Although clinical studies on the effect of the high-flow nasal cannula (HFNC) system on washout have been performed [1], the mechanism has only been estimated from studies of transtracheal oxygen therapy, which is quite a different system; thus, the mechanism for the washout effect remains to be clarified [1,2,3]. We used an artificial respiratory system model to evaluate the washout effect of the HFNC system.
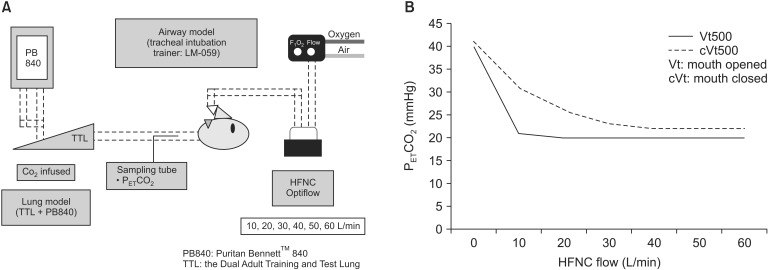
The experimental system (Fig. 1A) consisted of the Optiflow instrument (Fisher and Paykel Healthcare, Auckland, New Zealand), which was used as the HFNC system and was connected to the Dual Adult Training and Test Lung (TTL [lung model]: tidal volume, 500 ml; respiratory rate, 16 /min; inspiration time, 1.0 sec; Michigan Instruments Inc., Grand Rapids, MI, USA) via the LM-059 Koken Airway Management Model (airway model: upper airway volume, 200 ml) (Koken Co., Ltd., Tokyo, Japan). CO2 was infused into a respiratory lung model to maintain the end-tidal PCO2 (PETCO2) of 40 mmHg at the subglottic area. PETCO2 was measured by the Capnomac Ultima (Datex-Ohmeda GE Healthcare, Fairfield, CT, USA). The HFNC gas flow rate was varied from 10 to 60 L/min, and changes in PETCO2 were measured using open- and closed-mouth airway models.
HFNC gas flow of 10 L/min decreased PETCO2 to 20 mmHg in the open-mouth model and reached the minimum value. The reduction in PETCO2 was less with the closed-mouth model than that with similar HFNC flow in the open-mouth model, but PETCO2 reached 22 mmHg, which was near the minimum value with the open-mouth model at maximum HFNC flow of 60 L/min (Fig. 1B).
The washout effect of HFNC was efficient at an HFNC flow rate much lower than the flow rate generating positive end-expiratory pressure (PEEP) under an open-mouth condition. PEEP delivered by HFNC is reportedly 3–5 cmH2O with HFNC flow of 30–50 L/min and the mouth closed [4]. HFNC flow of 10 L/min with the mouth open would not generate sufficient PEEP to be clinically effective when the washout effect reaches its maximum. Fresh gas delivered by the HFNC is thought to wash out the exhaled CO2 efficiently from the upper airway through the oral cavity under the open-mouth condition. Fresh gas delivered by the HFNC under the closed-mouth condition must enter and exit via the nostrils, which is less efficient than the open mouth condition for washing out CO2 from the upper airway. Therefore, the washout effect of the closed-mouth model was less efficient than that of the open-mouth model, and the closed-mouth model needed more HFNC flow to reduce PETCO2.
One of our study's limitations was that the anatomical dead space was different from the actual value of 2 ml/kg [5]. Our model had 200 ml of anatomical dead space just in the upper airway, which would be about twice that of most adult patients. Dead space volume is thought to be a key factor influencing the washout effect; therefore, further study with a more sophisticated airway model is needed.
Another limitation of our study was that we were unable to record the flow and pressure patterns. The lung model we used was able to infuse CO2, but did not have sensors to measure pressure or flow. The association between the washout effect and PEEP generated needs to be assessed with a single model to estimate the respiratory physiological difference between HFNC flows, and a study with a lung model equipped with pressure and flow sensors needs to be performed.
The washout effect of an HFNC system was efficient with a relatively low flow rate, particularly with the open-mouth model. HFNC flow should be considered if there is a need for the washout effect or PEEP.