Postoperative renal function in patients is unaltered after robotic-assisted radical prostatectomy
Article information
Abstract
Background
Pneumoperitoneum with an intra-abdominal pressure (IAP) of 14 mmHg is known to decrease renal function. Robotic-assisted radical prostatectomy (RARP) requires an IAP of more than 15 mmHg for operation. Therefore, we retrospectively investigated whether patients who underwent RARP experienced renal insufficiency during the postoperative period (at postoperative days 7 and 30).
Methods
One hundred patients who underwent RARP were enrolled in this study. Preoperative serum blood urea nitrogen (BUN) and serum creatinine (Cr) levels were measured. Creatinine clearance (CrCl) was calculated using the Cockcroft and Gault formula. CrCl was calculated at 1 day before surgery (baseline), 2 hr postoperatively, and at 1, 3, 7, and 30 days postoperatively (POD 1, POD 3, POP 7, and POD 30). Patients were assigned to abnormal CrCl (n = 52) or normal CrCl groups (n = 48) on the basis of these measurements.
Results
Significant inter-group differences in BUN, Cr, and CrCl were observed at all postoperative time points. BUN and Cr decreased significantly at postoperative 2 hr and POD 1, 3, and 7 versus baseline in both groups, whereas CrCl increased significantly at postoperative 2 hr and POD 1, 3, and 7 versus baseline in both groups. However, BUN, Cr, and CrCl were similar at POD 30 and preoperatively in the two groups.
Conclusions
RAPR, which requires an IAP of 15-20 mmHg for more than 4 hr, does not induce renal dysfunction during the postoperative period, and even in those patients with an abnormal CrCl.
Introduction
Increased intra-abdominal pressure (IAP) has long been associated with oliguria. A pneumoperitoneum at 7 mmHg is known to have no adverse effects on renal hemodynamics or excretory functions, but an IAP of 14 mmHg is known to decrease the glomerular filtration rate (GFR) by 53% and the renal blood flow (RBF) by 46%, and to impair urine output markedly by 10% and sodium excretion by 20% [1]. Nonetheless, many authors have insisted that laparoscopic surgery with intraperitoneal insufflation is associated with transient oliguria, but without any apparent sequelae [2-4].
A recent report demonstrated that erythrocyte velocities in cortical peritubular capillaries were significantly reduced when IAP was increased from 8 to 12 mmHg after 5 minutes of pneumoperitoneum, and that tubular damage of the subcapsular renal cortex, including tubular vacuolation, cell detachment, and tubular damage, developed 2 hours after starting laparoscopic surgery using a sustained pneumoperitoneal pressure of 20 mmHg. Accordingly, it was recommended that the duration of surgery should be considered in addition to IAP [5].
Robotic-assisted radical prostatectomy (RARP) requires long operation times (often longer than 4 hours) and an IAP of more than 15 mmHg with the patient in the deep Trendelenburg position. In patients that undergo RARP, urine output cannot be monitored due to urine spillover into the peritoneal space because of bladder neck dissection [6]. Therefore, in this retrospective study, we investigated whether patients that underwent RARP experienced renal insufficiency during the postoperative period (postoperative day 7 and 30: POD 7 and 30).
Materials and Methods
After obtaining Institutional Review Board approval, we enrolled patients that had undergone RARP from July 2007 to July 2009. Patients who had an ASA physical status higher than III were excluded. Patients with massive bleeding during the operation were also excluded. Remifentanil, propofol, and rocuronium were used as induction agents. Anesthesia was maintained with remifentanil (0.25-0.40 µg/kg/min) and desflurane (5-8 vol%). Intraoperative MAP and HR were within ± 20% of preoperative values. The bispectral index (BIS) was maintained at 50-60 during the operation. A robot system (Da Vinci robot system; Intuitive Surgical, Mountain View, CA) was used. A pneumoperitoneum was created by CO2 insufflation (15 mmHg) and patients were positioned in a 30° head-down position. The pneumoperitoneum was released after prostate removal.
Creatinine clearance (CrCl) was calculated using Cockcroft and Gault's formula at 1 day before surgery (baseline), postoperative 2 hr, and POD 1, POD 3, POD 7, and POD 30 [7]: CrCl = (140 - age) × ideal body weight / (serum creatinine × 72).
The normal CrCl range for men younger than 40 yr is 90-139 ml/min, and for men over 40 yr, normal values decrease by 6.5 ml/min for each decade of life. The normal CrCl ranges for men 40-49 yr is 83.5-132.5 ml/min; for men 50-59 yr is 77-126 ml/min; for men 60-69 yr is 70.5-119.5 ml/min; and for men 70-79 yr is 64-113 ml/min.
The CrCl value less than the minimum value was considered to be abnormal (e.g. CrCl < 83.5 ml/min in patients aged 40-49 yr). Patients were allocated either to the abnormal (n = 52) CrCl group or normal CrCl group (n = 48) using these ranges.
Serum BUN and Cr levels were checked on POD 1, 3, and 7. CrCl values were calculated. CrCl values were corrected for body surface area (BSA) using the following equation: for men, corrected CrCl = CrCl (as determined using the Cockcroft and Gault formula) × 1.73 m2/the patient's body surface area (BSA) [8].
Statistical analyses were performed using SAS v 8.1 (SAS Institute Inc., Cary, NC, USA) for Windows®. All results are expressed as mean ± SD or as numbers of patients. Student's t test, the Chi-square test, or the Mantel-Haenszel Chi-square test were used to determine significant inter-group differences. Results were analyzed using repeated-measures analysis of variance within each group. When a significant main effect was detected, contrast was used for post hoc testing. P value of < 0.05 were considered significant. A minimum sample size calculation was performed with the assumption that a 10% change in CrCl on postoperative 7 day in the abnormal CrCl group was clinically significant based on data from normal CrCl patients. A minimum of 45 patients in each group was necessary to detect a difference in postoperative renal function change using a two-tailed test with a probability of a type I error (α) of 0.05 and a probability of a type II error (β) of 0.1 (power 90%).
Results
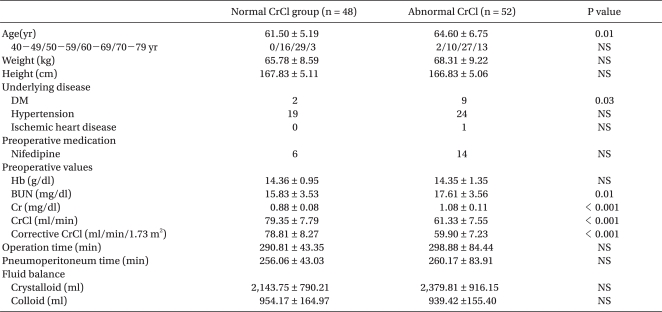
Patient characteristics and data from the perioperative period are summarized in Table 1. No significant differences were observed between the normal and abnormal CrCl groups except for age, a preoperative history of diabetes mellitus, and preoperative renal function. Patient age was significantly higher in the abnormal CrCl group than the normal CrCl group, but the age distribution was not significantly different between the two groups.
Significant inter-group differences in BUN, Cr, CrCl, and corrected CrCl were observed at all postoperative time points (Fig. 1). BUN and Cr decreased significantly at postoperative 2 hr and at POD 1, 3, and 7 versus baseline in both groups. CrCl and corrected CrCl were significantly higher at postoperative 2 hr and at POD 1, 3, and 7 compared with baseline in both groups. However, BUN, Cr, CrCl and corrected CrCl were similar to baseline at POD 30 in both groups.

Changes in BUN, Cr, CrCl, and corrected CrCl in the normal CrCl group and abnormal CrCl group. Normal CrCl group: patients with a normal CrCl preoperatively; abnormal CrCl group: patients with an abnormal CrCl preoperatively. *P < 0.05 compared with the preoperative value within each group, †P < 0.05 between groups.
The same pattern was seen for the patients in their 60 s (60-69 yr) of the abnormal and normal CrCl group (Fig. 2).

Changes in BUN, Cr, CrCl and corrected CrCl in the normal CrCl group and abnormal CrCl group aged 60-69 yr. Normal CrCl group: patients with a normal CrCl preoperatively; abnormal CrCl group: patients with an abnormal CrCl preoperatively. *P < 0.05 compared with the preoperative value within each group, †P < 0.05 between groups.
No major postoperative complication that required reoperation or postoperative intensive care occurred in both groups.
Discussion
The results of this retrospective study show that RAPR, which requires the patient to be in the deep Trendelenburg position with an IAP of 15-20 mmHg for more than 4 hr, does not induce renal dysfunction during the postoperative period.
Pneumoperitoneum has been previously shown to reduce GFR and RBF and to cause oliguria [1,9]. Although the mechanism underlying this phenomenon is largely unknown, direct compression of the renal parenchyma and renal vein, and the release of vasoconstrictors, such as vasopressin, angiotensin II, and catecholamines, have been well documented to reduce intraoperative urine output [10,11]. Even though oliguria is known to be transient and to resolve after desufflation in men [2-4], the use of vasodilators such as nitroglycerine [1], diltiazem [12], and nicardipine [6], and low doses of dopamine [13] has been suggested to prevent renal dysfunction during pneumoperitoneum without causing any hemodynamic derangement.
In a recent study, it was found that histologic changes such as tubular vaculoation, cell detachment, and tubular damage of the subcapsular renal cortex occurred after 2 hours of laparoscopic surgery in a porcine model (pneumoperitoneal pressure maintained at 20 mmHg) [5]. In this study, erythrocyte velocity in the cortical peritubular capillaries was found to decrease when the carbon dioxide pneumoperitoneum pressure was 12 mmHg; erythrocyte velocity improved rapidly when the pressure was reduced to 8 mmHg. Thus, those authors recommended that a pneumoperitoneal pressure of less than 8 mmHg be used for laparoscopic surgery to protect the renal microcirculation [5].
However, RARP is becoming a routine procedure for the treatment of prostate cancer, and requires marked head-down tilting and an IAP of more than 15 mmHg for more than 4 hours. An extreme head-down tilt markedly increases the central venous pressure and it may further compromise renal perfusion, and it is also associated with a 40-50% decrease in cardiac output during laparoscopic procedures, and even at an IAP of 10-12 mmHg [14,15]. Furthermore, almost all patients that undergo prostate resection are over 40 years old and nephrosclerosis and glomerulosclerosis occur to some extent in most people after the fourth decade of life, which reduces the number of functional nephrons by ~10% for each 10 years of age after 40 [16]. Thus, the effect of pneumoperitoneum during RAPR on renal function might be different from other forms of laparoscopic surgery. Postoperative renal function should be evaluated in patients undergoing RAPR and the need for active treatment to prevent renal dysfunction should be reexamined.
In the present study, renal function profiles were evaluated as CrCl. Calculated and corrected CrCl levels were used rather than measured CrCl levels to estimate GFR, because measured CrCl levels are inaccurate and imprecise due to the inaccurate collection of urine samples. Calculated CrCl has been reported to provide a better estimate of GFR and a corrected CrCl, which corrects for BSA levels, has been reported to provide more accurate estimations of GFR than measured CrCl when compared with inulin clearance [17-19].
Immediate postoperative renal dysfunction was expected in patients undergoing RAPR. Interestingly, however, BUN and Cr decreased while CrCl and corrected CrCl increased significantly versus baseline at postoperative 2 hr and also at POD 1, 3, and 7 in both normal and abnormal CrCl groups. This finding is consistent with previous laparoscopic studies. Nishio and colleagues [20] demonstrated that urinary output decreased significantly during insufflation and increased significantly after desufflation during laparoscopic adrenalectomy. Other clinical and animal studies have shown that renal function profiles using CrCl or estimated GFR levels were significantly or substantially elevated after laparoscopic surgery (an IAP of 15 mmHg for more than 3 hr) on POD 1 and 3 [1,2,6].
These renal function profiles returned to the preoperative values on POD 30 in all the patients. Even patients with abnormal preoperative CrCl levels were found to have a similar renal function on POD 30 compared with their preoperative values. In our study, no patient showed postoperative renal insufficiency or renal failure. In an animal study, it was found that pigs exposed to a CO2 pneumoperitoneum at 20 mmHg for 6 hr to mimic a complex laparoscopy had elevated levels of N-methyl-β-D-glucosaminidase in their urine. However, GFRs were found to have returned to the preexposure levels when reassessed 1 week after pneumoperitoneum, even in swine with chronic renal failure [21].
Our findings suggest that postoperative renal function in patients who underwent RARP is unaltered and the administration of intraoperative vasodilators is not required to prevent renal dysfunction for laparoscopic procedures lasting more than 2 hr (up to 4 hr) at an IAP of 15 mmHg. However, in this retrospective study, we excluded the patients with an ASA physical status class III or more, and the severity of the patients' renal insufficiency was not evaluated. Therefore, it is unclear if our findings can be extrapolated to patients with severe renal insufficiency and hemodynamic derangement.
In summary, renal function was not reduced on POD 7 and 30 in patients who underwent RARP, and even in patients with an abnormal preoperative CrCl level.
Notes
This study was supported by grants from the Institute of Medical System Engineering (iMSE) in the Gwangju Institute of Science and Technology (GIST), Republic of Korea.