 |
 |
|
|
Abstract
Background
Monitoring of anesthetic depth is important for successful general anesthesia. It is well known that entropy or BIS monitoring assisted titration of anesthetic drugs decreases their consumption. This study evaluated the effect of remifentanil on consumption of sevoflurane during entropy monitored general anesthesia.
Methods
Patients were randomly assigned to two groups. The R group was administered 0.1 ┬Ąg/kg/min of remifentanil and inhaled sevoflurane, while the S group was administered only inhaled sevoflurane. Anesthesia was maintained using sevoflurane with nitrous oxide, and entropy was monitored. In both groups, the concentration of sevoflurane was adjusted to keep the state entropy (SE) value between 40 and 60. End-tidal sevoflurane concentration (ET), entropy value, systolic blood pressure (SBP), diastolic blood pressure (DBP) and heart rate (HR) were measured at 5 minute intervals, during a 25 minute period after intubation, skin suture and the end of surgery.
Anesthetic awareness can cause perioperative pain and discomfort, as well as temporary after-effects, such as postoperative anxiety, sleep disorder, nightmares, and recall. In some cases, it can cause post-traumatic stress disorder. Therefore, the anesthesiologist has to carefully maintain anesthetic depth.
Anesthetic depth is judged from observing vital signs and can be adjusted by the dose of administered anesthetics, depending on the patient's vital signs. Monitoring anesthetic depth makes it possible to administer the appropriate dose of anesthetics and prevent anesthetic awareness, side-effects of over-dose, and economic and environmental waste. Therefore, anesthetic management, using proper anesthetic administration, is equally important as maintaining the patient's vital signs.
Entropy monitoring allows for the quantification of cerebral neural activity. The increase and decrease in entropy scores are related to the level of consciousness under anesthesia. EEG-entropy is an entropy monitor based on EEG analysis used in measuring hypnosis levels [1]. EEG-entropy has two signals: State entropy (SE) receives information from the brain waves; response entropy (RE) incorporates information from the frontal eletromyography. SE is computed using EEG data from the previous 15 s, between 0.8-32 Hz, and shows the value in the range of 0-91. RE is computed from 32-47 Hz with 1.92 s, and reflects fast muscular activity from the frontal muscle, and shows the value in the range of 0-100. Similar to BIS, 100 signifies awake; 60, clinically significant anesthetic state; 40, low possibility of consciousness; and 0, suppression of cortical activity [2].
The authors maintained the appropriate anesthetic depth for patients undergoing entropy-monitored gynecological surgery and controlled anesthetic depth by titrating the concentration of the inhaled anesthetic - sevoflurane. In this study, the authors attempted to compare the ET sevoflurane concentration (ET) when using continuous infusion of sevoflurane alone, against ET when using remifentanil as a supplement to sevoflurane, to determine the difference in administered doses of sevoflurane.
Upon receiving the approval of the hospital ethics committee and the consent of the patients after they were informed about the study during preanesthetic visitation, we performed the study on 40 patients of ASA class I & II, electing for gynecological surgery under general anesthesia.
Patients were excluded if they had a neurologic or psychiatric disease, past history of cardiovascular disease, or if they had consumed sedatives, antidepressants, anticonvulsants, or opioids. Also, patients were excluded if intubation was expected to be difficult or had been difficult in the past.
The patients were randomly divided into two groups that were infused with remifentanil (Group R) or normal saline (Group S). Normal saline (40 ml) and remifentanil (40 ml) diluted with normal saline (50 ┬Ąg/ml) were prepared in continuous infusors. The anesthesiologist was blinded for the study and no patient was given premedication. Upon arrival onto the operating table, electrocardiography, non-invasive blood pressure, and pulse oxymetry were attached for monitoring. The entropy sensor was attached to the patient's forehead (Entropy Sensor, Disposable, GE Healthcare, Helsinki, Finland), connecting the patient to the entropy monitor (S/5 Entropy Module, Datex-Ohmeda, Madison, WI, USA).
Anesthesia was induced using thiopental sodium (5 mg/kg) in both groups. After loss of consciousness, rocuronium (1.0 mg/kg) was administered, and manual mask ventilation was performed using 4 vol% sevoflurane. After sufficient muscle relaxation, before intubation, IV remifentanil (1.0 ┬Ąg/kg) was slowly administered for 1 min in both groups. Following intubation, O2-N2O-sevoflurane was used for the maintenance of anesthesia. In the two groups, either the prepared normal saline or remifentanil was administered with the continuous infusor at the rate of 0.002 ml/kg/min, 2 vol% sevoflurane was inhaled, and the SE value was maintained between 40-60 by titrating 0.5 vol% sevoflurane every 5 minutes. Despite controlling the concentration of sevoflurane to maintain SE value, when the hemodynamics could not be stabilized, cardiovascular drugs were used and recorded afterwards. The surgery proceeded, and when skin suturing (SS) was started, the continuous infusion of either saline solution or remifentanil and the administration of sevoflurane were stopped and the patient was ventilated with 100% O2. After the surgery, muscle relaxation was reversed.
The systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), RE, SE, and end-tidal sevoflurane concentration (ET) measurements were recorded by a blinded medical resident immediately after intubation, at 5 min intervals over a 25 min period, at the beginning of SS and at the end of surgery. The measurements of the two groups were compared. The mean ET scores taken every 5 min immediately after intubation until the end of surgery were averaged and analyzed for the purpose of comparing sevoflurane.
All statistical analyses were performed on SPSS (version 18.0, SPSS Inc., IL, USA). The values were expressed as mean ┬▒ SD. To test homogeneity, age height, weight and the administration time of sevoflurane were analyzed using an independent t-test and ASA classes using a chi-square test. The comparison of the mean ET measured from post-intubation until the end of the surgery for the two groups was analyzed using an independent t-test. ET, RE, SE, SBP, DBP, and HR values were analyzed using a repeated measure one-way ANOVA. When time affected a line, a contrast test was performed on the values taken 5 min post-intubation to the end of surgery. The analysis of each period was done using an independent t-test; P < 0.05 was considered statistically significant.
The demographic data analysis showed no statistical differences in the patient age, weight, or height (Table 1). The two groups showed significant differences in ET (Fig. 1) (P < 0.05). During time periods from 5 min post-intubation to the end of surgery, ET values were significantly lower in Group R compared to Group S (Fig. 1) (P < 0.05). Perioperative mean ET in Group S (1.63 ┬▒ 0.15) was significantly lower than in Group R (1.11 ┬▒ 0.10) (P < 0.05).
RE and SE were maintained in both groups between 40-60, and there were no significant differences amongs subjects in both groups (Fig. 2 and 3) (P > 0.05).
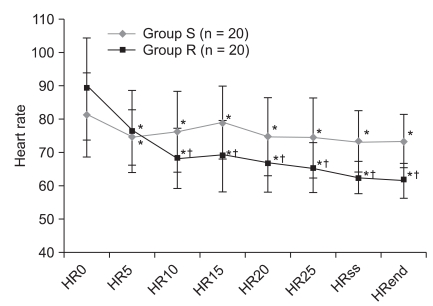
The SBP and DBP were not significantly different and they were similar with the progress of time (P > 0.05). Comparing intervals, Group R compared to Group S had low SBP and DBP 10 min and 15 min post-intubation, but there were no differences afterwards (Fig. 4 and 5). HR values were significantly different (P < 0.05). Although Group R, compared to Group S, had lower HR values from 10 min post-intubation (Fig. 6) (P < 0.05), this was clinically insignificant. Neither group required drug administration for intra-operative hemodynamic stabilization.
In general anesthesia, correctly judging and maintaining anesthetic depth is very important. Judging the depth of anesthesia from observing patient cardiovascular response and then titrating the dose of anesthetics is common, but with the introduction of EEG-entropy, one can monitor the depth of anesthesia and the hypnosis level, and it measures anesthetic depth similar to BIS in anesthesia using propofol or sevoflurane [1-4].
Vakkuri et al. [2] stated that in sevoflurane-anesthesia, the appropriate depth of anesthesia has the entropy value of 40-60. In the current study, sevoflurane concentration was adjusted so the entropy value could be maintained between 40-60. Comparisons of RE and SE between the two groups showed no significant differences, and they followed similar changes with time.
Remifentanil is an opioid, with a rapid onset of effect and a short duration that selectively affects the ┬Ą-receptor [5]. Because of its pharmacokinetic characteristics, it is commonly used as a supplement in general anesthesia performed with inhaled or intravenous anesthetics [6]. However, it has side-effects such as hypotension, postoperative nausea and vomiting (PONV), respiratory depression, and increased postoperative pain. O'Hare et al. [7] stated that a bolus infusion of remifentanil (1 ┬Ąg/kg) can control the balance of hemodynamic response at the time of intubation and reduce the risk of post-intubation hypotension. Lee et al. [8] stated that a bolus infusion of remifentanil (1.0 or 2.0 ┬Ąg/kg) effectively suppresses the increase in post-intubation mean arterial blood pressure (MAP) and HR. A remifentanil dose of 2.0 ┬Ąg/kg can permit hypotension to persist, so 1.0 ┬Ąg/kg is considered the more appropriate dose. Song and White [9] stated that in desflurane-anesthesia, a low supplementary dose of remifentanil (0.07 ┬Ąg/kg/min) can effectively control the autonomic nervous system response to nociceptive stimulation during laparoscopic surgery, and allows for fast awakening without postoperative side-effects. Song et al. [10] compared the usage to the non-usage of remifentanil (0.05-0.2 ┬Ąg/kg/min) in patients under sevoflurane-anesthesia for a laparoscopic cholecystectomy and found that the patient awakening and extubation times were shorter without raising PONV rates and without the extra use of antiemetics or analgesics.
Lee et al. [11] also similarly found that patients undergoing laparoscopic cholecystectomy, who were anesthetized with sevoflurane with the continuous infusion of remifentanil (0.1 ┬Ąg/kg/min), did not have higher rates of PONV, pain, or a greater use of analgesics. Calder├│n et al. [12] found that when either remifentanil (0.05 ┬Ąg/kg/min or 0.1 ┬Ąg/kg/min) was continuously infused in patients undergoing elective abdominal and thoracic surgery, postoperative pain was effectively managed in both groups, without side-effects such as respiratory depression or PONV. Also, the group continuously infused with remifentanil (0.1 ┬Ąg/kg/min) required less additional analgesics. Therefore, the current study sought to stabilize hemodynamic response to intubation while reducing the risk of post-intubation hypotension by slowly infusing IV remifentanil (1.0 ┬Ąg/kg) for 1 min. To effectively control post-intubation perioperative autonomic nervous system response and to allow for faster awakening without side-effects, a low dose of remifentanil (0.1 ┬Ąg/kg/min) was continuously infused. The vital signs were then measured, and showed that they were lower for Group R than Group S. Neither group required drugs to safely maintain hemodynamics.
G├│mez de Segura et al. [13] found through a rat experiment, that the continuous infusion of remifentanil in rats under sevoflurane-anesthesia decreased sevoflurane MAC proportionally to the dose of remifentanil. Manyam et al. [14] found that remifentanil decreased the required dose of sevoflurane when they performed anesthesia using TCI of sevoflurane (0.3-6 vol%) and the effect-site concentration of remifentanil was 0.5-15 ng/ml. Pavlin et al. [15] used a BIS monitor to titrate the dose of sevoflurane and found that ET was reduced by 13%. Aim├® et al. [16] found that in sevoflurane-anesthesia using either BIS or an entropy monitor to titrate the administered dose of anesthetics, both monitoring methods equally reduced the administered dose of sevoflurane by 29%.
Therefore, the current study used an entropy monitored titration of sevoflurane and the continuous infusion of remifentanil to determine if the administered dose of sevoflurane could be reduced, and the results were significantly different. Compared to Group S, Group R had significantly lower ET, and significantly lower mean ET when measured during surgery. When sevoflurane alone is used in anesthesia, compared to when remifentanil is used as a supplement, it is believed that a greater dose of sevoflurane is unnecessary.
Many factors affect the patient's recovery from anesthesia, and the level of the residual anesthetic can be a factor. Also, if an individual's methabolism rate of the drug is consistent, the determinant factor is the administered dose of the anesthetic. Recart et al. [17] studied 90 patients to determine the effect of desflurane dose on the recovery time. Patients who were administered low doses of desflurane, from titrating to the auditory evoked potential or BIS monitor, had shorter extubation times and shorter lengths of PACU stay. Thus, the dose of anesthetics was found to directly affect recovery rates. Also, many studies have found that compared to the single use of sevoflurane, the combined use of remifentanil and sevoflurane reduces the required dose of sevoflurane and allows for faster patient recovery [18,19]. Although the current study did not measure the extubation or recovery times, the authors found that the continuous infusion of remifentanil proved to reduce the necessary dose of sevoflurane, and may also help in the recovery from anesthesia.
The current study monitored the depth of anesthesia when sevoflurane alone and when sevoflurane plus a low dose of remifentanil (0.1 ┬Ąg/kg/min) were administered; and the authors found that with the combined use of remifentanil, low doses of sevoflurane can also maintain anesthetic depth. The intra-operative mean ET was reduced approximately 32%. In the combined use of sevoflurane and remifentanil, the authors kept the dose concentration consistently at 0.1 ┬Ąg/kg/min, but titrating remifentanil's concentration to hemodynamic changes may also be helpful.
In conclusion, in entropy monitoring of anesthetic depth, administering a low dose of remifentanil (0.1 ┬Ąg/kg/min) as a supplement to inhaled anesthetics, will allow for a decreased dose of inhaled anesthetics, compared to when inhaled anesthetics are used alone. This will prevent the delay in recovery resulting from overdose and circumvent economic and environmental waste. Even without the entropy-monitoring of anesthetic depth, the combined use of sevoflurane and remifentanil can reduce the inhaled dose of sevoflurane, without perioperative awareness.
References
1. Bruhn J, Bouillon TW, Radulescu L, Hoeft A, Bertaccini E, Shafer SL. Correlation of approximate entropy, bispectral index, and spectral edge frequency 95 (SEF95) with clinical signs of "anesthetic depth" during coadministration of propofol and remifentanil. Anesthesiology 2003; 98: 621-627. PMID: 12606904.


2. Vakkuri A, Yli-Hankala A, Talja P, Mustola S, Tolvanen-Laakso H, Sampson T, et al. Time-frequency balanced spectral entropy as a measure of anesthetic drug effect in central nervous system during sevoflurane, propofol, and thiopental anesthesia. Acta Anaesthesiol Scand 2004; 48: 145-153. PMID: 14995935.


3. Schmidt GN, Bischoff P, Standl T, Hellstern A, Teuber O, Schulte Esch J. Comparative evaluation of the Datex-Ohmeda S/5 Entropy Module and the Bispectral Index monitor during propofol-remifentanil anesthesia. Anesthesiology 2004; 101: 1283-1290. PMID: 15564934.


4. Vanluchene AL, Vereecke H, Thas O, Mortier EP, Shafer SL, Struys MM. Spectral entropy as an electroencephalographic measure of anesthetic drug effect: a comparison with bispectral index and processed midlatency auditory evoked response. Anesthesiology 2004; 101: 34-42. PMID: 15220769.


5. Glass PS, Hardman D, Kamiyama Y, Quill TJ, Marton G, Donn KH, et al. Preliminary pharmacokinetics and pharmacodynamics of an ultra-short-acting opioid: remifentanil (GI87084B). Anesth Analg 1993; 77: 1031-1040. PMID: 8105723.


6. Beers R, Camporesi E. Remifentanil update: clinical science and utility. CNS Drugs 2004; 18: 1085-1104. PMID: 15581380.



7. O'Hare R, McAtamney D, Mirakhur RK, Hughes D, Carabine U. Bolus dose remifentanil for control of haemodynamic response to tracheal intubation during rapid sequence induction of anaesthesia. Br J Anaesth 1999; 82: 283-285. PMID: 10365011.



8. Lee JR, Jung CW, Lee JH, Choi IY, Seo KS, Kim HK, et al. Optimal dose of remifentanil to suppress cardiovascular response to laryngoscopic endotracheal intubation. Korean J Anesthesiol 2005; 49: 780-785.

9. Song D, White PF. Remifentanil as an adjuvant during desflurane anesthesia facilitates early recovery after ambulatory surgery. J Clin Anesth 1999; 11: 364-367. PMID: 10526805.


10. Song D, Whitten CW, White PF. Remifentanil infusion facilitates early recovery for obese outpatients undergoing laparoscopic cholecystectomy. Anesth Analg 2000; 90: 1111-1113. PMID: 10781462.


11. Lee JJ, Hong SJ, Kim JS, Hwang SM, Lim SY, Lee SK. The effect of intraoperative remifentanil infusion on analgesic requirements after laparoscopic cholecystectomy. Korean J Anesthesiol 2009; 57: 161-164.


12. Calder├│n E, Pernia A, De Antonio P, Calder├│n-Pla E, Torres LM. A comparison of two constant-dose continuous infusions of remifentanil for severe postoperative pain. Anesth Analg 2001; 92: 715-719. PMID: 11226107.


13. G├│mez de Segura IA, de la Vibora JB, Aguado D. Opioid tolerance blunts the reduction in the sevoflurane minimum alveolar concentration produced by remifentanil in the rat. Anesthesiology 2009; 110: 1133-1138. PMID: 19352151.


14. Manyam SC, Gupta DK, Johnson KB, White JL, Pace NL, Westenskow DR, et al. Opioid-volatile anesthetic synergy: a response surface model with remifentanil and sevoflurane as prototypes. Anesthesiology 2006; 105: 267-278. PMID: 16871060.


15. Pavlin DJ, Hong JY, Freund PR, Koerschgen ME, Bower JO, Bowdle TA. The effect of bispectral index monitoring on endtidal gas concentration and recovery duration after outpatient anesthesia. Anesth Analg 2001; 93: 613-619. PMID: 11524328.


16. Aim├® I, Verroust N, Masson-Lefoll C, Taylor G, Lalo├½ PA, Liu N, et al. Does monitoring bispectral index or spectral entropy reduce sevoflurane use? Anesth Analg 2006; 103: 1469-1477. PMID: 17122226.


17. Recart A, Gasanova I, White PF, Thomas T, Ogunnaike B, Hamza M, et al. The effect of cerebral monitoring on recovery after general anesthesia: a comparison of the auditory evoked potential and bispectral index devices with standard clinical practice. Anesth Analg 2003; 97: 1667-1674. PMID: 14633540.


18. van Delden PG, Houweling PL, Bencini AF, Ephraim EP, Frietman RC, van Niekerk J, et al. Remifentanil-sevoflurane anesthesia for laparoscopic cholecystectomy: comparison of three dose regimens. Anaesthesia 2002; 57: 212-217. PMID: 11879208.


19. Breslin DS, Reid JE, Mirakhur RK, Hayes AH, McBrien ME. Sevoflurane-nitrous oxide anaesthesia supplemented with remifentanil: effect on recovery and cognitive function. Anaesthesia 2001; 56: 114-119. PMID: 11167470.


Fig.┬Ā1
Change of end-tidal sevoflurane concentration. Values are expressed as mean ┬▒ SD. Group S: group received normal saline. Group R: group received remifentanil (0.1 ┬Ąg/kg/min). ET0-25: end-tidal sevoflurane concentration at 0-25 minute after intubation, ETss: end-tidal sevoflurane concentration at skin suture, ETend: end-tidal sevoflurane concentration at end of surgery. *P < 0.05 compared with ET0. ŌĆĀP < 0.05 compared with Group S.
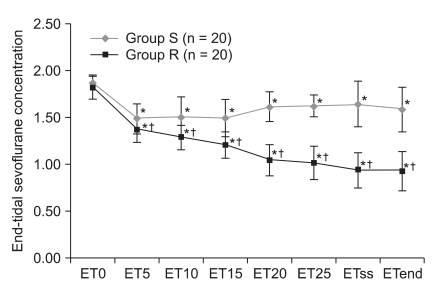
Fig.┬Ā2
Change of response entropy. Values are expressed as mean ┬▒ SD. Group S: group received normal saline. Group R: group received remifentanil (0.1 ┬Ąg/kg/min). RE0-25: response entropy at 0-25 minute after intubation, REss: response entropy at skin suture, REend: response entropy at end of surgery.
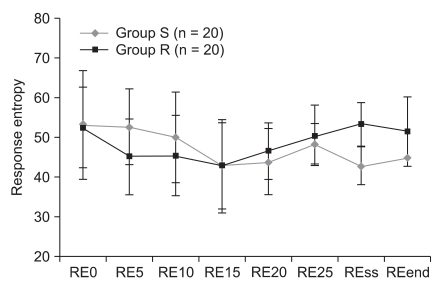
Fig.┬Ā3
Change of state entropy. Values are expressed as mean ┬▒ SD. Group S: group received normal saline. Group R: group received remifentanil (0.1 ┬Ąg/kg/min). SE0-25: state entropy at 0-25 minute after intubation, SEss: state entropy at skin suture, SEend: state entropy at end of surgery.
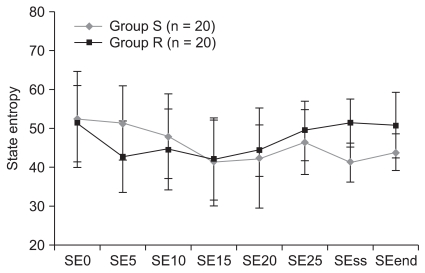
Fig.┬Ā4
Change of systolic blood pressure. Values are expressed as mean ┬▒ SD. Group S: group received normal saline. Group R: group received remifentanil (0.1 ┬Ąg/kg/min). SBP0-25: systolic blood pressure at 0-25 minute after intubation, SBPss: systolic blood pressure at skin suture, SBPend: systolic blood pressure at end of surgery. *P < 0.05 compared with SBP0. ŌĆĀP < 0.05 compared with Group S.
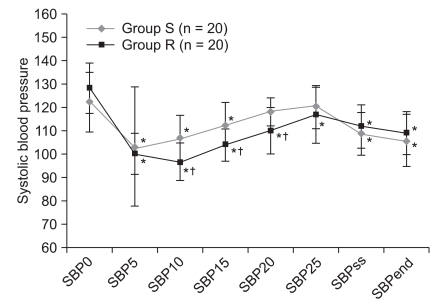
Fig.┬Ā5
Change of diastolic blood pressure. Values are expressed as mean ┬▒ SD. Group S: group received normal saline. Group R: group received remifentanil (0.1 ┬Ąg/kg/min). DBP0-25: diastolic blood pressure at 0-25 minute after intubation, DBPss: diastolic blood pressure at skin suture, DBPend: diastolic blood pressure at end of surgery. *P < 0.05 compared with DBP0. ŌĆĀP < 0.05 compared with Group S.
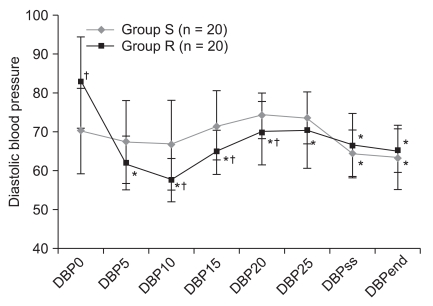
Fig.┬Ā6
Change of heart rate. Values are expressed as mean ┬▒ SD. Group S: group received normal saline. Group R: group received remifentanil (0.1 ┬Ąg/kg/min). HR0-25: heart rate at 0-25 minute after intubation, HRss: heart rate at skin suture, HRend: heart rate at end of surgery. *P < 0.05 compared with HR0. ŌĆĀP < 0.05 compared with Group S.
- TOOLS









