Effect of arterial oxygen tension during reperfusion on myocardial recovery in patients undergoing valvular heart surgery
Article information
Abstract
Background
Valvular heart surgery (VHS) utilizing cardiopulmonary bypass (CPB) is inevitably associated with ischemic-reperfusion injury, which is known to depend on oxygen tension during reperfusion. The aim of this study was to evaluate the effect of arterial oxygen tension during reperfusion on myocardial recovery in patients undergoing VHS.
Methods
Fifty-six patients undergoing isolated VHS were randomly exposed to an oxygen fraction of 0.7 (hyperoxic group, n = 28) or 0.5 (normoxic group, n = 28) during reperfusion. All patients received an oxygen fraction of 0.7 during CPB. In the normoxic group, the oxygen fraction was lowered to 0.5 from the last warm cardioplegia administration to 1 minute after aortic unclamping, and was then raised back to 0.7. Hemodynamic data were measured after induction of anesthesia, weaning from CPB, and sternum closure. The frequency of cardiotonic medications used during and after weaning from CPB, and the short-term outcomes during the hospital stay were also assessed.
Results
The frequency of vasopressin and milrinone use during weaning from CPB, but not norepinephrine, was significantly less in the normoxic group. The post-operative cardiac enzyme levels and short-term outcomes were not different between the groups.
Conclusions
Normoxic reperfusion from the last cardioplegia administration to 1 minute after aortic unclamping in patients undergoing VHS resulted in significantly less frequent use of vasopressin and inotropics during weaning from CPB than hyperoxic reperfusion, although it did not affect the post-operative myocardial enzyme release or short-term prognosis.
Introduction
During surgery utilizing cardiopulmonary bypass (CPB), the heart is damaged not only by ischemic injury during aortic cross clamping (ACC), but also reperfusion injury after discontinuation of ACC. Especially, valvular heart surgery (VHS) requires a longer CPB duration than coronary artery bypass graft (CABG) surgery and has the possibility of reducing myocardial function by increased afterload post-operatively [1]. Thus, reducing reperfusion injury is very important in improving prognosis.
The overproduction of reactive oxygen-derived free radicals during reperfusion after ischemic injury is a major cause of the ischemic-reperfusion myocardial injury [2]. The rate of production of reactive oxygen-derived free radicals depends on the oxygen tension at reperfusion [3,4]. Previous studies have demonstrated that reducing the oxygen concentration in the CPB circuit to normoxic levels reduces the production of creatine kinase (CK)-MB in patients undergoing CABG [5]. However, monitoring devices enabling the continuous evaluation of arterial oxygen tension are not available in South Korea, and lowering oxygen tension during CPB without an appropriate real-time monitoring device for hypoxemia is unsafe. Therefore, it is difficult to maintain lower oxygen tension throughout CPB. In contrast, by lowering the oxygen fraction to 0.5 from the last warm cardioplegia administration to 1 minute after aortic unclamping, one can access hypoxic events through serial arterial blood analysis during the reperfusion period. This period is usually short, and the risk of hypoxia is low. By lowering the oxygen fraction of the reperfusate, the reactive oxygen-derived free radicals, which are the main cause of reperfusion myocardial injury that occurs with reoxygenation, can be reduced thus facilitatingmyocardial recovery during weaning from CPB and after surgery.
The aim of this study was to evaluate the effect of arterial oxygen tension during reperfusion on myocardial recovery in patients undergoing VHS by an analysis of hemodynamic variables, frequency of cardiotonic drug use, and short-term outcomes.
Materials and Methods
The study group was comprised of 56 consecutive patients undergoing valve replacement surgery due to valvular heart disease. The age range was from 18-75 years. The study was approved by the institutional review board and all patients gave informed consent before inclusion in the study. The pre-operative evaluation included the past medical history, cardiac echogram, common blood cell count, and routine chemistries. The exclusion criteria included a left ventricular ejection fraction <30%, emergency surgery, anemia, evidence of a coagulopathy, chronic lung disease, liver and kidney disease, a history of heart surgery, and taking medications, such as heparin, coumadin, aspirin, and anti-platelet medications, within 5 days. Patients who restarted CPB after failure of the first valve replacement surgery, used mechanical support during weaning of CPB, and had an oxygen partial pressure <75 mmHg with an inspired oxygen fraction of 0.4 after induction were also excluded.
Patients were randomly allocated to 2 groups based on the FiO2 at the time of last reperfusion after aortic unclamping during CPB, as follows: group FiO2 0.7 (hyperoxic group, n = 28); and group FiO2 0.5 (normoxic reperfusion, n = 28). Only the perfusionist who controlled the FiO2 during CPB was aware of the patient group. The anesthetists and surgeons obtained information about the patient groups after surgery.
Lowering the oxygen fraction to 0.7 during CPB was determined by previous surgical experience in our hospital involving safe and lower oxygen fraction without continuous monitoring of the CPB circuit. In the current study, the oxygen partial pressure of arterial blood was 250-350 mmHg in the hyperoxic group. The oxygen fraction of 0.7 was the minimal oxygen fraction to maintain an oxygen partial pressure >200 mmHg. We obtained oxygen partial pressures between 300 and 350 mmHg in the hyperoxic group, which were lower than a previous study [5]. And the oxygen fraction of 0.5 in the normoxic group was determined from preliminary studies that obtained oxygen partial pressure 150 mmHg in the normoxic group [5].
All patients continued cardiac medications, except diuretics, and received an intramuscular injection of morphine (0.05 mg/kg) for pre-medication 1 hour before arrival to the operating room. Upon arrival in the operating room, standard monitoring devices were applied and a radial artery catheter was inserted under local anaesthesia for continuous blood pressure monitoring. Pulmonary artery catheter (Swan-Ganz CCOmbo®CCO/SvO2, Edwards Lifesciences LLC, USA) was inserted via the right internal jugular vein under local anesthesia for continuous measurement of the cardiac index (CI), mixed venous oxygen saturation (SvO2), right ventricular ejection fraction (RVEF), and right ventricular end-diastolic volume index (RVEDVI). Cerebral oxymetry sensors (INVOS 5100TM, Somanetics, Troy, MI, USA) were applied to the forehead of the patients for continuous monitoring of regional cerebral oxygen saturation (rSO2).
Anesthesia was induced with midazolam (2.5 mg), sufentanil (1.5-3.0 µg/kg), and rocuronium bromide (50 mg). After tracheal intubation, the lungs were ventilated with a tidal volume of 8-10 ml/kg at a rate of 8-12 breaths/min, a FiO2 of 0.4, and a peak expiratory positive pressure (PEEP) of 5 mmH2O. Anesthesia was maintained with a continuous infusion of sufentanil (0.5-1.5 µg/kg/h), vecuronium (1-2 µg/kg/min), and sevoflurane (1-2%).
Heparin was given at a dose of 3 mg/kg before CPB and additional heparin was administered to maintain the ACT >480 s during CPB. Tranexamic acid (2 g) was loaded before CPB; 1 g was mixed to a pump priming solution and infused continuously (6 mg/kg/h) until the end of surgery. All the patients began CPB with moderate systemic hypothermia, and used blood cardioplegia. The bypass circuit had a membrane-type oxygenator, and the blood flow rate was 2.2-2.4 L/min/m2. Acid-base balance was corrected with α-stat. Norepinephrine or sodium nitroprusside was infused to maintain the mean arterial blood pressure between 60 and 80 mmHg, and vasopressin (1 unit) was administered when using norepinephrine >0.5 µg/kg/min. Packed red blood cells were transfused when the Hct was <20% during CPB. Sufentanil (1.5 µg/kg) and midazolam (0.05 mg/kg) were administered before the re-warming period.
All patients received an oxygen fraction of 0.7 during CPB. In the normoxic group, the oxygen fraction was lowered to 0.5 from the last warm cardioplegia administration to 1 minute after aortic unclamping, and then raised back to 0.7. In both the hyperoxic and normoxic groups, arterial blood gas analysis from an arterial cannula was done and the rSO2 was recorded after the last warm cardioplegia administration. Blood cardioplegia was a mixture of crystalloid cardioplegia and the patienttalloid cin a 4 : 1 ratio. With an oxygen fraction of 0.7, the PaO2 of blood cardioplegia was 272 ± 72 blood cardithe PaO2 of arterial blood was 293 ± 93 arter (P = 0.57). With an oxygen fraction of 0.5, the PaO2 of blood cardioplegia and arterial blood was 97 ± 48 mmHg and 83 ± 444 mmHg, respectively (P = 0.687). There were no specific differences between the PaO2 of blood cardioplegia and arterial blood. Because the partial pressure of oxygen of crystalloid cardioplegia was about 160-180 mmHg, it had no specific effect on the oxygen partial pressure of the mixture of cardioplegia and the patientod cardioplegia and arterial blood. Because the parti2 of the arterial blood from the arterial cannula because there were no differences in the PaO2 between the blood cardioplegia and arterial blood, and blood cardioplegia was administered in a brief period.
Heparin was reversed with protamine (0.5 mg per 100 units of the initial heparin dose) after CPB. An autotransfusion system (Cell Saver® 5 system; Haemonetics, MA, USA) was used and the remaining blood in the CPB pump was reinfused to the patient after processing by the Cell Saver® 5 system. Norepinephrine was infused when the mean systemic arterial pressure (MAP) was decreased to <60 mmHg during and after weaning of CPB and vasopressin was infused continuously (2-4 unit/h) to the patients using norepinephrine over 0.3 µg/kg/min who took a renin-angiotensin system inhibitor before surgery. Nicardipine was infused when the mean systemic arterial pressure (MAP) was increased to >90 mm Hg. Milrinone was infused (0.5 µg/kg/min) after a 50 µg administration to patients who had a CI <2.0 L/min/m2, PCWP >18 mmHg, and LVEF <40% at trans-esophageal echocardiogram.
All patients were transferred to the ICU after surgery. Packed red blood cells were transfused when the Hct was <25%. Fresh frozen plasma was transfused to correct microvascular bleeding (bleeding >200 ml/h for 2 consecutive hours) or in the presence of abnormal coagulation values (PT[INR] > 1.5). The platelet concentrate was transfused when the platelet count was <50,000 mm3.
Hemodynamic variables, including heart rate (HR), mean arterial pressure (MAP), central venous pressure (CVP), mean pulmonary artery pressure (MPAP), and CO were recorded during induction of anesthesia, weaning from CPB, and sternum closure. The amount and frequency of cardiotonic medications used during CPB and weaning from CPB was recorded. The hemodynamic variables were recorded 6 and 24 hours after surgery in the the ICU, and cardiac enzymes were measured 12 and 24 hours after surgery. The complications during admission were recorded. The respiratory support period and length of the stay in the ICU and general ward was also recorded.
The sample size calculation was performed based on the data of patients undergoing VHS in our hospital. The standard deviation (SD) of cardiac output was 0.7, assuming 1 SD has clinical significance between groups. This generated an estimate of 22 patients in each group with a 90% power to detect 1 SD in cardiac output (0.7 L/min/m2) and an alpha level of 0.05. Considering a 20% estimated dropout, we included 28 patients in each group. Statistical analyses were performed using SPSS 13.0 (SPSS Inc., Chicago, IL, USA). Data were assessed for normal distribution of variance with a Shapiro-Wilk test and Q-Q plot. All data are expressed as the number of patients or mean ± SD. Discrete variables between the groups were compared using Chi-square test, Fisher's exact test, and continuous variables were compared using Mann-Whitney U test. Continuous variables between the groups, such as hemodynamic data were compared using repeated-measures ANOVA. Changes at time points between the groups were compared using a Bonferroni correction after the t-test. Comparing contra data (data after anesthesia induction) within the groups was done using Dunnett's test. A P value < 0.05 was considered statistically significant.
Results
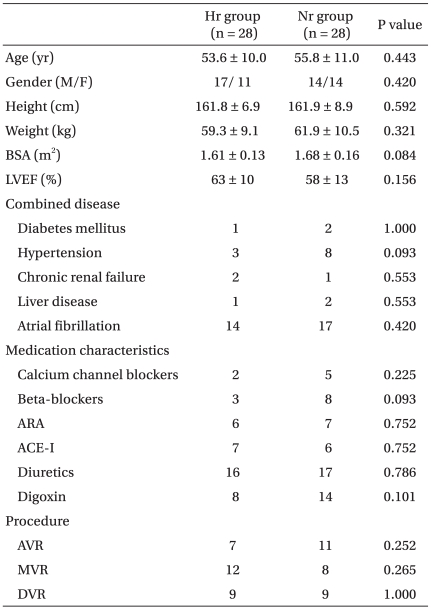
There were no significant differences in the demographic data, pre-operative medications, and types of surgery between the two groups (Table 1).
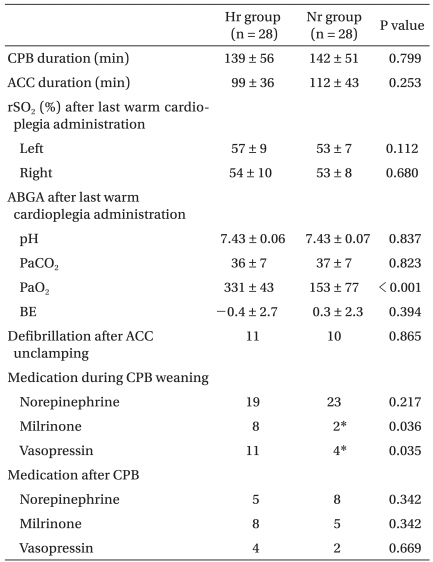
The CPB and ACC times were similar between the two groups. The results of arterial blood gas analysis after the last warm cardioplegia administration was not significantly different, except for the low oxygen partial pressure in the normoxic group. The rSO2 result after the last warm cardioplegia administration was similar in both groups. The arterial oxygen partial pressure after an oxygen fraction of 0.4 in the normoxic group for 8 patients between 80 and 100 mmHg, 15 patients between 100 and 200 mmHg, and 5 patients >200 mmHg. From the last warm cardioplegia administration to the 1 min after ACC off was 21.2 ± 7.9 min.
The frequency of using norepinephrine during weaning from CPB was not different. The dose of using norepinephrine from re-warming to weaning from CPB was 0.10 off was between the groups were compar and 0.14 of using nog/min in the normoxic goup; there were no differences between the groups (P = 0.337). But, the number of patients using vasopressin and milrinone was significantly less in the normoxic group. Other variables related the weaning from CPB were unremarkable (Table 2).
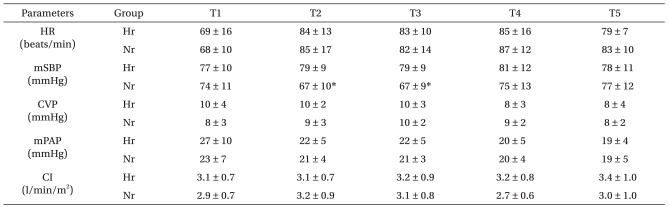
The changes in hemodynamic variables before and after surgery were not significantly different, except that the mean arterial pressure 1 hr after weaning of CPB and after sternum closure in the normoxic reperfusion group were significantly lower in the normoxic goup (Table 3).
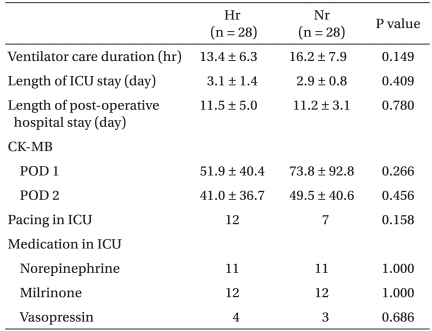
There were no significant differences in the cardiac enzyme levels after surgery, the period of mechanical ventilator support, the frequency of cardiotonic medications, and the length of stay in the ICU and hospital (Table 4).
Discussion
This study was designed to evaluate the effect of arterial oxygen tension during reperfusion on myocardial recovery and hemodynamic improvement and short-term outcome in patients undergoing VHS. As a result, we know that the frequency of using cardiotropic drugs was decreased in the normoxic reperfusion group, but there were no specific effects in the hemodynamics and short-term outcomes and cardiac enzymes.
VHS has the possibility of reducing myocardial function by increasing afterload post-operatively, unlike the CABG surgery that improve myocardial function by increased coronary flow [1]. Also, for the reduction of myocardial injury associated with CPB, off-pump coronary artery bypass surgery (OPCAB) can replace CABG in high-risk patients for CPB complications [7]. But, VHS without CPB has not been generalized. Therefore, it is clinically important to find a method that reduces myocardial injury from ischemic-reperfusion for patients undergoing VHS.
The pathophysiology of ischemic-reperfusion injury has been evaluated, and there have been two main mechanisms proposed: calcium overload and formation of oxygen free radicals [2,8]. The injury related overproduction of oxygen free radicals was induced by a kind of redox reaction when the myocardium was exposed to oxygen, it produced oxygen free radicals by a heavy metal-catalyzed reaction. In the first 5 min after reperfusion, oxygen derived-superoxide anion (O2-), hydroxyl radical (•OH, the most important mediator in myocardial stunning), and peroxynitrite (ONOO-) were generated. They play an important role in reperfusion injuries [9-11]. Reperfusion activates polymorphonuclear neutrophils (PMNs), and as a result there is an over-production of oxygen free radicals by PMNs [10]. At this time, oxygen free radicals react to phospholipids, proteins (contraction proteins and enzymes), and thiols (SH), and make various cellular damages. They injure the sarcolemma by forming lipid and hydrogen peroxide, and weaken the membrane bound enzyme-system [11].
The production of these free radicals is proportionate to oxygen tension (PO2) during reperfusion [3,4]. Methods that have been studied to reduce ischemic-reperfusion injury include lowering blood pressure during reperfusion [12] and reducing blood flow during reperfusion [13], but one of the most vigorously researched methods is controlling arterial oxygen tension in order to reduce reperfusion injury [14,15]. In relation to these studies, one study reported that maintaining normal arterial oxygen tension (150 mmHg) during CPB in children with cyanotic congenital heart disease resulted in dramatically reduced levels of conjugated diens, which represents the lipid peroxidation levels of the heart, compared with patients that maintained high arterial oxygen tension [16]. A following study reported reduced levels of CK-MB, a biomarker indicating the extent of myocardial damage, in adult patients in which arterial oxygen tension was maintained in the normal range tension during CPB and reperfusion [17]. There is also a study reporting that maintaining arterial oxygen tension between 200 and 250 mmHg during CPB resulted in better recovery of cardiac function and effective improvement of aortic and coronary blood flow when compared with arterial oxygen tension of 400 and 450 mmHg [15].
This study was designed to evaluate the effect of arterial oxygen tension during reperfusion on myocardial recovery in high-risk patients undergoing VHS. Previous studies maintained normal arterial oxygen tension from the start of CPB and directly monitored the arterial oxygen saturation or oxygen tension during CPB [5,14]. Unfortunately, monitoring devices enabling continuous evaluation of arterial oxygen tension are not available in South Korea, and lowering oxygen tension during CPB without an appropriate monitoring device is unsafe. Also, depending on the patient's condition, the risk of hypoxia can increase during rewarming periods due to increased oxygen consumption. In fact, we observed oxygen tension falling to <100 mmHg in 28% of patients when lowering the FiO2 to 0.5.
The decision was thus made to observe whether controlling oxygen tension during the final reperfusion period (period of administrating warmed cardioplegia and blood and removing the ACC) can reduce myocardial injury due to ischemic-reperfusion. This period is usually as short as 5-10 minutes, and the risk of hypoxia is low due to the high flow rate of the CPB machine.
The patient group that maintained a normal arterial oxygen tension of 150 mmHg by reducing the FiO2 to 0.5 required a significantly lower dose of vasopressin and milrinone. Otherwise, hemodynamic variables and post-operative cardiac biomarkers and short-term prognosis was not different between the two groups. Drugs administered to maintain hemodynamic variables, which were primary end points, within the normal range are thought to be the reason for this lack of discrepancy.
Also, considering the fact that severe declines in systemic vascular resistance after CPB are closely related to disturbances in calcium homeostasis and oxidative stress due to ischemic-reperfusion injury [18]; lower rates of vasopressin or milrinone administration in the normoxic group means that incidences of severe hypotension or low cardiac output were lower in this group. Therefore, it can be said that controlling oxygen tension during reperfusion is effective in cardioprotection.
The mean arterial pressures were higher in the hyperoxic group 1 hour post-CPB and sternum closure. This is thought to represent rebound hypertension occurring in more patients in the hyperoxic group when vascular tension recovers from the dilated state that occurred while weaning from CPB. The mean arterial pressure was maintained around 70 mmHg in the normoxic group, and there was no difference in the amount of peripheral vasoconstrictor administration between the two groups. Interestingly, the number of patients requiring nicardipine due to high mean arterial pressures >80 mmHg was higher in the hyperoxic group (T2: 6 to 1, P = 0.04; T3: 11 to 1, P < 0.001). In previous studies, biomarkers of ischemic-reperfusion injury, such as CK-MB, was significantly lower in groups that maintained oxygen tension at 150 mmHg compared with hyperoxic groups [5]. In contrast, the present study showed no difference in biomarkers or short-term prognosis between the two groups. The reason for this discrepancy seems to be related to the fact that we were not able to maintain normal arterial oxygen tension throughout CPB and therefore all patients were reperfused with high oxygen tension cardioplegia at all times. Moreover, diverse responses between patients to the change in oxygen fraction seems to be a significant factor when considering that 11 patients in the normoxic group showed oxygen tensions >150 mmHg right before removal of ACC despite lowering the oxygen tension to normal levels. Also, compared to oxygen tensions of >400 mmHg in the hyperoxic groups of previous studies [5,15], the hyperoxic group of the present study showed oxygen tensions between 250 and 350 mmHg, leading to smaller differences between the groups.
Because oxygen tensions were controlled with the beginning of administration of warmed cardioplegia, measuring the oxygen tension of cardioplegia was needed in order to measure the oxygen tension of the initial reperfusion fluid. There was no difference in oxygen tension between the cardioplegia and arterial blood, and the arterial blood was administered through the aortic cannula, thus this does not seem to have affected the accuracy of this study.
In addition, patients undergoing VHS were enrolled in this study which may lead to various degrees of myocardial injury, depending on the type of surgery, whereas previous studies were conducted in patients undergoing CABG. It increased the SD of cardiac enzymes after surgery, and the number of patients in this study was insufficient; however, the primary end point in this study was a difference of hemodynamic variables, not cardiac enzymes.
Therefore, although there were no significant improvements in levels of cardiac biomarkers or short-term prognosis, the reduced amount of administered peripheral vasoconstrictors and inotropes after only a short period of oxygen tension modulation seems to be of clinical importance. Vasoconstrictors and inotropes administered during CPB means hemodynamic instability after reperfusion, and influences the prognosis and complications of the patient post-operatively [19,20].
As a result, we lowered the oxygen fraction of 0.7 to 0.5 from the administration of last cardioplegia to 1 min after ACC to reduce reperfusion injury during VHS, there were no specific effects at the hemodynamics and short-term outcome and cardiac enzymes, but the frequency using cardiotropic drugs was decreased in the normoxic reperfusion group. Reduced oxygen tension during reperfusion after aortic unclamping on CPB is thought that convenient and safe supportive management technique to reduce reperfusion injury.