Efficacy of the combination of cold propofol and pretreatment with remifentail on propofol injection pain
Article information
Abstract
Background
Pain upon the injection of propofol is a common adverse effect. This study was conducted to evaluate the analgesic effect of remifentanil and cold propofol during propofol injection for the induction of anesthesia and to determine if a combination of cold propofol and remifentanil produced additional analgesic efficacy.
Methods
A total of 160 patients aged 20-65 years old were randomly allocated into one of four groups (n = 40, in each). Control and remifentanil group patients received 2 mg/kg propofol that had been stored at room temperature (20-23℃), while the cold and combination group received cold (4℃) propofol. The patients received remifentanil 0.5 µg/kg IV in the remifentanil and combination groups or saline in the control and cold groups. Ninety seconds after administration the patients were administered propofol over a 30 second period. The pain intensity and incidence were then evaluated using a 4-point verbal rating scale.
Results
The incidence of pain was significantly reduced in groups that received remifentanil in the cold and combination groups when compared with the control group (27.5%, 30%, and 2.5% vs. 70%, respectively). Moreover, the severity of pain was significantly lower in groups that received remifentanil in the cold and combination groups when compared with the control group. The incidence and severity of pain from the propofol injection in the combination group was significantly lower than that in the remifentanil and cold groups.
Conclusions
The combination of cold propofol and pretreatment with remifentanil more effectively reduced the incidence of pain upon the injection of propofol than either treatment alone.
Introduction
Propofol (2,6-diisopropylphenol) is an intravenous hypnotic that has long been a popular choice for induction and maintenance of general anesthesia owing to its rapid onset and short duration. However, pain upon injection with propofol is a common problem that can be very distressing to the patient. The incidence of propofol injection pain has been reported to range from 80% to 90% when the veins on the dorsum of the hand are used for injection without treatment [1,2].
Several investigators have studied pharmacological and nonpharmacological strategies for the prevention of pain upon propofol injection. Specifically, studies have been conducted to evaluate variations in the injection speed and carrier fluids [3], dilutions [4], and concomitant therapies using local anesthetics or opioids [5].
Pretreatment with remifentanil has been reported to reduce the incidence and severity of pain during propofol injection [6-9]. Iyilikci et al. [8] reported that remifentanil effectively prevented propofol injection pain, and that it should be administered at a dose of at least 0.02 mg for this purpose. Moreover, it has been reported that intravenous remifentanil 0.02 mg or remifentanil 0.03 mg pretreatment effectively alleviates the pain associated with propofol injection [9]. However, the failure rate of this treatment was about 40% [8,9], and remifentanil did not completely control propofol-induced pain; thus, combination therapy has been suggested for the prevention of this pain [10]. Moreover, recent studies have revealed that a combination of two different analgesic modalities, opioids and lidocaine, can reduce the incidence and severity of propofol injection pain in adults when compared to administration alone [11,12]. Previous studies have suggested that chilling propofol leads to a decrease in the incidence of propofol injection [13,14]. However, there have been no reports of the use of combination cold propofol and pretreatment with remifentanil to reduce propofol injection pain.
This study was conducted to assess the effectiveness of cold propofol and pretreatment with remifentanil at minimizing the pain associated with the injection of propofol and to determine if a combination of cold propofol and remifentanil produced additional analgesic efficacy.
Materials and Methods
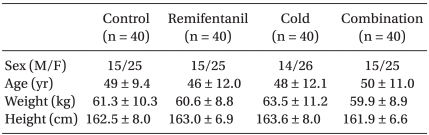
After obtaining approval from the Institutional Review Board and informed consent from the subjects, the study was conducted prospectively on 160 American Society of Anesthesiologists physical status I or II patients aged 20-65 years who underwent general anesthesia for elective surgery. Patients who had known allergies to opioids or propfol; renal, hepatic, or cardiac problems; neurologic deficits or psychiatric disorders: or who had received analgesics or sedatives within the previous 24 hours were excluded. The patients were randomly assigned to one of four groups using an Excel (Microsoft Corp., Seoul, Korea) generated randomization table. The four groups were comparable with respect to patient characteristics (Table 1). No patients were excluded from the analysis due to complications; hence, the data for all 160 patients is presented. The induction dose of propofol (1% Anepol®, Hana Pharm. Co., Ltd., Hwasung, Korea) was 2 mg/kg. For the cold propofol, the propofol was drawn up in 20 ml syringes and maintained at a temperature of 4℃ in a refrigerator until ready for use. The control and remifentanil group patients received propofol 2 mg/kg stored at room temperature (20-23℃) and the cold and combination group received cold (4℃) propofol. The patients received remifentanil 0.5 µg/kg IV in the remifentanil and combination groups, or saline in the control and cold groups over a 30 second period. Ninety seconds later, the patients were given propofol over a 30 second period. Blinding was maintained by the involvement of two practitioners (the drug manipulator and the anesthesia provider) at the induction of every patient. The drug manipulator prepared and injected the drugs, while the anesthesia provider assessed complications and pain and was blinded to the treatment group.
Premedication was not administered prior to the induction of anesthesia. Before arriving at the operating room, a 20 gauge cannula was inserted in the left cephalic vein, and its position was confirmed by the free flow of Hartmann's solution infused by gravity prior to the induction of anesthesia. Upon arrival at the operating room, all patients were evaluated based on electrocardiogram, pulse oximetry, non-invasive arterial pressure, and bispectral index score (BIS) monitoring. All patients were preoxygenated for five minutes prior to the induction of anesthesia. Following remifentanil or saline injection, propofol 2 mg/kg was administered through the rubber port connected to the intravenous cannula without the carrier fluid. The assessment of pain was made continuously from the start of the propofol injection to the point at which the patients lost consciousness. The severity of pain was assessed using a four-point scale. Pain manifested as a verbal response accompanied by facial grimacing or withdrawal of the arm was scored as severe; grimacing or withdrawal not accompanied by a verbal response was scored as moderate pain. If severe or moderate pain was not observed, the patient was asked whether they had any discomfort in the arms. If they answered 'yes', this was scored as mild pain, if they answered 'no', this was scored as no pain [7].
Following the loss of an eyelash reflex, the patients were intubated after administration of rocuronium 0.8 mg/kg. Anesthesia was then conducted at the anesthetist's convenience. After remifentanil or saline injection, the BIS score was checked to subjectively assess the level of consciousness to ensure an adequate response to the pain questionnaires.
The mean arterial pressure and heart rate were recorded prior to injection of the study drug (baseline), after the remifentanil injection, and before tracheal intubation. The chest wall rigidity, which was described as transient chest discomfort, was also recorded during remifentanil injection. Patients were monitored hourly for 24 hours post-surgery by a blinded investigator for adverse effects at the injection site (i.e., pain, edema, wheal, and flare response).
Based on previous studies [10], the incidence of injection pain in the cold or remifentanil group was expected to be ~40%. Therefore, 37 subjects per group would be needed to decrease this incidence to 5% (power 80% and a = 0.05). Additionally, we assumed a dropout rate of 10%; therefore, we increased the sample size to 40 patients per group.
Statistical analyses were conducted using SPSS (version 15.0, SPSS Inc., Chicago, IL, USA). Analyses of variance (ANOVA) was performed on the demographic data using the ANOVA test for continuous variables (i.e., age, height, and weight) and the chi-square test for discrete variables (sex). The Fisher exact test was used to calculate between-group differences in the incidence of propofol-induced pain, and the Kruskal-Wallis rank test was used to assess differences in the mean pain-intensity scores. A P value < 0.05 was considered significant. All values are expressed as the mean (SD) or absolute value (%).
Results
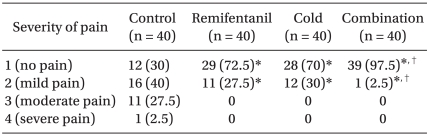
Both the incidence and severity of pain differed significantly among groups (P < 0.01). As shown in Table 2, the incidence and severity of pain was significantly reduced in the remifentanil, cold and combination groups when compared with the control group (P < 0.01).
The incidence of pain from the propofol injection in the combination group (2.5%) was significantly lower than that in the remifentanil and cold groups (27.5% and 30%, respectively, P < 0.01, Table 2). In addition, the severity of pain was significantly lower in the combination group than the remifentanl and cold groups (P < 0.01).
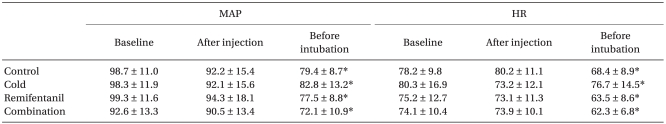
Although the decrease in heart rate (HR) and mean arterial pressure (MAP) prior to intubation was statistically significant in all groups, the decrease in HR and MAP was not of clinical importance (Table 3). Additionally, none of the patients suffered from desaturation, apnea, or chest wall rigidity during the induction of anesthesia.
For all subjects, the BIS score was above 90 prior to propofol injection, indicating adequate responses to questionnaires. There were no adverse effects at the injection site observed in any patients.
Discussion
Our study demonstrated that combined treatment with remifentanil 0.5 µg/kg pretreatment and cold propofol significantly reduced the incidence and severity of propofol injection pain when compared with each treatment alone.
To date, the mechanism by which propofol causes pain upon injection is not fully understood.
In studies examining strategies for the prevention of propofol-induced pain [15], the activation of pain mediators such as the kinin cascade system has been suggested as a possible cause.
Many factors that influence pain during propofol injection have been identified, including temperature [13,14], the size of the vein and speed of injection [15], the site of the IV cannula [16], dilution [4] and sedative medication [17].
It has also been reported that the incidence and severity of pain during propofol injection were related to the formulation of propofol [18,19]. Larsen et al. [18] has reported that a new formulation of propofol (a 10% fat emulsion formulated with long- and medium-chain triglycerides) may be associated with less pain upon injection. Microemulsion of propofol produces more frequent and severe pain upon injection than lipid emulsion propofol, which may be attributable to higher concentrations of aqueous free propofol [19].
Remifentanil is a synthetic and esterase-metabolized opioid with a rapid onset, an ultrashort duration of action, and a short context-sensitive half-time when compared with other opioids [20]. Several investigators have reported that remifentanil administered via bolus injection or continuous infusion effectively reduces propofol injection pain with varying results [6-9]. It has also been reported that intravenous remifentanil 0.02 mg or remifentanil 0.03 mg pretreatment is effective at alleviating the pain associated with a propofol injection to 40% and 30% of that reported without pretreatment [9]. In the present study, pretreatment with remifentanil 0.5 µg/kg significantly reduced the incidence of propofol injection pain from 70% to 27.5%, which is comparable with of the results observed in other studies [8,9].
We assumed that the pain-reducing action of remifentanil was primarily central because a tourniquet technique was not used and adequate time was allowed for the onset of remifentanil (90 s). Moreover, it has been reported that intravenous opioids administered as Bier's block prior to propofol injection failed to show analgesic efficacy [21,22].
Changing the temperature of administered propofol has produced conflicting results in adults. Two studies demonstrated reduced pain in response to treatment with cold propofol [13,14], and it has been suggested that this mechanism may occur due to the decreased speed of the kinin cascade and the stabilization of local pain mediators at lower temperatures [13]. Conversely, two studies have failed to demonstrate a reduction in pain using cold propofol [23,24]. However, we found that administration of propofol at 4℃ reduced the incidence of injection pain from 70% to 30%, which is comparable to the results obtained in response to pretreatment with remifentanil at 0.5 µg/kg.
In this study, the incidence of injection pain of propofol was reduced to 2.5% of patients in the combination group. Conversely, 27.5% of patients in the remifentanil group and 30% of patients in the cold group suffered from painful injection. The mechanism involved in this synergistic interaction has not been identified; therefore, further study to elucidate this mechanism is warranted.
Although the decrease in HR and MAP prior to intubation was statistically significant in all groups, the decrease of HR and MAP was not of clinical importance. None of the patients suffered from desaturation, apnea or chest wall rigidity during the induction of anesthesia. For all subjects, the BIS score was greater than 90, indicating adequate responses to questionnaires. No adverse effects at the injection site were observed in any patient.
It is important to consider the findings presented here within the context of the limitation of the study. Specifically, we did not use higher doses of remifentanil for our study. Higher doses of remifentanil may have produced further reductions in propofol injection pain, which would be of clinical benefit if it is not associated with an increase in the incidence of complications. Seconds, Hanci et al. [25] reported that the phases of the menstrual cycle may have a significant role on injection pain of propofol in women. However, the comparison for pain incidence and intensity with menstrual cycle was not evaluated. Further studies should consider these limitations.
In conclusion, the combination of cold propofol and pretreatment with remifentanil more effectively reduced the incidence and severity of pain upon injection of propofol than either treatment alone.