|
 |
|
|
Central venous catheterization is frequently used as the procedure for preparation of major surgery, chemotherapy, total parenteral nutrition, and etc [1]. Usually, the catheterization sites are femoral vein, subclavian vein, and internal jugular vein (IJV). Because the right IJV has easy accessibility, and it gives direct route for right atrium [2], the right IJV is a popular site of central venous catheterization. Generally, landmark technique with a seeker needle is used for right IJV catheterization. It is a blind technique. Imagine if you are performing an IJV catheterization, and there is no blood aspiration in the seeker needle. What are the possible causes? And what do you do? Our case may offer a little help.
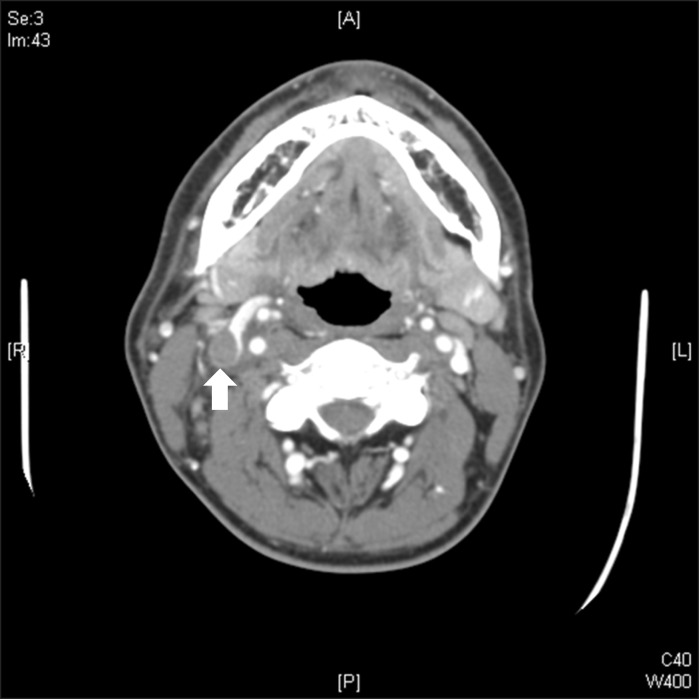
The patient was a 43 year-old male. He had been diagnosed with esophageal cancer and tracheal invasion (stage IVA, T3N1M1a) 2 years ago. Since then, he had 5 times of palliative chemotherapy and 6300 cGy of palliative radiotherapy on his neck. This patient needed general anesthesia for an Ivor-Lewis operation because of dysphasia and tracheo-esophageal fistula. In the operation room, we tried to find the right IJV with seeker needle aspiration. Despite of several trials, the aspiration failed. So, we used the ultrasound to find the right IJV. However, the ultrasound showed that the IJV lumen was distended with hypo-echoic thrombus or something, and flow was not detected in the IJV. Lastly, we cannulated the right femoral vein and the surgery proceeded. During the operation, we reviewed the neck CT images that were taken one and half years before the surgery when the patient had local infection on the right neck. Further, the CT review revealed that there was an occlusion in the right IJV (Fig. 1). We thought the cause of occlusion was tissue granulation or thrombosis. The radiologist's opinion was thrombosis or thrombophlebitis.
As we mentioned earlier, the IJV has easy accessibility, and the procedure has performed with blind technique traditionally. Khatri and Espinosa [1] shows 29 cases of difficult circumstances encountered on the right side, out of 320 cases. The ratio is 9%. Venous thrombosis was 9 cases out of 29 difficult cases.
IJV thrombus is caused by catheterization history of central venous catheter, malignancy, long term catheterization, thrombophillia, local infection, and spontaneous occlusion [3]. This patient had history of malignancy (esophageal cancer) and local infection on the neck. Those were maybe the cause of thrombosis, which made us be unable to cannulate with traditional landmark guided technique.
Ultrasound guided internal jugular catheterization has the advantage to detect anatomical variation or distortion, since ultrasound provides real time visualization. Ultrasound shows what is happened under the patient's skin. Ultrasound guided catheterization has higher success rate, lower attempt times, and lower complication rate than that of the traditional landmark guided catheterization [4,5]. In other words, if we use ultrasound guided technique, we can detect the difficult cases quickly and makes these to easier and safer cases. We revealed IJV thrombus on a CT review, after failure of several approaches. Because the patient had a history of local infection and malignancy, we should anticipate difficulty of the right IJV catheterization, and we should have to review the patient's neck before the attempting several approaches, but we did not. If the patient had a history of neck related disease and the right IJV catheterization is necessary, preoperative patient review is needed.
Therefore, we suggest the use of the ultrasound guided as a routine procedure while catheterization of the IJV. It makes catheterization easer, and lowers possible complications. Additionally, when the patient has a history of neck infection, malignancy or the prior catheterization of the IJV, a neck CT review is very helpful.
References
1. Khatri VP, Espinosa MH. A safer technique of internal jugular venipuncture: experience with 320 cases. J Cardiothorac Vasc Anesth 1994; 8: 663-667. PMID: 7880996.


2. Troianos CA, Jobes DR, Ellison N. Ultrasound-guided cannulation of the internal jugular vein. A prospective, randomized study. Anesth Analg 1991; 72: 823-826. PMID: 2035868.


3. Gbaguidi X, Janvresse A, Benichou J, Cailleux N, Levesque H, Marie I. Internal jugular vein thrombosis: outcome and risk factors. QJM 2011; 104: 209-219. PMID: 20974769.



4. Denys BG, Uretsky BF, Reddy PS. Ultrasound-assisted cannulation of the internal jugular vein. A prospective comparison to the external landmark-guided technique. Circulation 1993; 87: 1557-1562. PMID: 8491011.


5. Mallory DL, McGee WT, Shawker TH, Brenner M, Bailey KR, Evans RG, et al. Ultrasound guidance improves the success rate of internal jugular vein cannulation. A prospective, randomized trial. Chest 1990; 98: 157-160. PMID: 2193776.


- TOOLS