 |
 |
|
|
Abstract
Background
Dexmedetomidine is an alpha-2 adrenergic agonist with sedative, anxiolytic, and analgesic properties. This study was designed to evaluate the inhibitory effects of preoperative administration of 0.5 µg/kg dexmedetomidine on hemodynamic responses caused by endotracheal intubation in elderly patients undergoing treatment for hypertension.
Methods
Forty elderly (≥ 65 years old) patients who had been receiving hypertension treatment, had American Society of Anesthesiologists physical status II, and were scheduled to undergo elective noncardiac surgery were randomly selected and assigned to 2 groups. Group C received normal saline and group D received 0.5 µg/kg dexmedetomidine intravenously over 10 min just before endotracheal intubation. Systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), and heart rate (HR) were recorded preoperatively in the ward, immediately after study drug administration, and at 1, 3, and 5 min after endotracheal intubation.
Dexmedetomidine is a highly selective alpha-2 adrenergic agonist with dose-dependent sedative, anxiolytic, and analgesic effects [1], and preoperative administration of dexmedetomidine is known to reduce sympathetic tone and maintain hemodynamic stability. Several studies have documented the effects of dexmedetomidine on hemodynamic responses during laryngoscopy and tracheal intubation [2].
Laryngoscopy and tracheal intubation are risky processes that can cause tachycardia, hypertension, or arrhythmia, because of the sympathetic adrenergic outflow caused by laryngeal tissue stimulation [3,4,5]. Furthermore, this hemodynamic instability is associated with perioperative complications, especially in elderly patients with a comorbid disease, and may result in catastrophic effects, such as, myocardial ischemia, cardiac arrhythmia, or a cerebrovascular accident [3]. Therefore, anesthesiologists have used various medications to attenuate the sympathetic responses. However, many of the studies on this topic limited their study populations to young and normotensive individuals. Nevertheless, hemodynamic instability presents higher levels of risk in elderly patients with a comorbid disease than in the abovementioned patient populations, because the reserve capacity of the cardiovascular system is decreased in elderly patients [6].
In general, dose reduction of dexmedetomidine is recommended for elderly patients (≥ 65 years old), and the US Food and Drug Administration recommends a loading dose of 0.5 µg/kg instead of 1 µg/kg. In addition, many study results support the effectiveness of a 0.5 µg/kg loading dose in both young and elderly patients.
This study included elderly patients undergoing treatment for hypertension. These patients are known to show more pronounced hemodynamic responses to sympathetic stimulation. Therefore, a 0.5 µg/kg loading dose of dexmedetomidine may not be sufficient to attenuate the hemodynamic responses to endotracheal intubation.
Therefore, we investigated the effect of a 0.5 µg/kg single preoperative dose of dexmedetomidine on the hemodynamic stability of elderly patients undergoing treatment for hypertension.
After obtaining approval from the clinical research ethics committee at our hospital, we obtained written informed consent from all participating patients. The clinical trial was registered at clinicaltrials.gov in May 2016, with registration No.NCT02768610.
We screened 44 patients and 42 patients of both sexes aged between 65 and 85 years, with American Society of Anesthesiologists physical status II, Mallampati classification I or II, body mass index (BMI) ≤ 35 kg/m2, and scheduled to undergo elective noncardiac surgery were enrolled in this study. All patients had a diagnosis of hypertension and were undergoing treatment with antihypertensive medications. We excluded 2 patients with BMI ≥ 35 kg/m2. The dropout rate was 9%. Two patients in whom the endotracheal intubation attempt lasted longer than 20 s were excluded. The flow chart for the study is presented at Fig. 1.
The study had a placebo-controlled, randomized, double-blinded, prospective design. The 42 patients were randomly allocated to 2 groups by using a closed-envelope method—a control group (group C) that received normal saline and a comparative group (group D) that received dexmedetomidine. An anesthesiologist unaware of the study details prepared the syringes containing dexmedetomidine or normal saline.
Patients were premedicated with 0.2 mg glycopyrrolate intramuscularly, and antihypertensive medications were maintained until the day of surgery. After arrival at the operating room, the patients were connected to a continuous electrocardiograph, pulse oximeter, and noninvasive blood pressure monitor. Group D patients (n = 22) were administered 0.5 µg/kg dexmedetomidine (Precedex™; Hospira Inc., Lake Forest, IL, USA) intravenously over 10 min. Group C patients were administered the same volume of normal saline (also intravenously for 10 min). Saline and dexmedetomidine were administered using a syringe pump by an anesthesiologist unaware of the study protocol. After completing the saline or dexmedetomidine administration, thiopental sodium (5 mg/kg) and rocuronium (0.6 mg/kg) were administered. Two minutes after these administrations, endotracheal intubation was performed using a laryngoscope; the intubation condition of all patients was excellent or good. All intubations were performed within 20 s by one anesthesiologist except two patients in group D. Anesthesia was maintained with 2% sevoflurane in a 50 : 50 nitrous oxide/oxygen mixture for 5 min and was followed by 1.5 to 2.5% sevoflurane in a 50 : 50 nitrous oxide/oxygen mixture.
Systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), and heart rate (HR) were recorded in the ward just before departure to the operating room (baseline value), immediately after study drug administration, and at 1, 3, and 5 min after endotracheal intubation.
If hypotension or bradycardia (SBP < 90 mmHg and HR < 60 beats/min) occurred, ephedrine and atropine were administered, respectively.
According to a power analysis, a sample size of 20 patients per group was determined sufficient to detect a 20% change in blood pressure and HR between the two groups with a power of 80% at the 5% significance level [7,8]. Assuming a 10% dropout rate, we planned to enroll 44 patients. Data were analyzed using PASW Statistics for Windows, version 18.0 (SPSS Inc, Chicago, IL, USA). Group demographics and intergroup comparisons of SBP, DBP, MAP, and HR were analyzed using Student's t-test, and intragroup comparisons were performed using the paired t-test. Results are presented as means ± SD, and P values of < 0.05 were considered statistically significant.
Group demographic data are summarized in Table 1. No significant differences were observed between groups C and D in terms of demographic characteristics.
The mean SBP was significantly lower in group D than in group C at 1, 3, and 5 min after intubation (Table 2). In group C, SBP was significantly higher at 1 min (186.0 ± 26.6, P < 0.001) and 3 min (160.1 ± 23.2, P < 0.001) after intubation than at baseline (135.1 ± 13.4), and in group D, SBP was significantly higher at 1 min (165.2 ± 16.2, P < 0.001) but lower at 5 min (108.4 ± 12.6, P < 0.001) after intubation than at baseline (135.4 ± 23.8) (Fig. 2). The maximum increase in SBP was 37.7% in group C, and the minimum increase was 22% in group D at 1 min after intubation.
The mean DBP was significantly lower in group D than in group C at 3 and 5 min after intubation, but no intergroup difference was observed at 1 min (Table 2). In group C, DBP was significantly higher at 1 min (104.8 ± 14.9, P < 0.001) and 3 min (87.9 ± 15.5, P = 0.028) after intubation than at baseline (79.7 ± 9.8). In group D, DBP was significantly higher at 1 min (97.0 ± 14.5, P < 0.001) and lower at 5 min (66.5 ± 7.2, P < 0.001) after intubation than at baseline (76.7 ± 8.3) (Fig. 3). The maximum increase in DBP was 31.5% in group C, and the minimum increase was 26.4% in group D at 1 min after intubation.
The mean MAP was significantly lower in group D than in group C at 1, 3, and 5 min after intubation (Table 2). In group C, MAP was significantly higher at 1 min (137.2 ± 18.3, P < 0.001) and 3 min (116.9 ± 16.2, P < 0.001) after intubation than at baseline (100.3 ± 11.9), and in group D, MAP was significantly higher at 1 min (123.4 ± 13.8, P < 0.001) and significantly lower at 5 min (83.4 ± 8.4, P < 0.001) after intubation than at baseline (97.7 ± 14.9) (Fig. 4). The maximum increase in MAP was 36.8% in group C, and the minimum increase was 26.4% in group D at 1 min after intubation.
The mean HR was significantly lower in group D than in group C at 3 and 5 min after intubation, but no intergroup difference was observed at 1 min (Table 2). In group C, HR was significantly higher at 1 min (92.9 ± 13.5, P < 0.001) and 3 min (82.2 ± 10.3, P < 0.001) after intubation than at baseline (70.3 ± 7.4), and in group D, HR was significantly higher at 1 min (85.2 ± 12.6, P < 0.001) but lower at 5 min (65.7 ± 9.5, P = 0.007) after intubation than at baseline (72.1 ± 7.0) (Fig. 5). The maximum increase in HR was 32.1% in group C, and the minimum increase was 18.1% in group D at 1 min after intubation.
Laryngoscopy and endotracheal intubation are known to be associated with perioperative hemodynamic instabilities, such as, hypertension, cardiac arrhythmia, and tachycardia, occurring secondary to the stimulation of the sympathetic nervous system [3,4,5]. In addition, sudden hemodynamic changes may lead to serious complications, especially in patients with a comorbid disease like hypertension [3]. Accordingly, anesthesiologists have devised means of attenuating the sympathetic stimulation in order to decrease the incidences of perioperative complications by using drugs, including opioids, adrenergic blockers, vasodilators, calcium channel blockers, lidocaine, and inhaled anesthetics [9,10,11,12,13,14,15]. Although many reports claim various drugs effectively attenuate hemodynamic responses, they also mention unexpected side effects like hypoventilation, hypotension, bradycardia, and muscle rigidity [16].
Dexmedetomidine is a selective alpha-2 agonist with a sympatholytic effect as well as sedative, hypnotic, anxiolytic, analgesic, and anesthetic sparing effects [1], which are mediated through alpha-2 adrenoreceptors in the central and peripheral nervous systems. Because of these effects, anesthesiologists use dexmedetomidine as a spinal anesthesia adjunct as well as for general anesthesia [17,18,19]. In addition, dexmedetomidine can be administered for intensive care unit sedation, procedural sedation, and monitored anesthesia care.
In previous studies, researchers have used doses of dexmedetomidine ranging from 0.25 to 2 µg/kg. The effects of dexmedetomidine are known to be dose-dependent, but the probabilities of side effects like bradycardia or hypotension also increase with dosage. Therefore, optimal dose adjustment according to the characteristics of the patient group is important. Lawrence et al. [20] reported that a single dose of dexmedetomidine before anesthesia induction attenuated the hemodynamic response to intubation and extubation; however, they used 2 µg/kg dexmedetomidine, and hypotension and bradycardia were found to occur more frequently in their dexmedetomidine group than in the control group. Keniya et al. [21] reported that patients administered 1 µg/kg dexmedetomidine required more treatment for bradycardia than the controls did. In contrast, Scheinin et al. [8] reported that 0.6 µg/kg dexmedetomidine attenuated cardiovascular responses to laryngoscopy and tracheal intubation in healthy individuals without serious side effects, and Basar et al. [22] reported that 0.5 µg/kg dexmedetomidine decreased thiopental requirements without causing serious hemodynamic effects or affecting recovery time. However, the abovementioned studies were conducted in young and normotensive individuals. Dose reduction is required in the elderly because of age-associated pharmacodynamic changes, and some studies have reported more pronounced hemodynamic responses to drugs in patients with hypertension [23,24].
Hence, we decided to preoperatively administer 0.5 µg/kg dexmedetomidine rather than 1.0 µg/kg to our elderly patients undergoing treatment for hypertension, and we found at this dose effectively suppressed the hemodynamic responses caused by endotracheal intubation without serious side effects.
In group D, all hemodynamic parameters were significantly lower at 5 min after intubation than at baseline and showed a decreasing trend from 1 min to 5 min after intubation. However, at 5 min after intubation, the hemodynamic values were still in the normal range (changes within 20%), and the commencement of surgical procedures halted this decreasing trend.
Basar et al. [22] reported that 0.5 µg/kg dexmedetomidine decreased thiopental requirements, with an administered dose of 4.9 mg/kg for anesthesia induction. Keniya et al. [21] reported that 1 µg/kg dexmedetomidine decreased thiopental requirements, with an administered dose of 4.4 mg/kg for anesthesia induction. Therefore, in the present study, we decided to administer 5 mg/kg of thiopental for anesthesia induction.
Propofol is another favorable induction agent with a cardiovascular depressive property, and is more effective at suppressing stress hormone release than is thiopental [25]. Studies have shown severe hypotensive episodes requiring vasoconstrictor treatment after general anesthesia induction in patients chronically using angiotensin II antagonists [26]. Although none of our patients experienced a hypotensive episode, additional study of the hemodynamic responses to different antihypertensive drugs and alpha-2 agonists, and the use of propofol rather than thiopental for anesthesia induction, may be needed.
In conclusion, our study shows that the preoperative administration of 0.5 µg/kg dexmedetomidine before anesthesia induction effectively suppresses the hemodynamic changes caused by endotracheal intubation in elderly patients (≥ 65 years old) undergoing treatment for hypertension, without causing any severe side effects.
References
1. Virtanen R, Savola JM, Saano V, Nyman L. Characterization of the selectivity, specificity and potency of medetomidine as an alpha 2-adrenoceptor agonist. Eur J Pharmacol 1988; 150: 9-14. PMID: 2900154.


2. Yildiz M, Tavlan A, Tuncer S, Reisli R, Yosunkaya A, Otelcioglu S. Effect of dexmedetomidine on haemodynamic responses to laryngoscopy and intubation : perioperative haemodynamics and anaesthetic requirements. Drugs R D 2006; 7: 43-52. PMID: 16620136.


3. Prys-Roberts C, Greene LT, Meloche R, Foëx P. Studies of anaesthesia in relation to hypertension. II. Haemodynamic consequences of induction and endotracheal intubation. Br J Anaesth 1971; 43: 531-547. PMID: 5089931.



4. Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth 1987; 59: 295-299. PMID: 3828177.



5. Edwards ND, Alford AM, Dobson PM, Peacock JE, Reilly CS. Myocardial ischaemia during tracheal intubation and extubation. Br J Anaesth 1994; 73: 537-539. PMID: 7999498.



7. Zhan-Ying G, Chang-Ming W, Shuai T, Lin-Lin T, Yu-Feng H. Comparison of effects of different doses dexmedetomidine on inhibiting tracheal intubation-evoked haemodynamic response in the elderly patients. J Clin Diagn Res 2015; 9: UC10-UC13. PMID: 26500982.



8. Scheinin B, Lindgren L, Randell T, Scheinin H, Scheinin M. Dexmedetomidine attenuates sympathoadrenal responses to tracheal intubation and reduces the need for thiopentone and peroperative fentanyl. Br J Anaesth 1992; 68: 126-131. PMID: 1347229.



9. Thompson JP, Hall AP, Russell J, Cagney B, Rowbotham DJ. Effect of remifentanil on the haemodynamic response to orotracheal intubation. Br J Anaesth 1998; 80: 467-469. PMID: 9640152.



10. Ko BJ, Oh JN, Lee JH, Choi SR, Lee SC, Chung CJ. Comparison of effects of fentanyl and remifentanil on hemodynamic response to endotracheal intubation and myoclonus in elderly patients with etomidate induction. Korean J Anesthesiol 2013; 64: 12-18. PMID: 23372880.



11. Prys-Roberts C, Foëx P, Biro GP, Roberts JG. Studies of anaesthesia in relation to hypertension. V. Adrenergic beta-receptor blockade. Br J Anaesth 1973; 45: 671-681. PMID: 4147153.



12. Kale SC, Mahajan RP, Jayalakshami TS, Raghavan V, Das B. Nifedipine prevents the pressor response to laryngoscopy and tracheal intubation in patients with coronary artery disease. Anaesthesia 1988; 43: 495-497. PMID: 3261548.


13. Mikawa K, Nishina K, Maekawa N, Obara H. Comparison of nicardipine, diltiazem and verapamil for controlling the cardiovascular responses to tracheal intubation. Br J Anaesth 1996; 76: 221-226. PMID: 8777101.



14. Sun HL, Wu TJ, Ng CC, Chien CC, Huang CC, Chie WC. Efficacy of oropharyngeal lidocaine instillation on hemodynamic responses to orotracheal intubation. J Clin Anesth 2009; 21: 103-107. PMID: 19329013.


15. Stoelting RK. Blood pressure and heart rate changes during short-duration laryngoscopy for tracheal intubation: influence of viscous or intravenous lidocaine. Anesth Analg 1978; 57: 197-199. PMID: 565157.


16. Min JH, Chai HS, Kim YH, Chae YK, Choi SS, Lee A, et al. Attenuation of hemodynamic responses to laryngoscopy and tracheal intubation during rapid sequence induction: remifentanil vs. lidocaine with esmolol. Minerva Anestesiol 2010; 76: 188-192. PMID: 20203546.

17. Park SH, Shin YD, Yu HJ, Bae JH, Yim KH. Comparison of two dosing schedules of intravenous dexmedetomidine in elderly patients during spinal anesthesia. Korean J Anesthesiol 2014; 66: 371-376. PMID: 24910729.



18. Ok HG, Baek SH, Baik SW, Kim HK, Shin SW, Kim KH. Optimal dose of dexmedetomidine for sedation during spinal anesthesia. Korean J Anesthesiol 2013; 64: 426-431. PMID: 23741565.



19. Shin HW, Yoo HN, Kim DH, Lee H, Shin HJ, Lee HW. Preanesthetic dexmedetomidine 1 μg/kg single infusion is a simple, easy, and economic adjuvant for general anesthesia. Korean J Anesthesiol 2013; 65: 114-120. PMID: 24023992.



20. Lawrence CJ, De Lange S. Effects of a single pre-operative dexmedetomidine dose on isoflurane requirements and peri-operative haemodynamic stability. Anaesthesia 1997; 52: 736-744. PMID: 9291757.


21. Keniya VM, Ladi S, Naphade R. Dexmedetomidine attenuates sympathoadrenal response to tracheal intubation and reduces perioperative anaesthetic requirement. Indian J Anaesth 2011; 55: 352-357. PMID: 22013250.



22. Basar H, Akpinar S, Doganci N, Buyukkocak U, Kaymak C, Sert O, et al. The effects of preanesthetic, single-dose dexmedetomidine on induction, hemodynamic, and cardiovascular parameters. J Clin Anesth 2008; 20: 431-436. PMID: 18929283.


23. Prys-Roberts C, Meloche R, Foëx P. Studies of anaesthesia in relation to hypertension. I. Cardiovascular responses of treated and untreated patients. Br J Anaesth 1971; 43: 122-137. PMID: 5550843.



24. Stone JG, Foëx P, Sear JW, Johnson LL, Khambatta HJ, Triner L. Risk of myocardial ischaemia during anaesthesia in treated and untreated hypertensive patients. Br J Anaesth 1988; 61: 675-679. PMID: 3207540.



25. Misiołek H, Wojcieszek E, Dyaczyńska-Herman A. Comparison of influence of thiopentone, propofol and midazolam on blood serum concentration of noradrenaline and cortisol in patients undergoing non-toxic struma operation. Med Sci Monit 2000; 6: 319-324. PMID: 11208330.

26. Bertrand M, Godet G, Meersschaert K, Brun L, Salcedo E, Coriat P. Should the angiotensin II antagonists be discontinued before surgery? Anesth Analg 2001; 92: 26-30. PMID: 11133595.


Fig. 1
Flow chart of the study. Forty-four patients were recruited, and 2 obese patients (body mass index > 35 kg/m2) were excluded. Randomization was done on 42 patients, with 20 in the control group and 22 in the dexmedetomidine group. Intervention was discontinued in 2 patients in the dexmedetomidine group because the intubation attempt lasted more than 20 s.
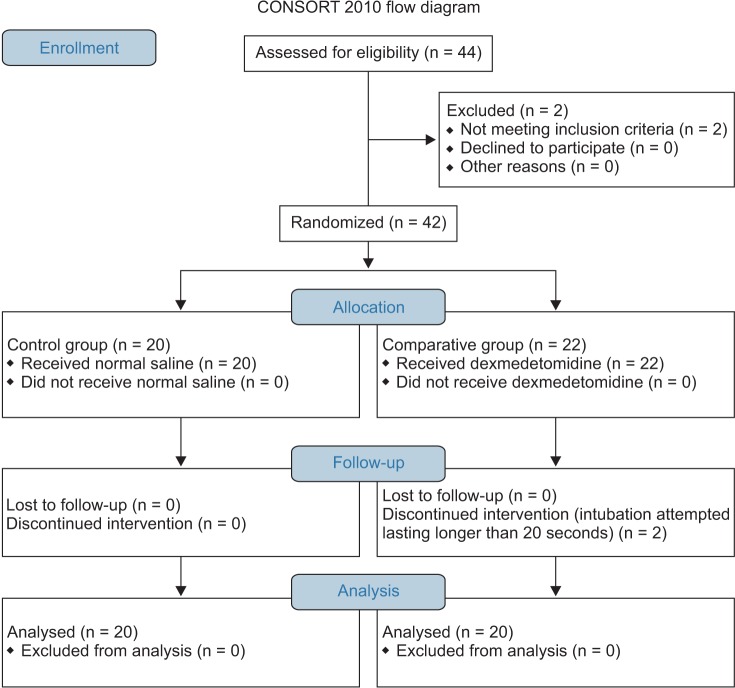
Fig. 2
Changes in systolic blood pressure (SBP) in the 2 groups. Group C: normal saline, Group D: dexmedetomidine. *P < 0.05 indicates a significant increase in each group, compared to the baseline values. †P < 0.05 indicates a significant decrease noted in Group D, compared to the baseline values. ‡P < 0.05 indicates a significant difference between the groups.

Fig. 3
Changes in diastolic blood pressure (DBP) in the 2 groups. Group C: normal saline, Group D: dexmedetomidine. *P < 0.05 indicates a significant increase in each group, compared to the baseline values. †P < 0.05 indicates a significant decrease noted in Group D, compared to the baseline values. ‡P < 0.05 indicates a significant difference between the groups.
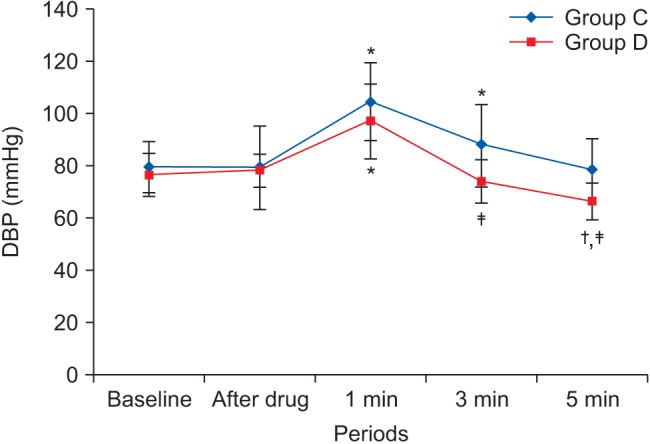
Fig. 4
Changes in mean arterial pressure (MAP) in the 2 groups. Group C: normal saline, Group D: dexmedetomidine. *P < 0.05 indicates a significant increase in each group, compared to the baseline values. †P < 0.05 indicates a significant decrease noted in Group D, compared to the baseline values. ‡P < 0.05 indicates a significant difference between the groups.
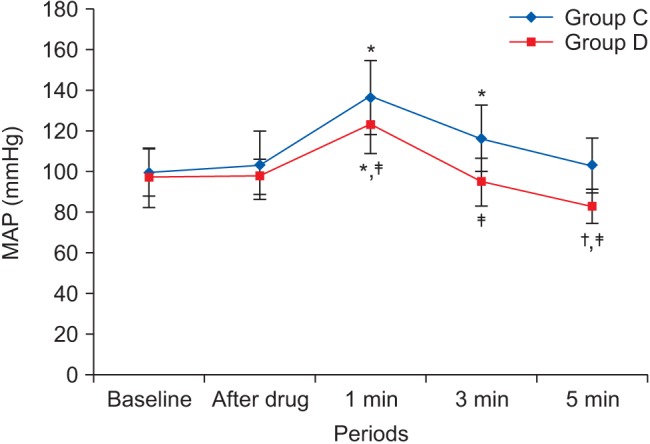
Fig. 5
Changes in heart rate (HR) in the 2 groups. Group C: normal saline, Group D: dexmedetomidine. *P < 0.05 indicates a significant increase in each group, compared to the baseline values. †P < 0.05 indicates a significant decrease noted in Group D, compared to the baseline values. ‡P < 0.05 indicates a significant difference between the groups.
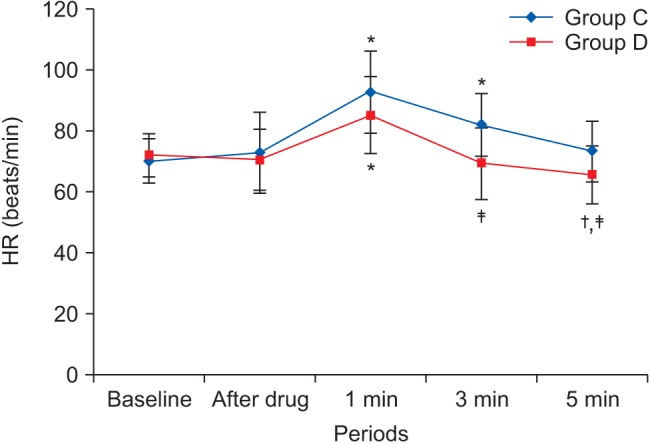
Table 1
Demographic Data
| Group C (n = 20) | Group D (n = 20) | |
|---|---|---|
| Age (yr) | 73.5 ± 5.1 | 73.2 ± 5.4 |
| Sex (M/F) | 9/11 | 11/9 |
| Weight (kg) | 61.2 ± 9.0 | 62.2 ± 7.6 |
| Height (cm) | 158.2 ± 6.7 | 160.4 ± 7.9 |









