 |
 |
| Korean J Anesthesiol > Volume 71(3); 2018 > Article |
|
Abstract
Huge goitor can lead to tracheal compression and hence difficulty in intubation. This is compounded by severe obesity. Failed tracheal intubation in difficult intubation is a serious event that may lead to increased patient morbidity and mortality. Current intubation rescue techniques and combination of different rescue techniques may increase the success rate of difficult intubation. In a 47-year-old female patient, with severe obesity and a huge goiter, our attempts at intubation using direct laryngoscope, video laryngoscope, and awake fiberoptic bronchoscope had failed. We succeeded by applying video laryngoscope to improve visualization of the airway and fiberoptic bronchoscope as a stylet for endotracheal tube.
Thyroid goiters are a risk factor for difficult intubation and respiratory complication. Numerous studies revealed high incidence of difficult intubation in thyroid surgery, ranging from 5.3%–16.5% [1]. This is compounded by other associated conditions such as morbid obesity, short neck, and huge thyroid swelling [2].
Management of the difficult airway remains problematic, despite significant progress made in designing equipment for airway visualization. Therefore, several case reports described that simultaneous use of two different equipment achieved success in difficult tracheal intubation [3–6].
We report successful airway management with combined use of a McGrath® MAC video laryngoscopy and a fiberoptic bronchoscopy in a severe obese patient with huge goiter.
A 47-year-old female patient with a nine-month history of growing thyroid goiter causing dyspnea was evaluated for total thyroidectomy. Laboratory examination, chest X-ray, and electrocardiography revealed no abnormality. The patient had hypertension, hypothyroidism, and severe obesity (body mass index 39.8 kg/m2, height 152 cm, weight 92 kg). She was suffering from severe obstructive sleep apnea that was intolerable in supine position.
Pre-operative airway assessment revealed several challenging aspects that strongly suggested difficult airway management. Her neck circumference was 51 cm with a huge thyroid goiter covering the entire anterior portion of the neck. Thickness of soft tissue measured from neck computer tomography (CT) was 49 mm that made palpation of the thyroid cartilage from the skin impossible. On neck CT, trachea was compressed bilaterally and posteriorly with slight deviation to the right side by the huge thyroid mass (Fig. 1). Her mouth opening was 3 cm, and thyromental distance could not be measured. Range of motion of the neck was 70 degrees from full flexion to full extension. Patient’s Mallampati class was IV. All options to secure the airway, from cricothyrotomy to laryngeal mask airway, were considered. However, due to location and size of the goiter and instability of the airway considering surgery, direct orotracheal intubation was inevitable.
On the day of surgery, we prepared the McGrath® MAC video laryngoscope (Aircraft Medical, UK), a fiberoptic bronchoscope (Olympus Optical, Japan), a laryngeal mask airway (LMA), and a cricothyrotomy set (Cook® Medical, USA) in case of intubation failure. On arrival in the operating room (OR), non-invasive blood pressure monitoring, electrocardiogram, and pulse oximetry were established. The monitoring revealed initial blood pressure of 159/89 mmHg, heart rate of 83 beats/min, and peripheral arterial oxygen saturation (SpO2) of 93% while breathing room air. In head up position (30 degrees), pre-oxygenation with 100% oxygen was conducted for three minutes, achieving saturation of 99%. Induction was conducted with intravenous injection of propofol 200 mg and succinylcholine 100 mg. Initial attempt with direct laryngoscopy failed due to grade IV difficulty. Following attempt with the McGrath® MAC video laryngoscope (blade size 3) with application of cricoid pressure also failed due to small oral cavity, visual field being limited to posterior part of arytenoid, and arytenoid cartilage edema (Fig. 2) that made access to vocal cords more difficult. As our third choice, we planned awake intubation with fiberoptic bronchoscope. Hydrocortisone 100 mg was injected to prevent further airway edema and 4% lidocaine was sprayed to anesthetize the airway. During the procedure, we had to apply mask ventilation periodically because the patient presented hypoxia. Due to unpredictable airway movement caused by spontaneous breathing, low patient compliance, and small oral cavity along with progression of airway edema including epiglottis, our attempt at intubation failed again. We had to abort the procedure as patient revealed signs of respiratory failure including hypoxia (SpO2 88%) and hypercapnia (end tidal CO2 62 mmHg). After injecting second dose of hydrocortisone 100 mg, we secured the airway with air-Q® intubating LMA (Cookgas®LLC, USA). Intubation of endotracheal tube (ETT) was attempted through LMA, but the tube could not be advanced due to edema of glottal area caused by multiple intubation trials. After confirming adequate ventilation with capnography, we transferred patient to surgical intensive care unit (SICU) under assisted ventilation with ambu bag and conducted respiratory care with a mechanical ventilator. Arterial blood gas analysis was pH 7.21, PaCO2 52 mmHg, PaO2 93 mmHg, base excess −7.7, and SaO2 95%. As patient’s condition improved on monitoring and arterial blood gas analysis, LMA was removed. After two days, patient was sent to a general ward.
After nine days, patient returned to the OR. Routine monitoring was established along with left radial artery cannulation under local anesthetic. After preparation of the airway with solucotef nebulizer, two trials of awake intubation with fiberoptic bronchoscope and video laryngoscope were attempted but failed again. We applied a fiberoptic bronchoscope (external diameter 5.9 mm; Olympus Optical, Japan) and the McGrath® MAC video laryngoscope (blade size 3) simultaneously (Fig. 3). Due to increasing discomfort and incompliance of the patient, intravenous injection of propofol 150 mg and succinylcholine 90 mg was administered. Intubation was conducted by two anesthesiologists. We secured oral cavity space with a video laryngoscope, thus improving visual field of the airway and simultaneously and manipulated fiberoptic bronchoscopy into the vocal cord. Visual confirmation of intra-tracheal placement of the fiberoptic scope was made on both sides, and ETT was pushed in along the fiberoptic bronchoscope. After confirming adequate ventilation with capnography and pulse oximetry, patient underwent total thyroidectomy as planned. After removing 220 g and 250 g of goiters from right and left side the patient was sent to SICU with spontaneous ventilation through ETT. Extubation was conducted after a day, and the patient was discharged after 10 days without complications.
Huge goiters can lead to tracheal compression and difficulty in endotracheal intubation. Voyagis and Kyriakos [7] reported that increased risk of difficult intubation among goiter patients compared with patients with no evidence of risk factors (6.8% vs. 0.9%). Difficult intubation rate in patients with goiter and other risk factors increased to 45.6%. Therefore, pre-operative detection of difficulty in maintaining airway or intubation during induction of anesthesia and airway control after thyroid surgery is critical.
Mask ventilation in all goiter patients may not be a problem but, goiters, when accompanied by airway deformity, constitute an aggravating factor for difficult intubation. This patient had airway deformity on neck CT and arytenoid edema as visualized by the fiberoptic bronchoscope and video laryngoscope. This edema of arytenoid and near structures, most likely due to obstruction of venous drainage caused by the huge goiter may worsen difficult intubation [8]. Therefore, we could predict difficult intubation because the patient had a huge goiter accompanied with tracheal compression, laryngeal edema, and risk factor of severe obesity.
Multiple attempts which can lead to tissue trauma, make intubation more difficult in subsequent trials, make mask ventilation more difficult, and result in hypoxia and hypercapnia. Failed tracheal intubation in difficult intubation is a serious event that may lead to increased patient morbidity and mortality. Therefore, it is imperative to choose the first intubation plan and anesthetic techniques carefully. Safe management requires timely decision-making and may require use of alternative techniques to ensure successful tracheal intubation. In this case, all options to secure airway, from cricothyrotomy to laryngeal mask airway, were taken into considered. However, cricothyrotomy could not be conducted due to the possibility of catastrophic complication in presence of the huge goiter and prolonged patient’s hypoxic condition caused by multiple attempts.
Fiberoptic intubation is used as the gold standard for elective difficult intubation management. Current intubation rescue techniques include video laryngoscopy, use of a lighted stylet, or insertion of supraglottic airway as a conduit to tracheal intubation [8]. Despite significant progress in designing equipment for airway visualization, management of the difficult airway remains problematic.
Aziz et al. [9] studied the success rate of intubation rescue techniques after failed direct laryngoscope. Use of video laryngoscope resulted in significantly higher success rate (92%) than other techniques: flexible bronchoscopic intubation 78%, supraglottic airway conduit 78%, lighted stylet 77%, and optical stylet 67%. Especially, video laryngoscope intubation may be more available than other rescue techniques because of high success rate in primary airway management and rescue-failed direct laryngoscopy [10].
Fiberoptic intubation is the gold standard procedure in managing difficult airway, however, its failure rate is reported as high as 1.2% [11]. Causes of failure are thought to be a lack of experience in manipulating the scope and inappropriate use of local anesthetics to minimize airway irritation.
Failure rate of video laryngoscopy as primary intubation technique is 2%, as a rescue technique after failed direct laryngoscope is 8%, and as a rescue technique after failed fiberoptic bronchoscope is 20%. Altered neck anatomy associated with surgical scar, radiation therapy or mass was reported as the strong predictors for failed video laryngoscopy [10].
The McGrath® MAC video laryngoscope is commonly used to provide a good view of the upper airway when conventional direct laryngoscopy fails. A video laryngoscope resembles the shape of conventional laryngoscope. Thus, the learning curve is brief, and the technique is relatively easily acquired. However, it is difficult to insert an ETT because the blade of a video laryngoscope has much greater curvature than that of a conventional direct laryngoscope [12].
In this patient, the attempt at awake fiberoptic intubation failed because the view of glottis was limited and heavily wavered along with respiration. The McGrath® MAC video laryngoscope provided a slightly better view of the vocal cord, but the view of glottis was heavily wavered and required tilting force. This force made the mouth open, but mouth opening was limited and handling of the ETT was difficult.
In addition to arytenoid edema, we could not position the tip of the ETT in front of the vocal cord opening, even with stylet. Consequently, we used the McGrath® MAC video laryngoscope for visualization of vocal cord and the fiberoptic bronchoscope as a stylet for the ETT. With application of both techniques, we could manipulate the tip of the fiberoptic bronchoscope into vocal cords, visualizing the trachea and successfully pushed the ETT along the fiberoptic bronchoscope.
Simultaneous use of video laryngoscopy and fiberoptic bronchoscopy can help achieve success in difficult tracheal intubation [3–6]. A video laryngoscope may allow easy visualization of glottis while the bronchoscope can function as an easily maneuverable stylet, avoiding trauma to glottis structures.
Under deep sedation, we first attempted tracheal intubation with the Macintosh laryngoscope and a video laryngoscope in this anticipated difficult airway with improper self-confidence of success. Consequently, these attempts may put patients in critical condition.
The only viable option is awake intubation using rescue airway techniques in anticipated difficult airway because deep sedation induces airway loss and obstruction as a result of reduced muscle tone. On the second trial, deep sedation was inevitable due to increasing discomfort and incompliance of the patient. In this situation, a combination of a video laryngoscope and a fiberoptic bronchoscope may be available for airway visualization including glottis, and thus increased the success rate of intubation. And, short acting muscle relaxant was used because of the possibility of intubation failure, despite the combined use of a video laryngoscope and a fiberoptic bronchoscope.
In conclusion, a strategy in expected difficult intubation should include identification of potential problem, consideration of different options, and selection of an appropriate plan in the particular scenario of the individual patient. Complications related to failed intubation can be decreased even more with a thorough preparation of various techniques and a combination of these techniques considering patient characteristics and clinical circumstances. We suggest a combined use of the McGrath® video laryngoscope and a fiberoptic bronchoscope as a useful option for difficult airway in a severely obese patient with huge goiter. Therefore, not one, but a combined application of airway techniques should be included in training programs.
Fig. 1.
Trachea is compressed bilaterally and posteriorly with slight deviation to the right side by huge thyroid mass (right: 7.5 cm × 4.0 cm, left: 7.3 cm × 6.0 cm).
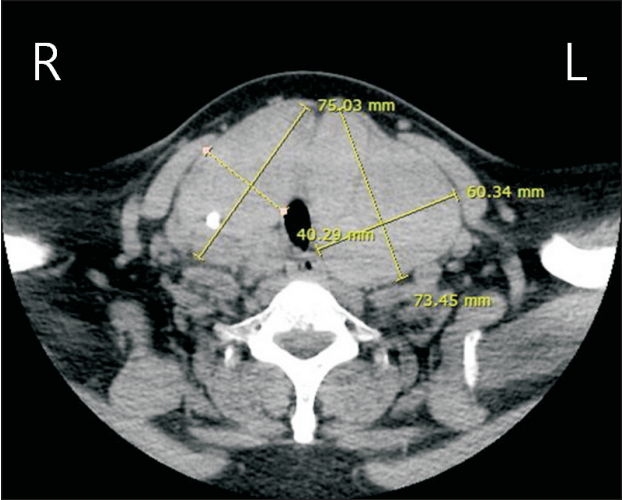
Fig. 3.
McGrath® MAC video laryngoscope (A) was used for visualization of glottis and fiberoptic bronchoscope, as a maneuverable stylet of endotracheal tube (B) were manipulated into the vocal cord simultaneously.

References
1. Bouaggad A, Nejmi SE, Bouderka MA, Abbassi O. Prediction of difficult tracheal intubation in thyroid surgery. Anesth Analg 2004; 99: 603-6.


2. Ezri T, Gewürtz G, Sessler DI, Medalion B, Szmuk P, Hagberg C, et al. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia 2003; 58: 1111-4.



3. Sharma D, Kim LJ, Ghodke B. Successful airway management with combined use of Glidescope videolaryngoscope and fiberoptic bronchoscope in a patient with Cowden syndrome. Anesthesiology 2010; 113: 253-5.


4. Kim Y, Kim JE, Jeong DH, Lee J. Combined use of a McGrath® MAC video laryngoscope and Frova Intubating Introducer in a patient with Pierre Robin syndrome: a case report. Korean J Anesthesiol 2014; 66: 310-3.



5. Park CD, Lee HK, Yim JY, Kang IH. Anesthetic management for a patient with severe mento-sternal contracture: difficult airway and scarce venous access -A case report-. Korean J Anesthesiol 2013; 64: 61-4.



6. Choi GS, Park SI, Lee EH, Yoon SH. Awake Glidescope® intubation in a patient with a huge and fixed supraglottic mass -A case report-. Korean J Anesthesiol 2010; 59 Suppl: S26-9.


7. Voyagis GS, Kyriakos KP. The effect of goiter on endotracheal intubation. Anesth Analg 1997; 84: 611-2.


8. Hariprasad M, Smurthwaite GJ. Management of a known difficult airway in a morbidly obese patient with gross supraglottic oedema secondary to thyroid disease. Br J Anaesth 2002; 89: 927-30.



9. Aziz MF, Brambrink AM, Healy DW, Willett AW, Shanks A, Tremper T, et al. Success of intubation rescue techniques after failed direct laryngoscopy in adults: a retrospective comparative analysis from the multicenter perioperative outcomes group. Anesthesiology 2016; 125: 656-66.


10. Aziz MF, Healy D, Kheterpal S, Fu RF, Dillman D, Brambrink AM. Routine clinical practice effectiveness of the Glidescope in difficult airway management: an analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology 2011; 114: 34-41.












