Successful use of i-gel™ in a patient with tracheal stenosis undergoing Montgomery t-tube insertion
Article information
It is sometimes difficult to place Montgomery t-tube in the correct position through the tracheostomy site. Anesthesiologists may not be familiar with this device because of its infrequent use and unique design. Therefore, the patient may be exposed to conditions such as hypoventilation, asphyxia, and pulmonary aspiration. Here, we describe successful anesthetic management in a patient with tracheal stenosis undergoing Montgomery t-tube insertion using i-gel™ (Intersurgical Ltd., Wokingham, Berkshire, UK) and a Carlens (Y) adapter (Mallinckrodt™ Endobronchial tube accessory; Covidien, Mansfield, MA, USA).
A 37-year-old male with a body weight 60 kg was scheduled for insertion of a Montgomery t-tube after removal of tracheostomy tube. Six years ago, the tracheostomy tube was changed to a t-tube under general anesthesia. At that time, there were no problems. Four months previously, the patient's t-tube had been switched back to a tracheostomy tube to facilitate anesthesia.
Preoperatively the patient showed obtunded mental status, and had left hemiplegia. Laboratory findings were not specific. After transferring the patient to the operating room without premedication, vital signs were as follows: blood pressure 109/81 mmHg, heart rate regular at 71 beats/min, and oxygen saturation 100% on room air without breathing difficulty. Fentanyl (100 µg) was administered intravenously, and then 1.5 vol% sevoflurane inhalation was administered with spontaneous breathing of 100% oxygen. The intention was to insertion a t-tube under deep sedation without disrupting the patient's self respiration.
The surgeon attempted the t-tube insertion several times, but failed to place the t-tube appropriately. The surgeon requested general anesthesia to progress with the procedure because of the cough reflex and vigorous involuntary movements. Therefore, we decided to insert i-gel™ to secure the airway and to use a Carlens (Y) adapter to allow easy switching of the ventilation route between the i-gel™ and t-tube (Fig. 1). A standard endotracheal tube connector was used to connect the t-tube and corrugated tube.
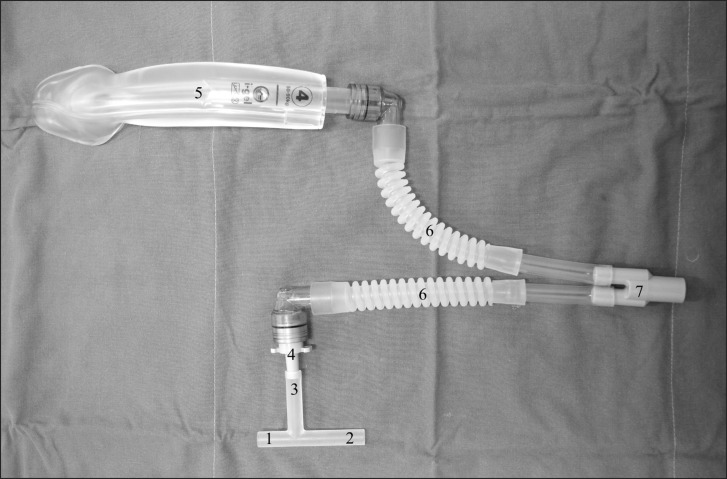
Photograph of a Montgomery t-tube and i-gel. (1) Short laryngeal part, (2) Long laryngeal part, (3) Extratracheal part, (4) Standard endotracheal tube connector, (5) i-gel, (6) Extension corrugated tube, (7) Carlens (Y) adapter.
For general anesthesia, remifentanil (target concentration: 2 ng/ml) and propofol (target concentration: 3 µg/ml) were infused intravenously using a target control infuser (Orchestra®; Fresenius Vial, Brézins, France). Muscle relaxation was induced by an intravenous bolus of atracurium (0.4 mg/kg). The i-gel™ (No. 4) was inserted and adequate ventilation was confirmed, although slightly elevated airway pressure was observed (peak airway pressure 24 cmH2O, VT 500 ml, ETCO2 35 mmHg). Ventilation was switched between the i-gel™ and t-tube by clamping the Carlens (Y) adapter appropriately. The t-tube insertion was finally completed within 30 min after these repeated attempts. Correct positioning of the inserted t-tube was assessed by confirming adequate ventilation of both sides by clamping either the i-gel™ or t-tube side of the Carlens (Y) adapter. Finally, a fiberoptic bronchoscope was inserted through the i-gel™ and t-tube patency was confirmed.
Several problems may be encountered during t-tube insertion; the airway is not fully under the control of anesthesiologist during insertion, and there may be kinking in the t-tube, leading to complete airway obstruction. To minimize the risk and manage the airway effectively, the anesthesiologist should first understand the unique design of the t-tube. Both the upper and lower ends of the intraluminal limb are open; loss of inspired gases through the upper end may lead to hypoventilation, and inadequate depth of anesthesia. In addition, unlike standard endotracheal and tracheostomy tubes, a t-tube does not have standard connectors [1]. Secondly, how to secure ventilation during t-tube placement remains controversial. Montgomery and Montgomery [2] suggested use of a Fogarty embolectomy catheter to block the upper open intraluminal end. Guha et al. [1] and Chung et al. [3] advocated insertion of a laryngeal mask airway before insertion of the t-tube. The Hebeler Safe-T-tube™ (Boston Medical Products, Westborough, MA, USA) is a modified t-tube that contains an internal balloon in the upper open intraluminal end [4].
In the present case, we inserted i-gel™ instead of Proseal™ laryngeal mask airway (PLMA) to secure the airway and for ventilation. The i-gel™ is easier to insert, less traumatic, requires less attempts for even emergency airway management, and provides a better fiberoptic view due to less epiglottic downfolding. The i-gel™ may also be superior to PLMA in preventing gastric aspiration by lower changes in position after insertion, and easier gastric tube placement [5]. We also used a Carlens (Y) adapter to make it possible to secure the airway as well as to switch ventilation between the i-gel™ and t-tube effectively. This can guarantee safe airway control even if t-tube insertion is delayed. Furthermore, we confirmed correct positioning of the t-tube by confirming adequate ventilation through both the i-gel™ and t-tube sides before reconfirming using fiberoptic bronchoscopy. Fiberoptic bronchoscopy via the i-gel™ can also be used to confirm correct positioning of a t-tube.
In conclusion, anesthesiologists should be familiar with dealing with airway diseases to prevent catastrophic hypoxic events. Use of i-gel™ with a Carlens (Y) adapter is effective for managing of patients with tracheal stenosis undergoing Montgomery t-tube insertion under general anesthesia.