Anesthetic management for percutaneous computed tomography-guided radiofrequency ablation of reninoma: a case report
Article information
Abstract
A reninoma is an uncommon, benign, renin-secreting juxtaglomerular cell tumor that causes secondary hypertension in young patients. This hypertension is treated by tumor resection. Except for increased levels of plasma renin and angiotensin I and II, the other physical and laboratory examinations and electrocardiographs were within normal limits upon admission of a 19-year-old woman with a reninoma. For percutaneous computed tomography-guided radiofrequency ablation, general anesthesia was induced by thiopental sodium and rocuronium bromide and maintained with servoflurane (2-4 vol%) and oxygen. The operation ended uneventfully in hemodynamic stability. However, the patient complained of dizziness while sitting 5 hours after the operation, and hypotension was diagnosed. After aggressive normal saline (1 L) infusion over 30 min, the hypotension was corrected and the patient recovered without any other surgical complications. Here, we report the anesthetic management of a patient who underwent percutaneous computed tomography-guided radiofrequency ablation for reninoma destruction, particularly focusing on postoperative hypotension.
Hypertension is divided into primary and secondary hypertension. Uncontrolled hypertension leads to both endothelial damage and complications for the major organs, including the heart, kidney and central nervous system, which are fatal and life-threatening [1]. A reninoma, which is a renin-producing juxtaglomerular tumor, produces hypertension and hypokalemia via activation of the renin-angiotensin-aldosterone system [2]. In addition, uncontrolled, excessively increased renin induced by a reninoma leads to end-organ damage via hypertension. Because a total or partial nephrectomy for the removal of a hypertension-producing reninoma results in the conversion of increased blood pressure to normal blood pressure, a reninoma is a curable cause of secondary hypertension [2,3]. Thus, perioperative hemodynamic management is very important for patients who undergo surgery for the removal of a reninoma. In addition, to our best knowledge, case reports regarding the anesthetic management of a reninoma are very rare [4]. Here, we report the anesthetic management of a patient who underwent percutaneous computed tomography (CT)-guided radiofrequency ablation for the destruction of a reninoma, particularly focusing on postoperative hypotension.
Case Report
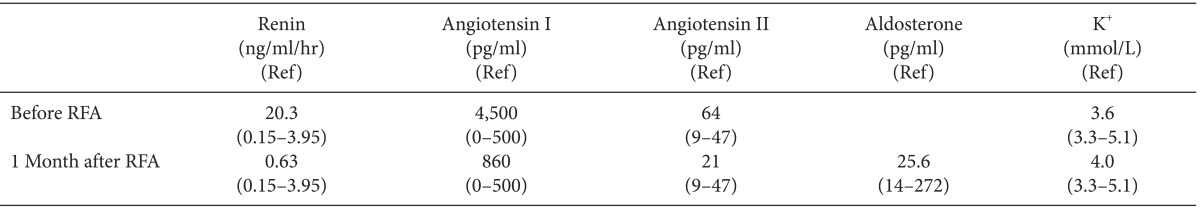
A 19-year-old female patient (body weight: 52.7 kg, height: 158.4 cm) was admitted to the university hospital for percutaneous CT-guided radiofrequency ablation of a reninoma in the lower pole of the left kidney. The patient had been taking the angiotensin II receptor blocker, candesartan (8 mg), or the combined calcium channel blocker and angiotensin II receptor blocker, amlodipine besylate (5 mg)/valsartan (160 mg), for 2 years to control what was presumed to be essential hypertension. The patient was diagnosed with essential hypertension 2 years prior because laboratory examinations including renal ultrasonography and cardiac echocardiography and renin, aldosterone and vanillylmandelic acid levels were all within the normal limits. However, when an abdominal CT was performed 1 year ago to confirm acute appendicitis, a small left renal mass (2 cm) was incidentally found and suspected to be benign. Four computed tomographies of abdomen were performed during follow-up to monitor the change in mass every 3 months for 1 year. The fourth follow-up CT showed that the size of the renal mass (2.3 × 1.8 cm) was slightly enlarged, and a radiologist recommended a biopsy of the mass to confirm whether the mass was malignant or benign. The results from the ultrasonography-guided renal biopsy of the renal mass indicated that the mass was a reninoma. At that time, blood examination of the patient indicated increased renin and angiotensin I and II levels, which are consistent with a reninoma (Table 1). The patient was scheduled to receive percutaneous CT-guided radiofrequency ablation under general anesthesia to destroy the reninoma in the left kidney.
The physical examination upon admission was unremarkable and did not show any end-organ damage due to hypertension, as is expected with well-controlled hypertension. The systolic and diastolic blood pressures, controlled by amlodipine besylate (5 mg)/valsartan (160 mg), were 110-131 and 62-82 mmHg, respectively, at the time of admission. In particular, a preoperative electrocardiogram, echocardiogram and chest posteroanterior radiography at the time of admission were all within the normal limits. She was taking amlodipine besylate (5 mg)/valsartan (160 mg) at the time of admission. She had a past anesthetic history of receiving general anesthesia for an appendectomy approximately 1 year prior and did not have any specific family history of anesthesia. Amlodipine besylate/valsartan was omitted on the day of the operation. No premedication was given for sedation. Anesthesia was induced with thiopental sodium (250 mg), servoflurane (6 vol%) and rocuronium bromide (50 mg), and the patient received oxygen (100%) through a facemask. Orotracheal intubation was performed using a reinforced endotracheal tube (internal diameter: 7.0 mm). The left radial artery was cannulated using a 20-gauge catheter to monitor intraoperative blood pressure. Anesthesia was maintained with servoflurane (2-4 vol%) in oxygen (2 L/min). The patient's position was changed from supine to prone, and the patient was transferred to the table for CT. Fig. 1 shows the intraoperative blood pressure and heart rate for every 5 min interval. When the first radiofrequency wave for percutaneous CT-guided radiofrequency ablation was given to the reninoma using an adjustable active tip (Proteus radiofrequency ablation electrode; STARmed, Ilsan, Korea), the patient's heart rate transiently increased from 74 beats/min to 104 beats/min. When the next nine radiofrequency waves were given using a 2.5 to 3 cm active tip, the intraoperative systolic and diastolic blood pressures and heart rate were 71-84, 77-86, and 80-92% of the preoperative value, respectively. In other words, the intraoperative blood pressure and heart rate were relatively stable. Heart rate and systolic blood pressure transiently increased from 65 beats/min to 102 beats/min and from 96 mmHg to 114 mmHg, respectively, when the last CT was taken 5 min before the operation ended. Normal saline (300 ml) was intraoperatively infused, and the intraoperative urine output was estimated to be 70 ml. The operation ended uneventfully, without any of the reported possible complications, including perirenal hematoma, hematuria, ureteropelvic junction obstruction and liver burn [5]. The total time for both anesthesia and operation was approximately 2 hours. The patient was extubated after adequate self-respiration was confirmed and clear consciousness was observed. The blood pressure and heart rate at extubation were maintained at preanesthetic levels. The patient was transferred to a recovery room using a movable bed, and the patient's position was changed from prone to supine in the movable bed. Fig. 2 shows that stable blood pressure and heart rate were maintained by the patient for approximately 70 min in the postanesthetic recovery room. The patient was transferred to the general ward 70 min after the operation. Fig. 3 shows the blood pressure and heart rate of the patient when in the general ward. As shown in Fig. 3, the patient had a stable blood pressure and heart rate for the initial 3 hours and 15 min spent in the general ward. Intravenous pethidine was given 3 hours after the operation to control postoperative pain. Normal saline (300 ml) was infused for 5 hours after the operation, and then the patient had a soft meal. When the patient sat up from a lying position to eat a soft meal approximately 5 hours after the operation, the patient complained of severe dizziness. At that time, the systolic/diastolic blood pressure and heart rate were 89/46 mmHg and 82 beats/min, respectively. Then, normal saline (500 ml) was intravenously infused over 15 min, which increased the systolic/diastolic blood pressure to 111/63 mmHg and significantly improved the dizziness of the patient. Then, the patient received an intravenous infusion of normal saline (1 L) at a rate of 120 ml/hr during the remaining time spent in the general ward. The blood pressure of the patient was stable throughout the remaining period in the general ward, but mild dizziness still occurred. The patient was uneventfully discharged from the hospital 18 hours after the operation. Although the patient's blood pressure was within the normal limits, the patient suffered mild orthostatic dizziness for approximately 4 weeks after discharge. Although she did not take antihypertensive drugs after the operation, her systolic and diastolic blood pressures at home were within the normal limits. At 1 month after the operation, the mild dizziness completely resolved and renin and angiotensin II levels were within the normal limits, but angiotensin I remained slightly increased (Table 1).
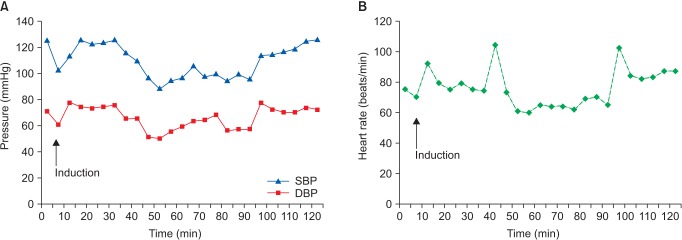
The systolic and diastolic blood pressures (A) and heart rate (B) during the operation. SBP: systolic blood pressure, DBP: diastolic blood pressure.
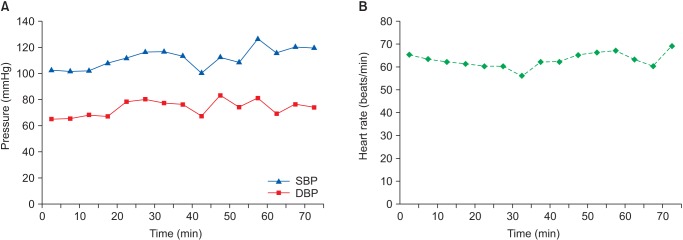
The systolic and diastolic blood pressures (A) and heart rate (B) in the postanesthetic care unit. SBP: systolic blood pressure, DBP: diastolic blood pressure.
Discussion
Reninomas are particularly prevalent in young females like this patient [2,3]. Uncontrolled increased plasma renin levels, as induced by a reninoma, activate the renin-angiotensin-aldosterone system, which leads to hypertension and hypokalemia [6]. Because the activated renin-anigotensin-aldosterone system induced by a reninoma is not normally controlled by a negative feedback system, an angiotensin receptor blocker or angiotensin-converting enzyme inhibitor is used to treat the hypertension observed with a reninoma [6]. In this patient, a calcium channel blocker was initially used to treat what was presumed to be essential hypertension, but the hypertension was not well controlled. Then, the calcium channel blocker was changed to either a combined drug with both a calcium channel blocker and an angiotensin II receptor blocker, or an angiotensin II receptor blocker alone, both of which worked well to control hypertension in this patient, compared with the calcium channel blocker alone. The incidence of retinopathy, papilledema, proteinuria, renal insufficiency and left ventricular hypertrophy, all associated complications of a reninoma causing uncontrolled hypertension, is reported to be 24, 6, 11, 3 and 7%, respectively [3]. Renin, the rate-limiting enzyme that hydrolyzes angiotensinogen to angiotensin I, has an elimination half-life of 80 min in the circulatory system [7]. Plasma renin is dramatically reduced by the surgical removal of a reninoma, which then leads to hypotension via decreased systemic vascular resistance [7]. In addition, the elimination half-life of amlodipine besylate and valsartan is 40-50 hours and 6 hours, respectively [8,9]. Thus, we omitted amlodipine besylate/valsartan treatment on the day of the operation because the drug might have augmented the hypotension observed after surgical removal of the reninoma.
It is important for the anesthesiologist to carefully monitor the intraoperative blood pressure and heart rate changes induced by surgical manipulation of a reninoma. To treat a severe blood pressure change induced by surgical manipulation, the anesthesiologist should prepare a vasodilator, a vasoconstrictor and an inotropic agent. We think that the minimally invasive percutaneous CT-guided radiofrequency ablation of a reninoma causes less hemodynamic change compared with an open or laparoscopic nephrectomy. We also believe that amlodipine besylate, with an elimination half-life of 40-50 hours, may partially contribute to the maintenance of a relatively stable blood pressure and heart rate during radiofrequency ablation [8]. As the reninoma in this patient was located in the lower pole of the left kidney, the percutaneous CT-guided radiofrequency ablation procedure itself may have had a negligible stimulating effect on the adrenal gland. However, as radiofrequency ablation of a reninoma adjacent to the adrenal gland stimulates the gland and leads to hypertensive crisis, we think that preparing to treat hypertensive crisis with a vasodilator during surgical removal of a reninoma is a reasonable method [10]. It has been reported that serum potassium levels were normalized within 7 days of the operation in a postoperative patient who underwent surgical removal of a reninoma [2]. In spite of the reninoma in this patient, preoperative serum potassium levels were within the normal limits. As this patient did not have secondary hyperaldosteronism due to the reninoma, serum potassium levels of the patient seemed to be within the normal limits during the perioperative period (Table 1) [3]. Initially, increased plasma renin levels induced by the reninoma lead to increased systemic vascular resistance, whereas surgical removal of a reninoma dramatically decreases plasma renin concentrations, leading to decreased systemic vascular resistance and relative hypovolemia compared with the preoperative state. The relative hypovolemia associated with decreased systemic vascular resistance seems to have been associated with the postoperative hypotension observed in this patient in the general ward. In addition, the relatively long-acting (elimination half-life: 40-50 hours) amlodipine besylate-induced vasodilation, which is not antagonized due to decreased renin levels in the postoperative patient, may have precipitated the observed hypotension. As 1 L normal saline, aggressively infused over 30 min, treated the postoperative hypotension in this patient, it seems to be a reasonable approach to aggressively infuse more fluids into patients in a relatively hypervolemic state during the postoperative period. In addition, the insertion of a central venous catheter or a Swan-Ganz catheter may be needed to evaluate the exact volume status of a patient with a reninoma during the intraoperative and postoperative periods. However, we did not insert these catheters because percutaneous radiofrequency ablation itself is a much less invasive procedure. In this patient, the postoperative blood pressure was within the normal limits, but the patient complained of mild dizziness upon standing. Blood pressure normalization induced by surgical removal of a reninoma may shift the autoregulation curve of cerebral blood flow from right to left [11]. Thus, even if the blood pressure of the patient is within the normal range postoperatively, the patient may feel mild dizziness until the central nervous system adapts to the left-shifted autoregulation curve of cerebral blood flow. In addition, this dizziness may be associated with the abolishment of the anti-ischemic effect of the angiotensin II receptor antagonist in the brain [11].
In conclusion, it is first very important to monitor the intraoperative blood pressure and heart rate carefully because surgical manipulation of a reninoma may produce severe hypertension similar to that produced by a pheochromocytoma [12]. Second, it would be better to aggressively infuse more fluids because both decreased systemic vascular resistance and relative hypovolemia induced by the surgical removal of a reninoma may produce lethal hypotension and severe orthostatic dizziness in the postoperative patient. Finally, it would be helpful to explain to the patient that dizziness transiently occurs in the postoperative period and eventually disappears.