|
 |
|
|
Abstract
Background
Coughing is a side effect of opioids that is rarely studied. Here, we evaluated the incidence of remifentanil induced coughing during anesthesia induction in an attempt to identify its risk factors and to examine the preventive effects of lidocaine and salbutamol.
Methods
A total of 237 patients scheduled to undergo general anesthesia were allocated randomly into three groups. Group C received no medication, while Group L received 2% lidocaine at 0.5 mg/kg intravenously 1 minute prior to remifentanil infusion and Group S inhaled one metered aerosol puff of salbutamol 15 minutes prior to entering the operating room. Remifentanil was infused at 5 ng/ml by target controlled infusion and coughing was measured for five minutes and graded as none, mild, moderate, or severe based on the number of coughs.
Results
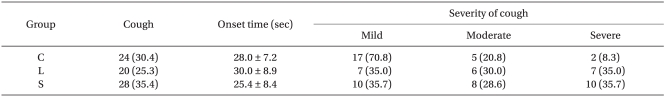
The incidences of coughing were 30.4%, 25.3%, and 35.4% in Groups C, L, and S, respectively. The incidences, onset times, and severity of coughing did not differ significantly among groups. In addition, multivariate analysis showed that non-smoking and a lower body weight were risk factors of remifentanil-induced coughing (odds ratio, 8.13; P = 0.024, 1.11, and 0.004, respectively).
Remifentanil is a fentanyl derivative that is an ultra-short acting, nonspecific esterase-metabolized, selective mu-opioid receptor agonist commonly administered in combination with volatile or intravenous anesthetic agents [1,2]. However, like other opioids, remifentanil can provoke various side effects such as nausea and vomiting, hypotension, bradycardia, muscle rigidity, and shivering [3]. Coughing immediately after injection is also commonly encountered, but has rarely been investigated. However, during the induction of anesthesia, coughing can increase intracranial, intraocular, and intra-abdominal pressures [4] and therefore be dangerous in patients with high ocular or intracranial pressure or a full stomach. The injection of opioids during the induction of anesthesia has also been reported to cause explosive spasmodic coughing severe enough to result in morbidity [5].
The incidence of fentanyl induced coughing has been reported to be 28-45% at co-induction [6], and 0.5 mg/kg of intravenous lidocaine or 1 metered aerosol puff of salbutamol have been reported to effectively reduce the incidence of fentanyl-induced coughing [6-8]. However, few studies have been conducted to evaluate remifentanil-induced coughing. Therefore, in the present study, we investigated the incidence and risk factors of remifentanil induced coughing during the induction of anesthesia and sought to determine whether pre-treatment with lidocaine or salbutamol can reduce the incidence and severity of coughing.
This study was approved by the Institutional Review Board and written informed consent was obtained from all patients. A total of 258 patients with an American Society of Anesthesiologists physical status of I or II aged 18-65 years and scheduled to undergo general anesthesia for elective surgery were included in this study. The following exclusion criteria were applied: a history of chronic pulmonary disease, cardiovascular disease, or an upper respiratory tract infection during the previous two weeks. Patients were randomly allocated to one of three groups, Group C (the control group, n = 79), Group L (the lidocaine group, n = 79), or Group S (the salbutamol group, n = 79), using a computer generated table of random numbers. No differences in patient characteristics were evident among the three groups (Table 1).
The evening before surgery, an 18-gauge cannula was inserted into a forearm and connected to a T-connector for drug injection. No premedication was administered prior to surgery. In the operating room, all patients were monitored by electrocardiography, non-invasive blood pressure, pulse oximetry, and capnography. One minute before the remifentanil injection, Groups C and S received 2 ml of 0.9% normal saline and group L received 0.5 mg/kg of 2% lidocaine over five seconds. Group S inhaled one metered aerosol puff of salbutamol 15 minutes prior to entering the operating room. Total intravenous anesthesia was conducted for anesthesia. Propofol and remifentanil were administered using a target-controlled infusion pump (Orchestra®, Fresenius Vial, France).
First, remifentanil was started at an effect site concentration of 5 ng/ml (Minto's pharmacokinetic model, maximum flow rate 450 ml/hr) and the patient reaction was observed for five minutes. The target concentration of remifentanil was reached within one minute in all patients. Coughing was observed by an anesthesiologist who was unaware of the type of medication administered. Coughing was graded as none, mild, moderate, or severe by counting coughs (mild: 1-2, moderate: 3-4, and severe: 5 or more). After five minutes of observation, propofol was started at an effect site concentration of 4-5 ┬Ąg/ml. Rocuronium (0.6 mg/kg) was injected after loss of consciousness and the patients were then intubated. O2 and air were administered at 2 L/min in a 1 : 1 ratio throughout anesthesia.
Systolic blood pressure (SBP), heart rate (HR), and SpO2 were recorded at five time points: before remifentanil injection (baseline), at the start of remifentanil injection (0), and at 1, 2, and 3 minutes after starting remifentanil injections.
A previous study revealed that the frequency of remifentanil induced coughing is 27.6% [7]. Accordingly, we assumed that a 20% decrease in the frequency of coughing after each treatment with a power of 80% and alpha error of 0.05. The calculated minimum sample size required was 68 patients per group.
Coughing incidence and severity were compared using a chi-square test or the Kruskal Wallis test. The patient characteristics in the three study groups were compared by one-way analysis of variance or by using the chi-square test. To identify the risk factors of remifentanil induced coughing, we used multiple logistic regression analysis. Statistical analysis was conducted using SAS (version 9.1.3, SAS Institute, Inc., Cary, NC, USA). Statistical significance was accepted for P values of <0.05.
A total of 258 patients that underwent surgery between January 2009 and August 2009 that also fulfilled the inclusion criteria were considered. Overall, 21 patients were excluded; therefore, 237 patients were enrolled, 79 in Group C, 79 in Group L, and 79 in Group S.
The frequencies of coughing were 30.4% in Group C, 25.3% in Group L, and 35.4% in Group S. No significant inter-group differences were observed in the frequency, onset time, or severity of coughing (Table 2). The hemodynamic variables (SBP, HR, and SpO2) were similar among the three groups (P = 1.00, except HR: P = 0.64). Multivariate analysis showed that non-smoking (odds ratio [OR], 8.13; 95% confidence interval [CI], 1.32-50.14; P = 0.024, frequencies of coughing; 59/72 patients; 81.4%) and a low body weight (OR, 1.11; 95% CI, 1.03-1.19; P = 0.004, body mass index < 22.5 kg/m2) were related to the risk of remifentanil-induced coughing.
The frequency of remifentanil-induced coughing was 30% and no differences in the frequency, onset time, or severity of coughing were observed among groups. However, a non-smoking status and a lower body weight were found to be risk factors of remifentanil-induced coughing.
Kim et al. [7] reported that 27.6% of patients experienced coughing after a remifentanil injection, which concurs with the results of our study. Our findings are also comparable with the reported incidences of fentanyl induced coughing (28-43%) [6-8]. Various mechanisms have been proposed to explain opioid induced coughing. Opioids are known to enhance vagal activity by inhibiting central sympathetic outflow [9], and it has been suggested that the vagal-dependent pathway triggers coughing and reflex bronchoconstriction [10]. Another possible mechanism is muscle rigidity provoked by opioid administration, which causes the abrupt adduction of vocal cords or supraglottic obstruction by soft tissues [11].
The suggested mechanism of intravenous lidocaine on opioid induced coughing involves its depressing brain stem function or the anesthetization of peripheral cough receptors in the trachea and hypopharynx [8,12]. In a previous study, 0.5 mg/kg of intravenous lidocaine was found to effectively suppress remifentanil-induced coughing [7]. However, in the present study, we found no evidence of an antitussive effect of lidocaine. Yokioka et al. [13] reported that the effective dose of lidocaine for suppressing fentanyl-induced coughing was 2 mg/kg, whereas 1.5 mg/kg lidocaine was found to be effective in another report [14]. Our findings suggest that lidocaine doses exceeding 0.5 mg/kg are required to prevent remifentanil induced coughing.
Salbutamol is a bronchodilator that is commonly used in the operating room to treat bronchospasm. In a previous study, one metered aerosol puff of salbutamol was found to prevent fentanyl-induced coughing [6]. The reason for the discrepancy with our results is unclear, although it may be due to our use of remifentanil rather than fentanyl. Remifentanil has more frequently been reported to provoke muscle rigidity during anesthesia than other types of opioids [15]; therefore, one MTD of salbutamol may have been insufficient to prevent remifentanil induced coughing. However, no systematic comparative research has been conducted on the two opioids to evaluate the frequency of coughing or the severity of muscle rigidity. Another possible reason for this discrepancy between results is that although beta agonists such as salbutamol have a bronchoprotective effect in hyper-reactive airways, they have minimal effects on normal airways [16]. In the present study, we excluded patients with pulmonary conditions such as asthma, COPD, or upper airway infection, which might explain why pre-treatment with salbutamol did not effectively prevent remifentanil-induced coughing in the present study.
In a previous study, age and non-smoking were found to be associated with remifentanil-induced coughing [7], whereas in the present study, non-smoking and a low body weight were found to be risk factors of remifentanil-induced coughing. The reason for this reduced incidence among smoking patients may be explained by the inhibition of C-fiber activity in the sensory nervous system of the lower respiratory tract by nicotine [17]. Furthermore, exposure to tobacco smoke can induce cough receptor desensitization within the airway epithelium [18]. Regarding the aforementioned age effect, the majority of our patients were between 26 and 48 years old. As a result, the age distribution of our cohort probably prevented identification of an age related coughing risk.
In the present study, a low body weight was found to be associated with remifentanil-induced coughing, and few clinical studies have reported that body weight affects cough reflex sensitivity, although one study mentioned that cough sensitivity is reduced in female obese patients with obstructive sleep apnea [19]. However, further studies are needed to document the lidocaine doses required to prevent remifentanil-induced coughing. Moreover, systematic comparisons of coughing and muscle rigidity for various opioids infusion are also needed. Furthermore, the correlation between body weight and opioid-induced muscle rigidity or coughing that was observed in the present study requires confirmation.
In conclusion, the frequency of remifentanil-induced coughing was 30%. Additionally, lidocaine (0.5 mg/kg) and salbutamol (1 metered aerosol puff) both failed to affect the incidence, onset time, and severity of remifentanil provoked coughing during the induction of anesthesia. Finally, thin and non-smoking patients were found to be at higher risk of remifentanil-induced coughing, which indicates that such patients need more attention during remifentanil infusion.
References
1. Scott LJ, Perry CM. Spotlight on remifentanil for general anaesthesia. CNS Drugs 2005; 19: 1069-1074. PMID: 16332149.


2. Kim JY, Kim JY, Park SY, Jung WS, Kwak HJ. Effect of low dose ketamine to prevent remifentanil-induced cough: a randomized, double-blind, placebo controlled trial. Korean J Anesthesiol 2009; 56: 624-627.


3. Scott LJ, Perry CM. Remifentanil: a review of its use during the induction and maintenance of general anaesthesia. Drugs 2005; 65: 1793-1823. PMID: 16114980.


4. Lin JA, Yeh CC, Lee MS, Wu CT, Lin SL, Wong CS. Prolonged injection time and light smoking decrease the incidence of fentanyl-induced cough. Anesth Analg 2005; 101: 670-674. PMID: 16115973.


5. Tweed WA, Dakin D. Explosive coughing after bolus fentanyl injection. Anesth Analg 2001; 92: 1442-1443. PMID: 11375822.


6. Agarwal A, Azim A, Ambesh S, Bose N, Dhiraj S, Sahu D, et al. Salbutamol, beclomethasone or sodium chromoglycate suppress coughing induced by iv fentanyl. Can J Anaesth 2003; 50: 297-300. PMID: 12620955.


7. Kim JY, Park KS, Kim JS, Park SY, Kim JW. The effect of lidocaine on remifentanil-induced cough. Anaesthesia 2008; 63: 495-498. PMID: 18412647.


8. Pandey CK, Raza M, Ranjan R, Singhal V, Kumar M, Lakra A, et al. Intravenous lidocaine 0.5 mg.kg-1 effectively suppresses fentanyl-induced cough. Can J Anaesth 2005; 52: 172-175. PMID: 15684258.


9. Reitan JA, Stengert KB, Wymore ML, Martucci RW. Central vagal control of fentanyl-induced bradycardia during halothane anesthesia. Anesth Analg 1978; 57: 31-36. PMID: 564641.


10. Lin CS, Sun WZ, Chan WH, Lin CJ, Yeh HM, Mok MS. Intravenous lidocaine and ephedrine, but not propofol, suppress fentanyl-induced cough. Can J Anaesth 2004; 51: 654-659. PMID: 15310631.


11. Oshima T, Kasuya Y, Okumura Y, Murakami T, Dohi S. Identification of independent risk factors for fentanyl-induced cough. Can J Anaesth 2006; 53: 753-758. PMID: 16873340.


12. Poulton TJ, James FM 3rd. Cough suppression by lidocaine. Anesthesiology 1979; 50: 470-472. PMID: 453567.


13. Yukioka H, Hayashi M, Terai T, Fujimori M. Intravenous lidocaine as a suppressant of coughing during tracheal intubation in elderly patients. Anesth Analg 1993; 77: 309-312. PMID: 8346830.


14. Pandey CK, Raza M, Ranjan R, Lakra A, Agarwal A, Singh U, et al. Intravenous lidocaine suppresses fentanyl-induced coughing: a double-blind, prospective, randomized placebo-controlled study. Anesth Analg 2004; 99: 1696-1698. PMID: 15562056.


15. Joshi GP, Warner DS, Twersky RS, Fleisher LA. A comparison of the remifentanil and fentanyl adverse effect profile in a multicenter phase IV study. J Clin Anesth 2002; 14: 494-499. PMID: 12477583.


16. Mulrennan S, Wright C, Thompson R, Goustas P, Morice A. Effect of salbutamol on smoking related cough. Pulm Pharmacol Ther 2004; 17: 127-131. PMID: 15123221.


17. Millqvist E, Bende M. Capsaicin cough sensitivity is decreased in smokers. Respir Med 2001; 95: 19-21. PMID: 11207012.


18. Dicpinigaitis PV. Cough reflex sensitivity in cigarette smokers. Chest 2003; 123: 685-688. PMID: 12628863.


19. Guglielminotti J, Tesniere A, Rackelboom T, Mantz J, Vecchierini MF, Bonay M, et al. Cough reflex sensitivity is decreased in female obese patients with obstructive sleep apnea. Respir Physiol Neurobiol 2007; 158: 83-87. PMID: 17412652.


- TOOLS