|
 |
|
|
Abstract
Central venous catheterization (CVC) can be difficult, especially with pediatric patients in critical care. Accessing the subclavian vein (SCV) can cause serious complications, including pneumothorax, arterial puncture, and hemothorax. Recently, the ultrasonographic (USG) technique has gained popularity, but its efficiency is not yet confirmed. Subclavian venous catheterization (SCVC) through the supraclavicular approach (SCA) with USG or accessing the brachiocephalic vein through the infraclavicular approach (ICA) has been reported in the past. A useful technique is reported that involves the use of a 40 mm probe rather than the usual 25 mm probe in order to confirm the location of the needle while successfully performing subclavian venous catheterization in pediatric patients weighing 1.1 kg to 15.0 kg.
Reasons to perform central venous catheterization with pediatric patients include fluid infusion, parenteral nutrition, sampling for laboratory investigation, hemodynamic monitoring, hemofiltration, or transfusion of blood components [1]. The most popular site has been either the femoral vein (FV) or the internal jugular vein (IJV), but recently, the IJV has been favored when ultrasound is used.
In 2002, the National Institute of Clinical Excellence (NICE) of the UK recommended the use of ultrasound during catheterization in pediatric patients [2]. Also, in a documented survey of administrators of pediatric anesthesia, 80% expressed a consensus for the need of ultrasonography, but the method was only practiced by 40% of those surveyed due to either a lack of expertise with the equipment or a lack of the equipment itself [3]. Reports on pediatric subclavian catheterization using ultrasonography have been rare, although reports on the supraclavicular approach [4], the axillary vein approach [5], and studies by Pirotte and Veyckemans [6] on the infraclavicular approach are available. However, the downside of Pirotte and Veyckemans's study was that real-time identification of the location of needle advancement was only possible in pediatrics weighing less than 10 kg, and was difficult in larger children.
A useful technique is reported of using a 40 mm probe rather than the usual 25 mm probe in order to confirm the location of the needle while successfully performing subclavian venous catheterization in pediatric patients weighing 1.1 kg to 15.0 kg.
A MylabŌäó 30 Gold (Esaote, Genova, Italy) and a linear probe (LA435: 6-18 MHz, Esaote, Genova, Italy) were used as the ultrasonographic equipment.
Performed in the intensive care unit (ICU), a blanket was placed under the calf of the patient in order to maintain dorsosacral position. A pad was placed beneath the shoulders for support in order to maintain a neutral position of the head or to prevent extension or flexion of the head. 1 mg/kg of ketamine was injected before the procedure for sedation, and after confirming sedation, the patient's head was rotated to the side opposite to the site of the procedure. A linear probe applied with non-sterilized ultrasonographic gel (Aquasonic®, Parker, New Jersey, USA) was placed in the cricothyroid membrane area to transectionally scan and confirm the anatomic structures of the internal jugular vein and carotid arteries before the procedure. The probe was then moved towards the patient's legs to confirm the merging of the internal jugular vein and the subclavian vein, clavicle, and pleural line. After confirmation of these anatomic structures, the site of the procedure was sterilely draped with 2% povidone iodine and covered with a sterile spread. 1 to 2 ml of 2% lidocaine was locally injected into the site of the procedure. A sterilized gel (Aquasonic®, Parker, New Jersey, USA) was applied to the probe and covered with a sterilized ultrasonographic drape. If the size of the subclavian vein identified through the probe was smaller than 2 mm, a 4 French catheter was used. If larger, a 5 French catheter (Pediatric two-lumen central venous catheterization set, Arrow® international, Pennsylvania, USA) was used (Fig. 1).
The internal jugular vein, carotid artery, subclavian vein, the clavicle and its shadow were identified by transectionally scanning, as done previously before sterile draping. After positioning the probe appropriately, the introducer needle was inserted in-plane. The needle was inserted while targeting the confluence of the internal jugular vein and the subclavian vein. After positioning the needle tip within the vessel, blood was aspirated in order to confirm its location, and a guide wire was inserted following typical catheterization procedures (Fig. 2). After insertion of the catheter, the internal carotid area was checked with the probe to see whether the catheter entered the internal jugular vein. After confirming no entry into the internal jugular vein, the catheter was fixed to the skin (Fig. 3).
Catheterization was carried out in the operating room (OR), and the patient was first put under general anesthesia and placed in a Trendelenburg position. The procedures of catheterization were carried out identically as done in the ICU.
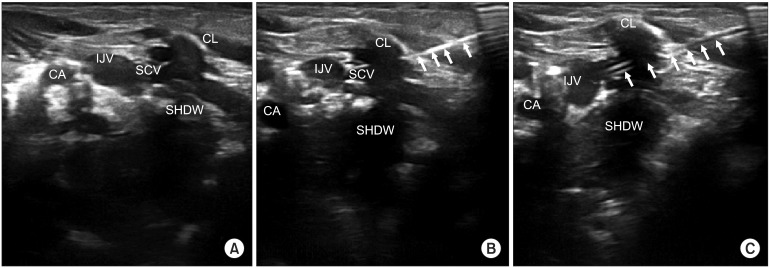
An identical method was used in a total of 11 pediatric patients. Demographic and procedural information are summarized in Table 1. Ages ranged from 2 days to 24 months, weighing 1,120 g to 12.4 kg, with height ranging from 34.2 cm to 91.7 cm. 3 procedures were carried out in the ICU, 5 in the OR, 2 in the neonatal intensive care unit (NICU), and 1 in the ward. Most were successful at the first attempt, although one patient carried out in the OR was successful upon the second attempt. A single attempt was defined as introducer-needle insertion into the skin, advancement into the vein, and blood aspiration. The number of attempts was increased if blood was not aspirated or the catheter insertion was unsuccessful despite aspiration, such that the introducer needle needed to be reinserted. Complications such as incorrect catheter location, arterial puncture, pneumothorax, or hemothorax did not occur in any patients.
The first patient in whom we ultrasonographically placed a subclavian vein catheter was a female pediatric patient weighing 5,150 g, born premature and being treated for a respiratory-related disease for over twelve months in the NICU and ICU. Due to extended stay in the hospital, peripheral venous access was difficult. Anesthesiology was consulted because many attempts of subclavian vein catheterization by cardiovascular and pediatric surgeons were unsuccessful, causing multiple hematomas and making of the anatomic landmark difficult.
There are a considerably large number of reports on ultrasound-guided central line placement in adult patients, but few on pediatric patients, for whom most procedures are carried out on the internal jugular vein. The only successful report of pediatric ultrasonographic-guided subclavian approach is by Pirotte et al. [6]. No reports have been reported in Korea.
According to NICE guidelines, the success rates of central venous catheterization through anatomic landmarks are high in adult and pediatric patients, but failure rates are as high as 35%, along with delayed management of complications such as arterial puncture, formation of arteriovenous fistula, pneumothorax, and nerve injury, thus encouraging the use of an ultrasonograph during internal jugular vein catheterization [2]. However, because there is no definite evidence on the efficacy of ultrasound-guided subclavian vein catheterization, it is difficult to make a positive conclusion. There are barely any cases considering ultrasound-guided subclavian vein catheterization in pediatric patients, although one case using a 25 mm linear probe through the supraclavicular fossa to access the axillary vein [5], or supraclavicularly to access the venous confluence [4] has been reported. However, for this particular case, it is difficult to say that a genuine central venous line was placed because the axillary vein was accessed. Also, a prolonged period of catheter placement in the supraclavicular fossa is prone to infection, because the catheter insertion point is close to the patients' mouth, thus causing management issues [7]. It is possible for the procedure to be carried out not only on the right side but also the left side, but a right-handed practitioner may be prone to difficulties, thus making handedness a problem [4].
Pirotte and Veyckemans [6] are the only ones to report a case of ultrasound-guided subclavian vein catheterization through an infraclavicular approach in pediatric patients. However, because a 25 mm hockey stick probe (HSP) was used, anatomical structures were detectable in real-time in small children. However, in larger children, this is not possible, and the needle has to be inserted after confirming the subclavian vein is limited to the clavicular area by marking the skin, making it difficult to observe the entire process.
On the other hand, a 40 mm linear probe was used in the current cases rather than the 25 mm HSP that Pirotte et al. used, making it possible to precisely observe not only the subclavian vein but other surrounding structures in children weighing over 10 kg, as well as premature infants weighing approximately 1 kg, while being able to observe the entire process of central venous catheterization. This method was successful on its first attempt in 10 out of 11 patients, and resulted in no complications regarding insertion. Due to its larger scanning range than the 25 mm HSP, the 40 mm probe provided more accurate scanning images of the surrounding structures, despite the posterior acoustic shadowing due to the clavicle.
In conclusion, if the method proposed here is carried out by a skilled anesthesiologist who is familiar with subclavian vein catheterization in pediatric central venous catheterization, ultrasound-guided central venous catheter insertion can be useful for premature infants, whose anatomical structures are difficult to identify, as well as relatively larger infants weighing over 10 kg, without any major complications. However, because this case was not a planned prospective study, more research is needed to prove its superiority to catheterization by anatomical indications.
References
1. ├ćitak A, Karab├Čc├╝oglu M, ├£├¦sel R, Uzel N. Central venous catheters in pediatric patients - subclavian venous approach as the first choice. Pediatr Int 2002; 44: 83-86. PMID: 11982878.


2. National Institute for Clinical Excellence. Guidance on the Use of Ultrasound Locating Devices for Placing Central Venous Catheters. Technlogy Appraisal Guidance No 49 2002;updated 2002; cited. Available from:
http://www.nice.org.uk.
3. Bosman M, Kavanagh RJ. Two dimensional ultrasound guidance in central venous catheter placement; a postal survey of the practice and opinions of consultant pediatric anesthetists in the United Kingdom. Paediatr Anaesth 2006; 16: 530-537. PMID: 16677262.


4. Rhondali O, Attof R, Combet S, Chassard D, de Queiroz Siqueira M. Ultrasound-guided subclavian vein cannulation in infants: supraclavicular approach. Paediatr Anaesth 2011; 21: 1136-1141. PMID: 21627714.


5. Breschan C, Platzer M, Jost R, Stettner H, Beyer AS, Feigl G, et al. Consecutive, prospective case series of a new method for ultrasound-guided supraclavicular approach to the brachiocephalic vein in children. Br J Anaesth 2011; 106: 732-737. PMID: 21414981.



6. Pirotte T, Veyckemans F. Ultrasound-guided subclavian vein cannulation in infants and children: a novel approach. Br J Anaesth 2007; 98: 509-514. PMID: 17332002.



7. Mermel LA, McCormick RD, Springman SR, Maki DG. The pathogenesis and epidemiology of catheter-related infection with pulmonary artery Swan-Ganz catheters: a prospective study utilizing molecular subtyping. Am J Med 1991; 91: 197S-205S. PMID: 1928165.


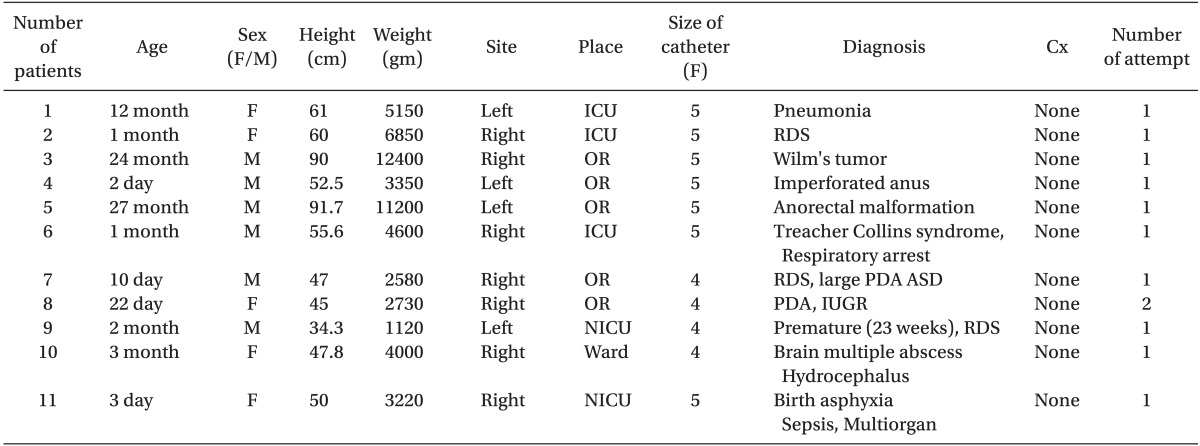
Fig.┬Ā1
Linear probe placement and needle puncture. (A) Schematic surface anatomy (lines are not drawn drawing the actual procedure). (B) Placement of the linear probe and its relation to the clavicle. (C) In-plane insertion of the introducer needle.
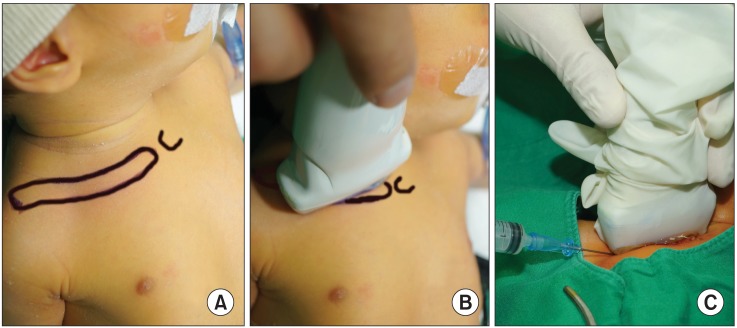
Fig.┬Ā2
Schematic diagram of the procedure and its related anatomy. IJV: Internal jugular vein, CLAV: clavicle, SCV: subclavian vein, CA: carotid artery, SHDW: acoustic shadow of clavicle.
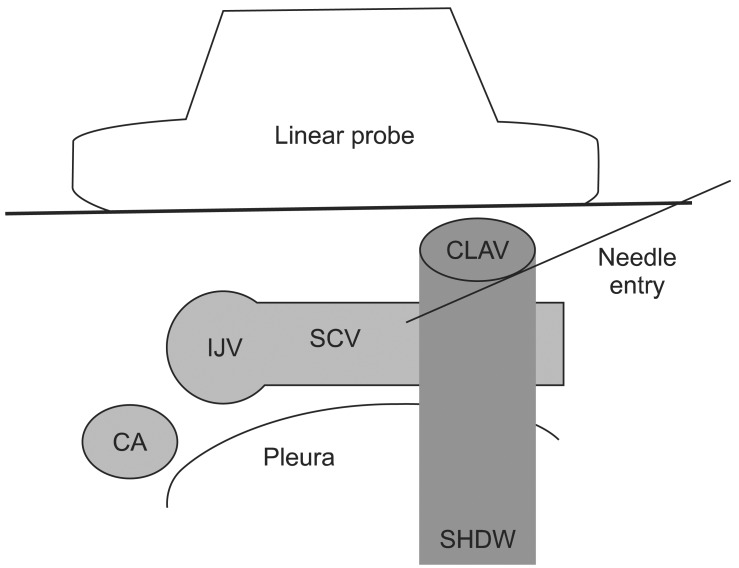
Fig.┬Ā3
Ultrasonographic images and techniques. (A) Confirmation of anatomical structure by a linear probe. (B) Introducer needle (arrows). (C) Catheter (arrows) in the subclavian vein. All related anatomical structures seen in one scanned image. IJV: internal jugular vein, CL: clavicle, SCV: subclavian vein, CA: carotid artery, SHDW: acoustic shadow of clavicle.
- TOOLS