 |
 |
|
|
Abstract
Background
The concept of the effect-site concentration of anesthetic agents is important. The effect compartment model can be explained using the concepts of effect-site concentration and effect-site equilibration rate constant (ke0). This study confirms that the time-to-peak effect (tpe) can be measured easily in clinical practice by applying a priming dose and train-of-four (TOF) during general anesthesia induction, and ke0 can be calculated from the tpe of the four muscle relaxants that are commonly used in general anesthesia.
Methods
Eighty patients who received general anesthesia were divided into the succinylcholine, rocuronium, atracurium, or vecuronium groups. Priming doses of muscle relaxants were administered. The effects of muscle relaxants were quantified by recording the twitch response of the adductor pollicis muscle after stimulating the ulnar nerve. The tpe was measured at the lowest TOF value. ke0 was calculated from the measured tpe.
The concepts of time and concentration are important for the administration of drugs used in anesthesia. Safe anesthesia is achieved by accurately understanding the effect time of the drug and the dose-response relationship.
The time at which the effect of the drug begins is known as the onset time of the drug. The time at which the effect is maximized is the time-to-peak effect (tpe). However, since blood is not an effect site of the drug but transports the drug to an effect site, the concept of an effect-site concentration that can represent the effect is needed. When the drug is administered, the plasma concentration gradually decreases from the maximum value, and the effect-site concentration gradually increases. The tpe is the time at which the plasma concentration and the effect-site concentration are equal, and the effect-site concentration is maximum [1].
The effect compartment model was designed to explain the effect-site concentration. The effect-site equilibration rate constant (ke0), which is derived from this model, is the first-order rate constant between the effect site and plasma.
The traditional approaches to calculating the ke0 are the parametric or sequential pharmacokinetic-pharmacodynamic method and the non-parametric pharmacodynamic modeling. The disadvantage of these methods is the need for a wide range of drug effects, which start at baseline, achieve a maximum effect, and then return to baseline. The calculation of the ke0 of the drug requires the measurement of the plasma concentration and pharmacokinetic parameters after drug administration combined with the evaluation of the effect of the drug. This approach usually results in an ethically questionable situation or is unfeasible in the clinical setting [2].
The estimation of ke0 using tpe is an alternative method [2]. ke0 can be estimated by measuring tpe after the administration of a single-dose or by evaluation of the effect-site concentration-response curve during continuous infusion [3,4]. We estimated ke0 from the tpe of muscle relaxants using a single priming dose and train-of-four (TOF) during general anesthesia induction. A priming dose was used because identification of the lowest effect of the drug was not possible with an induction dose.
Knowledge of the tpe and ke0 of anesthetic agents is important for safe anesthesia. The purpose of this study is to confirm that tpe can be measured easily in clinical practice by applying a priming dose and TOF during general anesthesia induction, and ke0 can be calculated from the tpe of the four muscle relaxants that are commonly used in general anesthesia.
After receiving approval from the Institutional Review Board (File No. 2015-12-004-001), a written informed consent was obtained from each patient. Eighty patients who were undergoing elective surgery under general anesthesia for non-systemic diseases such as otitis media and chronic rhinitis were selected by referring to another study [5]. All patients belonged to the American Society of Anesthesiologists (ASA) class 1 or 2. Patients with an ASA class 3 or higher, neuromuscular diseases, liver or kidney diseases, and those without a body mass index of 18.5–30.0 kg/m2 were excluded. Eighty patients who agreed to the study protocol were randomly divided into the succinylcholine, rocuronium, atracurium, and vecuronium groups. Twenty patients were assigned to each group.
Standard monitoring devices such as non-invasive blood pressure (NIBP), electrocardiogram, and pulse oximetry were used in all patients, who remained in the supine position in the operating room. A kinemyography (KMG) (NMT Mechanosensor, Datex-Ohmeda, Finland) sensor was placed on the thumb and index finger of the arm without the NIBP monitoring device, and electrodes were attached to the wrist where the ulnar nerve passes. After preoxygenation, anesthesia was induced with thiopental sodium 5 mg/kg, 100% oxygen, and 3–5% sevoflurane. The baseline value was measured by stimulating the ulnar nerve with a maximal stimulation of up to 70 mA, and TOF values were monitored every 10 seconds. The muscle relaxants were diluted with normal saline and were prepared as 10 mg/ml of succinylcholine chloride, 10 mg/ml of rocuronium bromide, 10 mg/ml of atracurium besylate, and 1 mg/ml of vecuronium bromide. After one-fifth of the muscle relaxant dose used in the induction of general anesthesia was intravenously administered with a priming dose, the time at which the TOF value was the lowest (Fig. 1A) and the effect-site concentration was the highest (Fig. 1B) was measured and recorded. We used 0.2 mg/kg of succinylcholine, 0.1 mg/kg of rocuronium, 0.1 mg/kg of atracurium, and 0.01 mg/kg of vecuronium as the priming dose. The estimated effect-site equilibration rate constant (estimated ke0) was obtained by using the measured time-to-peak effect (measured tpe). The method of Cortínez et al. [2] was used and is described in the Appendix.
When the TOF value increased to more than 20% of the lowest value, the remaining dose (four-fifths of the total muscle relaxant dose) was intravenously administered. Endotracheal intubation was performed when the TOF value was 0%. Data were collected in real-time using a data collection program (S/5Ⓡ collect, Datex-Ohmeda, Finland).
The estimated ke0 was obtained from the measured tpe, and all values were expressed as the mean (SD). Statistical analysis was carried out using Statistical Package for Social SciencesⓇ Statistics version 24 (IBMⓇ, USA). P values smaller than 0.05 were considered statistically significant.
A second objective of the study was the comparison of the estimated ke0 value (obtained from the measured tpe) with the effect-site equilibration rate constant proposed in other studies (presented ke0) [6–9]. The estimated tpe can be calculated from the presented ke0 using some equations (detailed in the Appendix). The measured and estimated tpe and the presented and estimated ke0 within each group were compared using a one-sample t-test.
The patient characteristics of the four muscle relaxant groups are shown in Table 1. There were no significant differences in these variables between the groups.
The measured tpe of each group was 2.2 (0.4) min in the succinylcholine group, 5.1 (1.7) min in the rocuronium group, 9.6 (1.5) min in the atracurium group, and 9.6 (2.1) min in the vecuronium group. The estimated ke0 was 0.076 (0.030)/min in the succinylcholine group, 0.228 (0.122)/min in the rocuronium group, 0.062 (0.011)/min in the atracurium group, and 0.077 (0.019)/min in the vecuronium group.
Table 2 presents the results of the comparison of the estimated ke0 and measured tpe with the effect-site equilibration rate constant proposed in other studies (presented ke0) [6–9] and the time-to-peak effect, which is calculated from the presented ke0 (estimated tpe). The tpe of the succinylcholine group and the ke0 of the vecuronium group were not significantly different, but these variables were significantly different in the other groups.
Knowledge about the tpe and ke0 of anesthetic agents is important for safe anesthesia. Identification of the time of onset of a drug is easy clinically, but the determination of tpe is not easy. This study was designed to easily obtain the tpe and ke0 of anesthetic agents in clinical practice. In general anesthesia induction involving a priming dose, TOF was used to measure tpe. We developed a program using ExcelⓇ 2007 (Microsoft, USA) software with equations (shown in the Appendix) that can calculate ke0 from tpe. ke0 is estimated when tpe is input to the program. The study design and the program can be simulated to obtain the ke0 of other drugs, and herein we estimated the ke0 of the four muscle relaxants that are commonly used in anesthesia. The measured tpe of the muscle relaxants was obtained by TOF monitoring during general anesthesia induction and administering a priming dose of each muscle relaxant. According to the principle of linear pharmacokinetics, because plasma concentration or elimination is proportional to the dose, ke0 is not affected [10]. Therefore, ke0 can be obtained by the intravenous administration of the priming dose.
The TOF stimulation method is used to determine the quantitative relationship between the effect-site concentration and the drug effect. After bolus administration of the muscle relaxant, the time at which the TOF value is the lowest is the tpe. The advantages of TOF stimulation are its noninvasiveness, ease of use, and cost-effectiveness. TOF stimulation has been applied with a minimum interval of 10 seconds and is known to be more sensitive than single twitch [11–13]. In addition, TOF stimulation is more advantageous than single twitch because the latter needs to establish a baseline value before the administration of muscle relaxants. Mechanomyography (MMG) has long been regarded as the gold standard of neuromuscular monitoring, but the mechanomyogram is relatively bulky and difficult to apply, which limits its clinical use [14,15]. The KMG used in this study can be easily applied in clinical practice without significant differences from the results of MMG, electromyography (EMG), acceleromyography, and phonomyography [15–17]. However, some studies suggest that KMG rather than EMG is overestimated [18], which may be a limitation of this study.
The determination of the estimated ke0 from the measured tpe only requires a portion of the response curve, without the need to evaluate the complete course of the drug effect, and is possible by measuring the drug effect during general anesthesia induction [19]. ExcelⓇ 2007 (Microsoft, USA) software was used to calculate the estimated ke0 rather than an expensive commercial program. ExcelⓇ is relatively easy to use to obtain the estimated ke0 from the measured tpe, and the estimated ke0 can be simulated for drugs other than muscle relaxants.
Since the drug volume of distribution in the effect site can be determined from the ke0, the initial loading dose and tpe can be obtained, and additional dosages and time points can be determined. Therefore, ke0 of muscle relaxants is important in general anesthesia. In other words, the tpe and ke0 of muscle relaxants are used clinically to determine the timing of intubation of each muscle relaxant and help to determine when additional doses should be administered during anesthetic maintenance. ke0 can also be used for target-controlled infusion [1].
Because the estimated ke0 was obtained from the measured tpe of the four muscle relaxants commonly used in general anesthesia, it has significance as the estimated ke0 of each muscle relaxant in the same study design. Our results indicated a variation in the measured tpe for each patient even with the same muscle relaxant. Since the estimated ke0 was obtained from each measured tpe, the former was also affected by an individual bias. However, even in cases in which the same drug was administered at the same dose, the effects were different for each patient because of the pharmacokinetic and pharmacodynamic variability [1]. Pharmacokinetic variability is defined as the condition in which a time-concentration curve varies from person to person. Pharmacodynamic variability is defined as a condition in which a response varies from person to person at the same concentration. This limitation can be overcome by population analysis. However, although studies have suggested the various pharmacokinetic parameters, we selected the same pharmacokinetic parameters for each group of muscle relaxant [6,20–22]. Therefore, it was thought that there was no variation in the estimation of the ke0 by using pharmacokinetic parameters.
The second objective of our study was to compare the tpe and ke0 of other studies with the tpe and ke0 of our study to support the accuracy of our results. The tpe of the succinylcholine group and the ke0 of the vecuronium group were not significantly different, but these variables were significantly different in the other groups (Table 2). In the rocuronium group, the presented ke0 that we quoted in another study was 0.127/min, but ke0 values suggested in that study were 0.127/min and 0.09/min [7]. For atracurium, a study suggests a ke0 of 0.043/min [23], the other study proposes 0.068/min. The difference between this study and other studies is the use of isoflurane or propofol as the anesthetic agent as well as the use of TOF or single twitch. As inhalation anesthetics enhance the effect of muscle relaxation, they likely affect the muscle relaxation effect. TOF stimulation and single twitch were considered study variants with a high sensitivity but a low specificity.
The estimated ke0 was compared with the presented ke0, and the estimated tpe (calculated from the presented ke0) was verified by using the measured tpe. In this study, the estimated ke0 of succinylcholine, rocuronium, and atracurium was different from the presented ke0. Further studies are necessary to elucidate these results.
In conclusion, this study was designed to easily obtain the tpe and ke0 of anesthetic agents in clinical practice. The study design and the program can be simulated to obtain the ke0 of other drugs, and we estimated the ke0 of the four muscle relaxants that are commonly used in anesthesia. The estimated ke0 can be obtained from the measured tpe of these four muscle relaxants using a priming dose and TOF stimulation during general anesthesia induction, and individual deviations in tpe and ke0 are observed.
Acknowledgments
This research was supported by the 2017 scientific promotion program funded by Jeju National University.
Fig. 1.
(A) Graphic representation of the induction-course of a rocuronium-induced non-depolarizing neuromuscular blockade in one patient. Measured tpe is the time-to-peak effect obtained by using trainof-four (TOF). (B) Concentration and time course of plasma Cp(t) and effect-site Ce(t). Estimated ke0 is the value calculated using the measured time-to-peak effect.
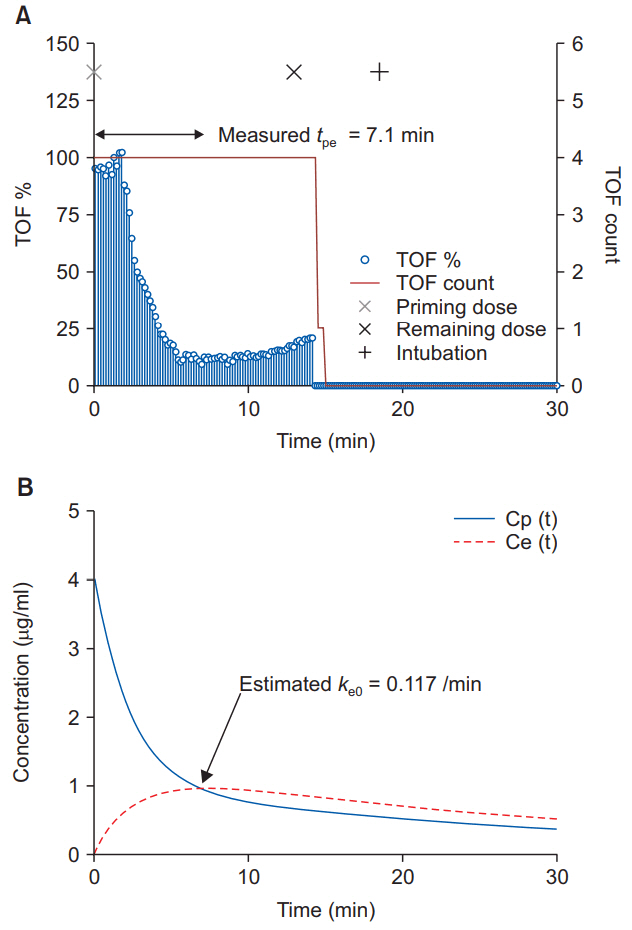
Table 1.
Patient Characteristics
Table 2.
Comparison of the Time-to-peak Effect (tpe) and the Effect-site Equilibration Rate Constant (ke0) for Each Muscle Relaxant
| Succinylcholine group (n = 20) | Rocuronium group (n = 20) | Atracurium group (n = 20) | Vecuronium group (n = 20) | |
|---|---|---|---|---|
| Measured tpe (min) | 2.2 (0.4) | 5.1 (1.7) | 9.6 (1.5) | 9.6 (2.1) |
| ↓ | ||||
| Estimated ke0 (/min) | 0.076 (0.030) | 0.228 (0.122) | 0.062 (0.011) | 0.077 (0.019) |
|
|
||||
| Estimated tpe (min) | 2.3 | 6.3 | 8.7 | 8.4 |
| ↑ | ||||
| Presented ke0 (/min) | 0.058 | 0.127 | 0.068 | 0.085 |
|
|
||||
| P value* | 0.127 | 0.005 | 0.013 | 0.020 |
| P value† | 0.013 | 0.002 | 0.027 | 0.066 |
Values are expressed as mean (SD). Measured tpe is the tpe obtained by using train-of-four (TOF). Estimated ke0 is the value calculated using the measured tpe. Estimated tpe is the value calculated using the presented ke0. Presented ke0 is the ke0 proposed in other studies. References of the presented ke0 (/min): succinylcholine [6], rocuronium [7], atracurium [8], vecuronium [9]. →: the direction of calculation, tpe (min): time-to-peak effect, ke0 (/min): effect-site equilibration rate constant.
References
1. Han DW. Pharmacokinetic and pharmacodynamic modeling in anesthetic field. Anesth Pain Med 2014; 9: 77-86.
2. Cortínez LI, Nazar C, Muñoz HR. Estimation of the plasma effect-site equilibration rate constant (ke0) of rocuronium by the time of maximum effect: a comparison with non-parametric and parametric approaches. Br J Anaesth 2007; 99: 679-85.



3. Minto CF, Schnider TW, Gregg KM, Henthorn TK, Shafer SL. Using the time of maximum effect site concentration to combine pharmacokinetics and pharmacodynamics. Anesthesiology 2003; 99: 324-33.


4. van Meurs WL, Nikkelen E, Good ML. Pharmacokinetic-pharmacodynamic model for educational simulations. IEEE Trans Biomed Eng 1998; 45: 582-90.


5. Park JC, Park KS. Comparison of pharmacodynamics and intubation conditions of muscle relaxants using a continuous infusion during induction. Korean J Anesthesiol 2006; 50: 250-5.

6. Roy JJ, Donati F, Boismenu D, Varin F. Concentration-effect relation of succinylcholine chloride during propofol anesthesia. Anesthesiology 2002; 97: 1082-92.


7. Dragne A, Varin F, Plaud B, Donati F. Rocuronium pharmacokinetic-pharmacodynamic relationship under stable propofol or isoflurane anesthesia. Can J Anaesth 2002; 49: 353-60.


8. Donati F, Gill SS, Bevan DR, Ducharme J, Theoret Y, Varin F. Pharmacokinetics and pharmacodynamics of atracurium with and without previous suxamethonium administration. Br J Anaesth 1991; 66: 557-61.



9. Alloul K, Whalley DG, Shutway F, Ebrahim Z, Varin F. Pharmacokinetic origin of carbamazepine-induced resistance to vecuronium neuromuscular blockade in anesthetized patients. Anesthesiology 1996; 84: 330-9.


10. Park JC. How to design intravenous anesthetic dose regimens based on pharmacokinetics and pharmacodynamics principles. Anesth Pain Med 2015; 10: 235-44.

11. Ali HH, Utting JE, Gray TC. Quantitative assessment of residual antidepolarizing block. I. Br J Anaesth 1971; 43: 473-7.



12. Ali HH, Utting JE, Gray TC. Quantitative assessment of residual antidepolarizing block. II. Br J Anaesth 1971; 43: 478-85.



13. Morgan GE, Mikhail MS, Murray MJ, Kleinman W, Nitti GJ, Nitti JT, et al. Clinical Anesthesiology. 5th ed. New York, McGraw-hill. 2002, p 228.
14. Jung W, Hwang M, Won YJ, Lim BG, Kong MH, Lee IO. Comparison of clinical validation of acceleromyography and electromyography in children who were administered rocuronium during general anesthesia: a prospective double-blinded randomized study. Korean J Anesthesiol 2016; 69: 21-6.



15. Gaffar EA, Fattah SA, Atef HM, Omera MA, Abdel-Aziz MA. Kinemyography (KMG) versus Electromyography (EMG) neuromuscular monitoring in pediatric patients receiving cisatracurium during general anesthesia. Egypt J Anaesth 2013; 29: 247-53.

16. Trager G, Michaud G, Deschamps S, Hemmerling TM. Comparison of phonomyography, kinemyography and mechanomyography for neuromuscular monitoring. Can J Anaesth 2006; 53: 130-5.


17. Son HJ, Lee JH, Park SW, Cho DS. The comparison among mechanical, electromyographic and accelerographic responses during recovery from vecuronium induced neuromuscular blockade. Korean J Anesthesiol 1993; 26: 910-8.

18. Salminen J, van Gils M, Paloheimo M, Yli-Hankala A. Comparison of train-of-four ratios measured with Datex-Ohmeda’s M-NMT MechanoSensorTM and M-NMT ElectroSensorTM. J Clin Monit Comput 2016; 30: 295-300.



19. Billard V, Gambus PL, Chamoun N, Stanski DR, Shafer SL. A comparison of spectral edge, delta power, and bispectral index as EEG measures of alfentanil, propofol, and midazolam drug effect. Clin Pharmacol Ther 1997; 61: 45-58.


20. Wierda JM, Kleef UW, Lambalk LM, Kloppenburg WD, Agoston S. The pharmacodynamics and pharmacokinetics of Org 9426, a new nondepolarizing neuromuscular blocking agent, in patients anaesthetized with nitrous oxide, halothane and fentanyl. Can J Anaesth 1991; 38: 430-5.


21. Kitts JB, Fisher DM, Canfell PC, Spellman MJ, Caldwell JE, Heier T, et al. Pharmacokinetics and pharmacodynamics of atracurium in the elderly. Anesthesiology 1990; 72: 272-5.


Appendix
The plasma concentration (Cp) is a composite convolution of the dosage regimen (D) and the unit disposition function (UDF). Cp can be summarized by the following equation:
where Ⓧ represents a convolution. When t is 0 and D is 1, Cp(t) becomes UDF(t). The UDF(t) of the multi-compartment model is presented by the following equation [10]:
where Ai is the coefficient and λi is the exponent, and these variables are obtained from the volume (Vi) and the micro-rate constant (kij) shown in Table A.
In the compartment models, the effect-site compartment includes the effect-site equilibration rate constant (ke0), and the volume of the effect site and the drug movement with the central compartment are negligible. The effect-site concentration (Ce) is represented by the following equation [10]:
Since the rate of increase or decrease of the effect-site concentration is 0 at the time-to-peak effect (tpe), when C'e(t) is 0, t is tpe. The tpe is estimated by substituting ke0 into the following equation [10]:
In contrast, ke0 can be estimated from the measured tpe. Considering that the plasma concentration and the effect-site concentration are in equilibrium at the measured tpe, ke0 can be calculated by the following equation [10]:
These equations were used in ExcelⓇ 2007 (Microsoft, USA) to construct a simulation program. The program can calculate tpe using ke0, and can derive ke0 by substituting tpe. The pharmacokinetic parameters used for each muscle relaxant are shown in Table A.
Table A. Pharmacokinetic Parameters of Muscle Relaxants
| Succinylcholine: Roy et al. [6] | Rocuronium: Wierda et al. [20] | Atracurium: Kitts et al. [21] | Vecuronium: Sohn et al. [22] | |
|---|---|---|---|---|
| k10 (/min) | 5.0 (2.6) | 0.1 | 0.166 | 0.099 (0.049) |
| k12 (/min) | 2.9 (3.9) | 0.21 | 0.217 | 0.23 (0.18) |
| k21 (/min) | 1.6 (0.4) | 0.13 | 0.123 | 0.19 (0.12) |
| k13 (/min) | - | 0.028 | - | 0.086 (0.024) |
| k31 (/min) | - | 0.01 | - | 0.013 (0.007) |
| V1 (L/kg) | 0.009 (0.003) | 0.045 | 0.032 | 0.048 (0.02) |
| V2 (L/kg) | 0.016 | 0.073 | 0.068 | 0.054 (0.031) |
| V3 (L/kg) | - | 0.126 | - | 0.38 (0.22) |









