 patients, and T10 in 4 patients). The total leukocyte count (TLC) was comparable between both the groups at baseline and it increased post-operatively in both the groups. The intergroup comparison showed a significantly higher TLC in group G as compared to that in Group S at 2 h, but not at 24 h post-surgery (Table 2). The median (IQR) increase in TLC from the baseline in group G was 600 (300–3325) cells/cu mm (P = 0.001) at 2 h and 1100 (600–2875) cells/cu mm (P = 0.001) at 24 h, which were both clinically and statistically significant. In group S, the median (IQR) increase in TLC from the baseline was 300 (100–625) cells/cu mm (P = 0.682) at 2 h and 535 (200–1250) cells/cu mm (P = 0.073) at 24 h, which were both clinically and statistically not significant. The changes in TLC were significantly higher in Group G as compared to that in Group S at 2 h (P = 0.002) (Fig. 2A) and 24 h (P = 0.002) post-surgery (Fig. 2B).
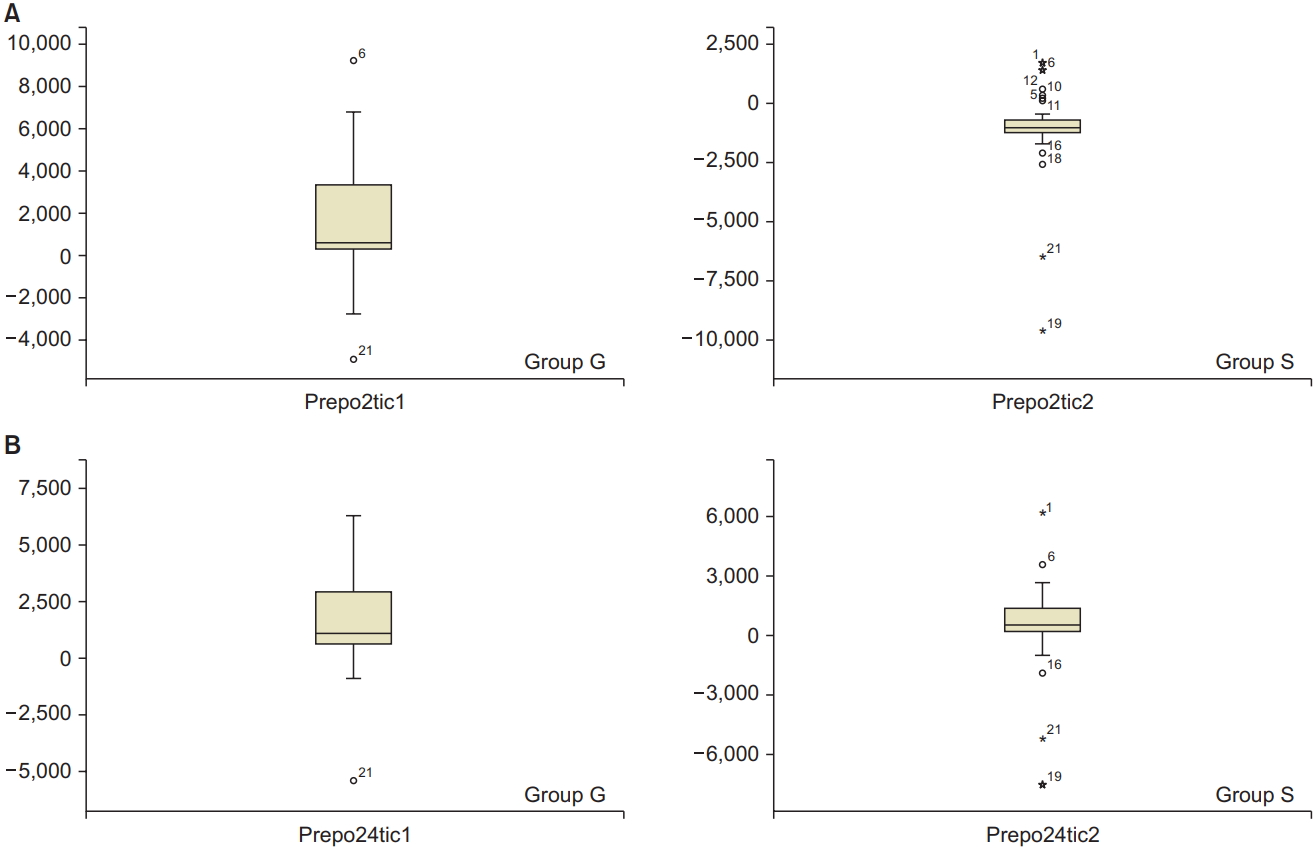
(A) Distribution of difference in total leukocyte count at 2 h from the basal value in Group G and Group S. (B) Distribution of difference in total leukocyte count at 24 h from the basal value in Group G and Group S.
The baseline NLR was comparable in both the groups at baseline, and it increased in both the groups post-operatively. The NLR was significantly higher in group G as compared to that in Group S at 2 h and 24 h post-surgery (Table 2). The median (IQR) increase in NLR from the baseline was 5 (2.73–7.16) (P < 0.001) at 2 h and 4 (2.59–6.05) (P < 0.001) at 24 h in group G, which were both clinically and statistically significant. The median (IQR) increase in NLR from the baseline was 1 (0.24–0.94) (P < 0.001) at 2 h and 0 (0.13–1.01) (P = 0.002) at 24 h in group S, which were clinically not significant. The magnitude of change in NLR was significantly higher in Group G as compared to that in Group S at 2 h (P < 0.001) (Fig. 3A) and 24 h (P < 0.001) (Fig. 3B).
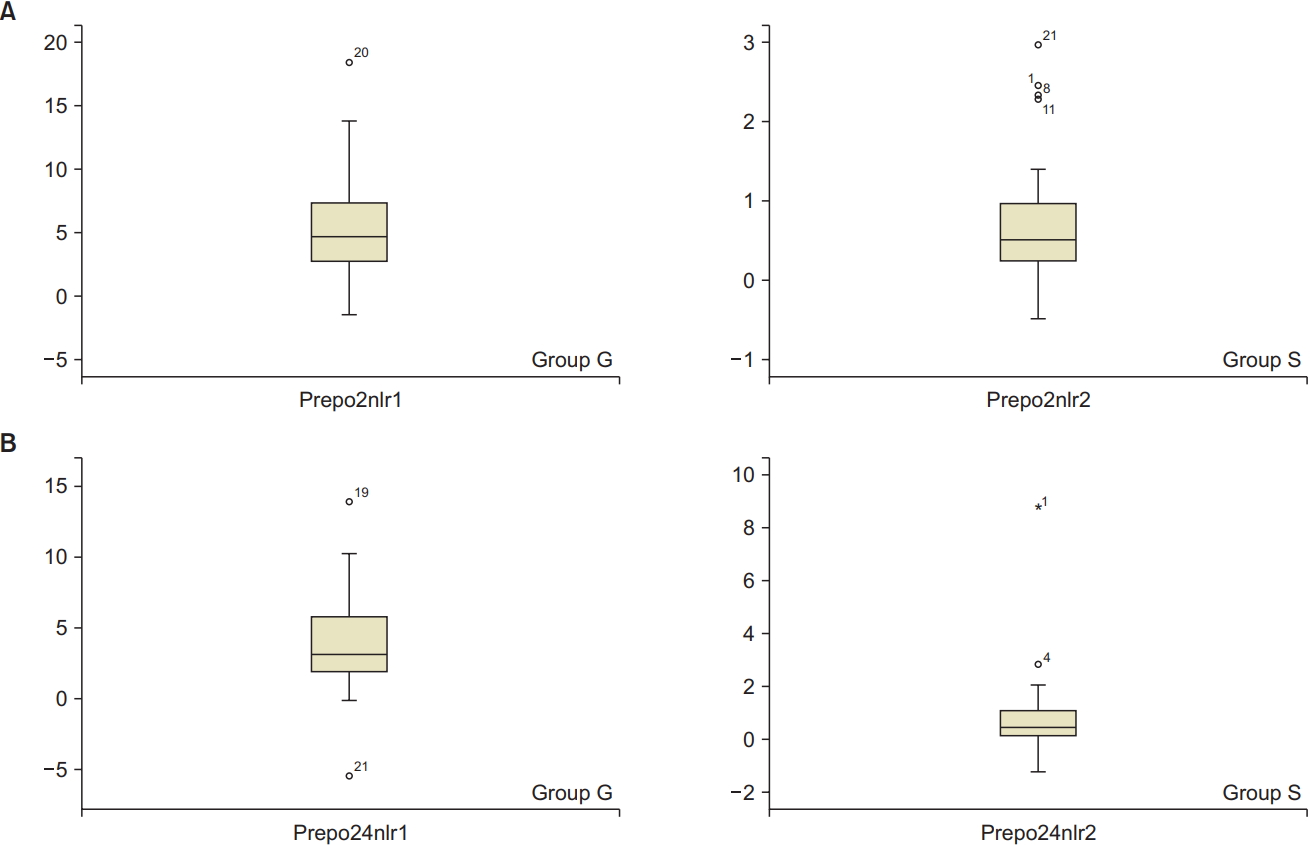
(A) Difference in NLR at 2 h from the baseline value in group G and group S. (B) Difference in NLR at 24 h from the baseline value in group G and group S. NLR: neutrophil to lymphocyte ratio.
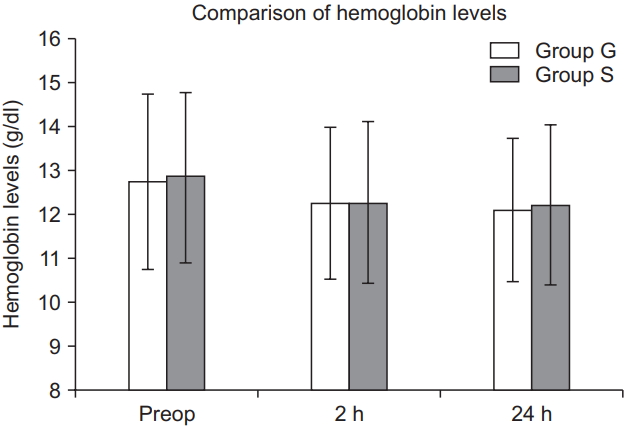
There was no significant change in the hemoglobin levels in the pre- and post-operative periods in both groups (Fig. 4). The median (IQR) changes in hemoglobin level from the baseline were 0.4% (0.2–0.625) (P = 0.001) at 2 h and 0.45% (0.2–1.0) (P < 0.001) at 24 h in group G, whereas in group S, these were 0.2% (0.12%–0.85%) (P < 0.001) at 2 h and 0.3% (0.24%–0.85%) (P < 0.001) at 24 h. These changes were statistically significant, although not clinically significant. An intergroup comparison of the change in hemoglobin level did not show significant difference (2 h, P = 0.37; 24 h, P = 0.36). There was no significant difference in the heart rate and mean arterial pressure between the two groups during the intraoperative period (Figs. 5A and 5B). The mean volume of intravenous fluids administered was 940 ± 241.57 ml in group G and 1042.5 ± 227.45 ml in group S (P = 0.054).
Discussion
In the present study, it was observed that spinal anesthesia was associated with a significantly lower NLR and a lower TLC as compared to that after general anesthesia. Studies on surgical trauma-induced stress have reported suppression of cellular resistance and susceptibility to inflammation. In addition, an increase in TLC and a reduction in the lymphocyte count in the post-operative period can increase the chance of infection [12]. These changes in leukocytes have been proposed to release inflammatory cytokines similar to IL-6. Studies have shown that changes in TLC and leukocyte subtypes are important markers of morbidity and mortality in patients with cancer, renal failure, and cardiovascular disorders [5,13,14].
Volatile anesthetic agents have been found to modulate both pro- and anti-inflammatory mediators, thereby resulting in lower lymphocyte counts [15,16]. The decreased neuroendocrine response to surgery with regional anesthesia [17] may explain the lesser increase in TLC and NLR in patients receiving spinal anesthesia.
Erbaş et al. [18], in a retrospective study, evaluated the relationship between blood NLR and anesthetic techniques in patients undergoing Cesarean section and concluded that post-operative NLR in these patients after spinal anesthesia was significantly lower as compared to that after general anesthesia, However, to the best of our knowledge, till date, are no other studies reporting the effects of anesthetic technique on NLR in patients undergoing non obstetric surgeries. The results of our study are similar to that of Erbaş et al. [18]. TLC and NLR were significantly lower in Group S as compared to those in Group G postoperatively. Another study found no increase in TLC following spinal anesthesia as compared to that following general anesthesia [19]. In the present study, although the increase in TLC was significant with general anesthesia as compared to that with spinal anesthesia, the magnitude of increase was not high.
A study investigated the effects of two general anesthetic techniques on leukocytic alterations including NLR after gynecologic laparoscopy. A significant increase in TLC, neutrophil count, and reduction in the lymphocyte count were observed at all time points after surgery in patients who received total intravenous anesthesia and who received inhalational anesthesia. NLR was significantly lower in the total intravenous anesthesia group compared to that in the inhalational anesthesia group [20]. A study assessing the correlation between NLR and post-operative complications after major abdominal surgeries found that NLR at day 7 correlated better with the incidence of post-operative complications as compared to other parameters including C reactive protein. The cut-off level for prediction of post-operative complications was found to be 5.5 [21]. However, another study found that a pre-operative NLR value of ≥ 2.3 was associated with major post-operative complications in patients undergoing colorectal surgeries [22]. The baseline NLR in the present study was a little higher than that of the mentioned studies. This could be attributed to the probable pre-operative stress as the baseline samples were obtained on the previous day of surgery before administration of the premedications.
The different types of anesthesia might have indirect effects on the post-operative complications by influencing NLR, and hence, an appropriate choice of anesthesia could influence the final outcomes. However, a study assessing the effects of general and spinal anesthesia on stress response to hemorrhoidectomy found no significant difference related to the effects of general and spinal anesthesia except for an increase in the leptin levels [23]. This could be attributed to the magnitude of surgery. Eight patients included in the study had undergone open-interval appendicectomy. These patients were included in the study as they were symptom-free (a history of acute appendicitis 6 months prior which was managed conservatively) and had no features suggestive of acute infection at the time of surgery. The volume of intravenous fluids administered in Group S was marginally higher than that in Group G. However, this might not have a significant diluent effect on the cell counts.
There are some limitations to the present study. The patients were not followed-up beyond 24 h for wound site or other infections as the post-operative management was entirely based on the surgical team’s protocol over which we had no control. Hence, the relationship between NLR and the incidence of post-operative infections and post-operative outcomes could not be established. However, a retrospective analysis of records found one patient in Group G with urinary tract infection on post-operative day 3, which improved with antibiotic treatment and there was no delay in the hospital discharge. Other investigations correlating neuroendocrine response with anesthetic technique could not be performed. Further studies are required to assess if a combination of regional anesthesia along with general anesthesia could influence the post-operative outcomes by its effect on NLR as compared to general anesthesia alone. Thus, to conclude, spinal anesthesia was found to be associated with significantly lesser variations in NLR and TLC as compared to that with general anesthesia.
Notes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Nethra Surhonne (Conceptualization; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing–review & editing)
Chaithali Hebri (Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Resources; Visualization; Writing–original draft)
Sudheesh Kannan (Conceptualization; Formal analysis; Investigation; Methodology; Resources; Software; Validation; Writing–review & editing)
Devika Rani Duggappa (Conceptualization; Formal analysis; Investigation; Project administration; Resources; Validation; Visualization; Writing–review & editing)
Raghavendra Rao RS (Conceptualization; Formal analysis; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Writing–review & editing)
Chethana G Mapari (Data curation; Investigation; Methodology; Resources; Writing–original draft)