Comparison of surgical condition in endoscopic sinus surgery using remifentanil combined with propofol, sevoflurane, or desflurane
Article information
Abstract
Background
Various maneuvers are commonly used to achieve the ideal operative field necessary for successful endoscopic sinus surgery (ESS). There are a few contradictory reports on this subject and the consensus is that propofol anesthesia results in a better or similar surgical field and less or similar amount of bleeding than volatile anesthesia. The aim of this study was to compare the surgical field in patients in whom intravenous anesthesia is used as opposed to balanced general anesthesia.
Methods
Sixty patients undergoing ESS were randomly assigned into three groups, each of which used a different type of anesthesia: propofol/remifentanil (PRO/REM) group, sevoflurane/remifentanil (SEV/REM) group, and desflurane/remifentanil (DES/REM) group. We aimed to maintain the intraoperative mean blood pressure (MBP) at 65 mmHg and the heartrate (HR) at about 75 beats per minute. The quality of visibility of the surgical field was graded, using a validated scoring system, 60 minutes after the start of the operation.
Results
All groups had a similar MBP and mean HR at 60 minutes after the operation started. There was no significant differences among the three groups for surgical grade score (P = 0.83).
Conclusions
In this comparative study of three anesthetic combinations (PRO/REM, SEV/REM, and DES/REM) in patients undergoing ESS with controlled BP and HR, we did not observe any significant differences in the surgical grade scores.
Introduction
Due to the nature of the space in which endoscopic sinus surgery (ESS) is performed, even a little bleeding can adversely affect the surgeon's ability to visualize the region to be operated. Increased bleeding results in further difficulties in obtaining an adequate surgical field. As a result, the operation become more difficult and takes more time.
Various attempts have been made to improve the surgical field, such as positioning the patient in reverse Trendelenburg, decongesting the nose, infiltrating the lateral nasal wall with lidocaine and epinephrine, or using the hypotensive anesthesia technique [1,2].
There are a few contradictory reports on this subject but the consensus is that propofol anesthesia results in a better or similar surgical field [2,3] and less or similar amount of bleeding [2,4-6] than does volatile anesthesia. The aim of this study was to either confirm or repudiate the findings of previous authors and to investigate the effects of the three types of anesthesia in the surgical field of ESS, with total intravenous anesthesia (TIVA) with propofol/remifentanil, balanced general anesthesia with sevoflurane/remifentanil and desflurane/remifentanil under controlled mean blood pressure (MBP) and heart rate (HR).
Materials and Methods
With approval from the hospital ethics committee, we recruited 60 patients between the ages of 18 and 60 years who were American Society of Anesthesiologists physical status I and II and were also undergoing elective ESS. The patients were randomly assigned to one of three protocols and then underwent ESS under general anesthesia performed by a single surgeon at a hospital-based surgery center. The exclusion criteria included: body mass index (BMI) ≥ 30.0, history of alcohol and drug abuse, pregnancy, medication known to affect minimum alveolar anesthetic concentration (MAC), communication problems, and allergic fungal sinusitis or nasal polyposis (>3 polyps). Allergic fungal sinusitis or nasal polyposis increases inflammation and vascularity; both of these conditions are related to a higher surgical grade score. Written consent for the study was obtained from each patient. Randomization was achieved through selection of an unmarked envelope revealing the study path immediately before induction. Patients were assigned by block randomization to receive one of three anesthetic combinations (n = 20 patients each group): TIVA with propofol/remifentanil group (PRO/REM), balanced general anesthesia with sevoflurane/remifentanil group (SEV/REM) and desflurane/remifentanil group (DES/REM).
Thirty minutes before surgery, patients were given 0.2 mg glycopyrrolate intramuscularly. The clinical monitoring included electrocardiography, pulse oximetry, temperature, noninvasive blood pressure, and bispectral index monitor (A-2000 BIS XP, Aspect Medical System Inc., Norwood, MA, USA). The patients in the three groups received target concentration infusion (TCI, Orchestra®, Base Primea, Fresinius Vial, France) for maintenance of anesthesia. The patient's age and weight were entered into the TCI unit so that the target propofol and remifentanil concentrations could be set. Remifentanil TCI was started at 3 ng/ml. After remifentanil reach target concentration, the inhalation groups (SEV/REM and DES/REM) received propofol (2.0 sevoflurane 2.0 mg/kg) for induction followed by sevoflurane 2.0 vol% or desflurane 5.0 vol%). The PRO/REM group received propofol (initial target plasma concentration, 4.0 µg/ml) for maintence of anesthesia. During induction, the patients were ventilated with 100% oxygen. After loss of the eyelash reflex and verbal response, a bolus dose of rocuronium 0.7 mg/kg was administered for muscular paralysis. The trachea was intubated and the lungs were mechanically ventilated to achieve an end-tidal CO2 concentration of 25-35 mmHg with 50% N2O in oxygen. The end-tidal sevoflurane and desflurane concentrations, as well as the propofol and remifentanil maintenance target infusions were adjusted to maintain an adequate depth of anesthesia, as judged by clinical signs and hemodynamic responses to surgical stimuli, and to maintain blood pressure.
In the inhalation group, anesthesia was maintained with sevoflurane (end-tidal concentrations of 0.8-2.0%) or desflurane (end-tidal concentrations of 3.0-6.0%). The target-controlled infusion rate of remifentanil was at 1-3 ng/ml. In the PRO/REM group, propofol was administered via target-controlled infusion to 2-4 µg/ml and remifentanil infusion was set at 1-3 ng/ml.
We aimed to maintain the intraoperative MBP at 65 mmHg, HR at about 75 beats per minute and bispectral index value from 40 to 60. If the systolic blood pressure fell below 75 mmHg, a 5 mg bolus of intravenous (IV) ephedrine was given. No other drugs were administered to control blood pressure.
The propofol, sevoflurane, or desflurane was discontinued and remifentanil and N2O were stopped right after the termination of the surgery. Once respiration and response to verbal command were adequate, patients were endotracheally extubated.
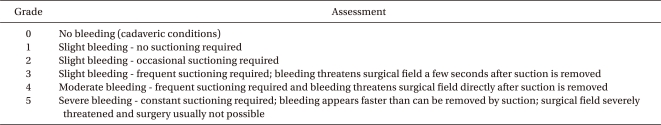
In most cases, the syringe device for the propofol infusion were set up and present even when the patient was receiving inhalation anesthesia. This was to prevent surgeons from knowing which kind of method of anesthesia we are providing. After 60 minutes from the start of the operation, the surgeon provided numerical assessments of the operative conditions (primarily in relation to the amount of bleeding and its effect on visibility), and identified the sinus being treated. Surgical field was scored using the scale that was originally described by Fromme et al. [7] and then subsequently adapted by Boezaart et al. [8]. Appendix 1 shows the surgical grade scoring system designed specifically for use with ESS. In addition, we documented data regarding the extent of the surgery, the Lund-Mackay (LM) computed tomography (CT) score (Appendix 2), the total operating time, total anesthetic time, surgical condition, volume of crystalloid given and the use of ephedrine.
Data were analyzed with the use of SAS® (version 9.2, SAS Institute, Cary, NC, USA). After normality test was conducted, age, volume, initial HR, BMI, operation time and anesthesia time, not showing normal distribution were examined with Kruskal-Wallis test, a non-parametric one-way ANOVA test and MBP at initial, 30 minutes and 60 minutes, HR at 30 minutes and 60 minutes with normal distribution were tested with ANOVA. As scores are ordinal scales, non-parametric analysis was performed, and Kruskal-Wallis test was conducted to determine differences of scores among the drugs. The friedman test was used to determine differences of scores following use of ephedrine and the spearman correlation test was performed to analyze the correlations of age, use of ephedrine and scores of each group, by using Fisher's exact test. Comparisons were considered significant if P < 0.05.
Results
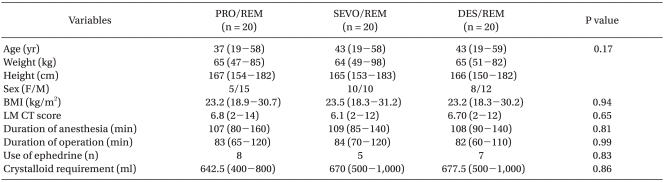
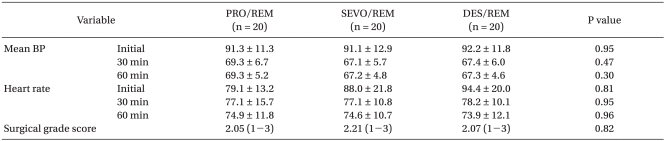
Among the three groups, there were no significant differences in the mean total surgical time, nor were there significant differences in the characteristics of the patients, duration of operation, crystalloid requirement and use of ephedrine (Table 1). The three groups were similar in terms of their mean LM CT score (Table 1). None of the groups had significant differences in MBP and HR throughout the operation (Table 2). There were no significant differences among the three groups for surgical grade score (Table 2).
Discussion
To obtain a relatively bloodless field in order to optimize visibility for the surgeon, various maneuvers are commonly used [1,2,9-12]. The concept that anesthesia may contribute to blood loss during surgery is not new; Stankiewicz [13] reported that estimated blood loss was less in patients receiving local anesthesia as opposed to general anesthesia for endoscopic sinus surgery. Surgical condition has been reported, in a statistically significant manner, to be influenced by the type of anesthetics, BP and HR [2,9,10,12]. Traditionally, controlled hypotension is required to reduce the amount of blood loss and provide a dry surgical field, but can cause some problems such as rebound hypertension, reflex tachycardia, vasodilation, organ ischemia and myocardial depression field for ESS. Further, the surgical field has not always been improved as a consequence of MBP reduction [7] and induced hypotension [8,14,15].
Desflurane is known to cause a moderate rise in heart rate, central venous pressure, and pulmonary artery pressure which often does not become apparent at low doses. Cardiac output remains relatively unchanged or slightly depressed with desflurane at 1-2 MAC. Sevoflurane decreases systemic vascular resistance and arterial blood pressure slightly less than desflurane. Sevoflurane causes little, if any, rise in heartrate, and patient's cardiac output is not maintained as well as it is with desflurane [16]. Despite the slightly different cardiovascular system effects between these two inhalation agents, it is reported that desflurane, sevoflurane or isoflurane combined with remifentanil provided adequate induced hypotension (MAP 60-70 mmHg) and similar surgical conditions during tympanoplasty [17]. Similarly, there are no significant differences between SEV/REM and DES/REM groups in our study.
Inhalation agents have a dose-dependent decrease in systemic vascular resistance which leads to the reduction in blood pressure [16]. This property can cause a capillary bleeding despite that systolic blood pressure is low [9]. Wormald et al. [3] suggest that the improvement in surgical grade in the TIVA group appears to be related to an overall reduction in MAP and the patients in the sevoflurane group require more significant reductions in MAP in order to obtain an equivalent surgical field grade score, due to the vasodilatory effect which results in capillary bleeding.
Some studies have reported that propofol produces a better surgical field than inhalational anesthesia in patients undergoing ESS, irrespective of the complexity of surgery [2,3,9,18]. Propofol and opioids can depress cerebral blood flow in parallel with depression of cerebral metabolic rate [19]. Thus, reduction of cerebral blood flow with propofol would be expected to decrease blood flow to the ethmoid, sphenoid, and frontal sinuses and potentially diminish bleeding related to arterial inflow.
It is well-known that remifentanil used in all three groups in our study provides excellent intraoperative analgesia and favors prompt emergence without prolonged respiratory depression [6,20,21]. The advantage of remifentanil in ESS is that they lower blood pressure through a decrease in cardiac output without peripheral vasodilatation, which results in reducing the capillary bleeding and at the same time provides good endoscopic surgical conditions [6]. The most frequent adverse events encountered when using remifentanil for IV anesthesia are hypotension during induction and hypotension and/or bradycardia during maintenance [10,22]. Although bradycardia is a recognized side effect of remifentanil [22], this was not a significant side effect in our study. In order to maintain controlled BP and HR, we did not allow the concomitant use of other cardiovascular medications other than ephedrine.
In this study, the PRO/REM group showed no statistical difference in using cardiovascular medication (IV ephedrine in this study) when compared with the other groups (P = 0.83). Some needs were almost entirely due to the higher incidence of hypotension during the induction and the early maintenance phase of anesthesia (i.e., after position change and before the start of surgery). In such cases, no significant effect was noted with surgical grade score (P = 0.62).
Severity of chronic sinusitis is one of the factors which can affect surgical condition. Ahn et al. [4] reported that the patients with a low-LM score (≤12) were not affected by anesthetic methods. In contrast, TIVA resulted in a better surgical condition than conventional balanced anesthesia in the patients with a high-LM score (>12). In our study, there were no statistically significant differences in MBP (P = 0.30), HR (P = 0.96), and surgical grade scores (P = 0.82) among the three groups at 60 minutes after the initiation of the operation and this result may be due to low LM scores in all three groups.
The operation time has also been reported as having an effect on the surgical field [3], which may be due to an increase in vasodilation with operation time as well as an increase in the surface area of the damaged tissue. In our study, we compared the surgical field score at 60 minutes after the initiation of the operation in all three groups to minimize the operation time factor which may contribute to the surgical field condition.
In conclusion, among three different anesthetic combinations (PRO/REM, SEV/REM, and DES/REM) in patients undergoing ESS with controlled BP and HR, we did not observe any significant differences in the surgical grade scores.
Appendices
Appendix 1
Surgical Grade Scoring System Designed Specifically for Use in Endoscopic Sinus Surgery
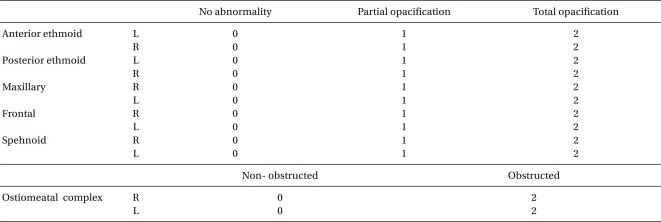
Appendix 2
Lund-Mackay Computed Tomography Staging System