|
 |
|
|
Abstract
Background
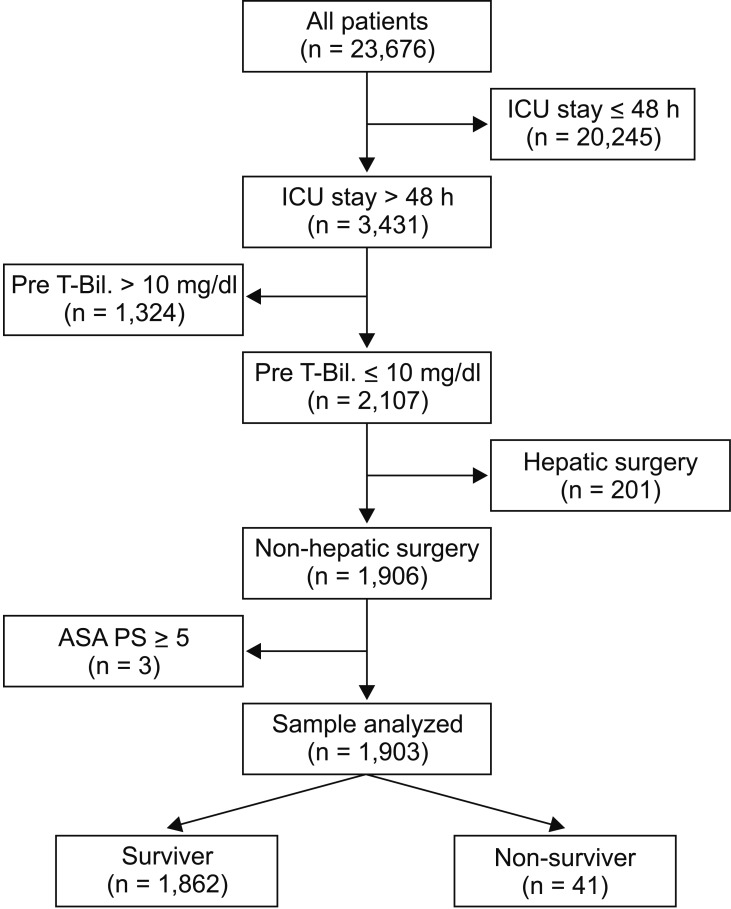
Methods
Results
References
Table┬Ā1
Proximate Causes of Death in 41 Non-survivors
| Proximate cause of death | n (%) |
|---|---|
| Neurological | 4 (9.8%) |
| Cardiovascular | 12 (29.3%) |
| Respiratory | 20 (48.8%) |
| Liver failure | 3 (7.3%) |
| Other | 2 (4.9%) |
Table┬Ā2
Comparison between Postoperative Survivors and Non-survivors
Data are presented as percentages (n/valid cases) or as the median (25% quartile, 75% quartile). Comparisons between two groups were performed using the Mann-Whitney U test and chi-square test. ASA-PS: American Society of Anesthesiologists-physical status, ICU: intensive care unit, APACHE: acute physiology and chronic health evaluation. *APACHE II score was obtained in 1,072 of 1,903 patients, including 1,031 of 1,862 survivors (55.4%) and all of 41 non-survivors (100%).
Table┬Ā3
Comparison of Bilirubin Level between Postoperative Survivors and Non-survivors
Table┬Ā4
Multivariate Analysis of the Association between Postoperative Bilirubin Level and Postoperative Mortality
POD: postoperative day, D-Bil: direct bilirubin, I-Bil: indirect bilirubin, ASA-PS: American Society of Anesthesiologists-physical status, CI: confidence interval. *APACHE II score was obtained in 1,072 of 1,903 patients, including 1,031 of 1,862 survivors (55.4%) and all of 41 non-survivors (100%).
Table┬Ā5
Associations between Mild and Moderate Hyperbilirubinemia and Postoperative Mortality
Multivariate logistic analysis was performed using hyperbilirubinemia of D-Bil and I-Bil, age, ASA-PS, operation category, and emergency operation as dependent variables, and mortality as the independent variable. POD: postoperative day, D-Bil: direct bilirubin, I-Bil: indirect bilirubin, ASA-PS: American Society of Anesthesiologists-physical status.
Table┬Ā6
Association between Postoperative Direct and Indirect Bilirubin Levels and ICU-free Survival Days at 28 Days after the Operation
Multivariate linear regression analysis was performed using D-Bil, I-Bil, age, ASA-PS, operation category, and emergency operation as dependent variables, and mortality as the independent variable. IFSD: ICU-free survival days at 28 days after the operation, POD: postoperative day(s), D-Bil: direct bilirubin, I-Bil: indirect bilirubin, ASA-PS: American Society of Anesthesiologists-physical status.