1. Carmichael P, Carmichael AR. Acute renal failure in the surgical setting. ANZ J Surg 2003; 73: 144-153. PMID:
12608979.


2. Tang IY, Murray PT. Prevention of perioperative acute renal failure: what works? Best Pract Res Clin Anaesthesiol 2004; 18: 91-111. PMID:
14760876.


3. Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 2004; 8: R204-R212. PMID:
15312219.



4. Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 2007; 11: R31PMID:
17331245.



5. Moore EM, Simpson JA, Tobin A, Santamaria J. Preoperative estimated glomerular filtration rate and RIFLE-classified postoperative acute kidney injury predict length of stay post-coronary bypass surgery in an Australian setting. Anaesth Intensive Care 2010; 38: 113-121. PMID:
20191786.


6. Bennet SJ, Berry OM, Goddard J, Keating JF. Acute renal dysfunction following hip fracture. Injury 2010; 41: 335-338. PMID:
19729159.


7. Thakar CV, Kharat V, Blanck S, Leonard AC. Acute kidney injury after gastric bypass surgery. Clin J Am Soc Nephrol 2007; 2: 426-430. PMID:
17699447.


8. Lassnigg A, Schmid ER, Hiesmayr M, Falk C, Druml W, Bauer P, et al. Impact of minimal increases in serum creatinine on outcome in patients after cardiothoracic surgery: do we have to revise current definitions of acute renal failure? Crit Care Med 2008; 36: 1129-1137. PMID:
18379238.


9. Bihorac A, Yavas S, Subbiah S, Hobson CE, Schold JD, Gabrielli A, et al. Long-term risk of mortality and acute kidney injury during hospitalization after major surgery. Ann Surg 2009; 249: 851-858. PMID:
19387314.


10. Abelha FJ, Botelho M, Fernandes V, Barros H. Determinants of postoperative acute kidney injury. Crit Care 2009; 13: R79. PMID:
19463152.



11. Karkouti K, Wijeysundera DN, Yau TM, Callum JL, Cheng DC, Crowther M, et al. Acute kidney injury after cardiac surgery: focus on modifiable risk factors. Circulation 2009; 119: 495-502. PMID:
19153273.


12. Kheterpal S, Tremper KK, Heung M, Rosenberg AL, Englesbe M, Shanks AM, et al. Development and validation of an acute kidney injury risk index for patients undergoing general surgery: results from a national data set. Anesthesiology 2009; 110: 505-515. PMID:
19212261.


13. Hobson CE, Yavas S, Segal MS, Schold JD, Tribble CG, Layon AJ, et al. Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation 2009; 119: 2444-2453. PMID:
19398670.


14. Hansen MK, Gammelager H, Mikkelsen MM, Hjortdal VE, Layton JB, Johnsen SP, et al. Post-operative acute kidney injury and five-year risk of death, myocardial infarction, and stroke among elective cardiac surgical patients: a cohort study. Crit Care 2013; 17: R292. PMID:
24330762.



15. Bucaloiu ID, Kirchner HL, Norfolk ER, Hartle JE 2nd, Perkins RM. Increased risk of death and de novo chronic kidney disease following reversible acute kidney injury. Kidney Int 2012; 81: 477-485. PMID:
22157656.


16. Shirabe K, Kajiyama K, Harimoto N, Tsujita E, Wakiyama S, Maehara Y. Risk factors for massive bleeding during major hepatectomy. World J Surg 2010; 34: 1555-1562. PMID:
20182718.


17. Jones DR, Lee HT. Perioperative renal protection. Best Pract Res Clin Anaesthesiol 2008; 22: 193-208. PMID:
18494397.


18. von Elm E, Altman DG, Egger M, Pocock SJ, G├Ėtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147: 573-577. PMID:
17938396.


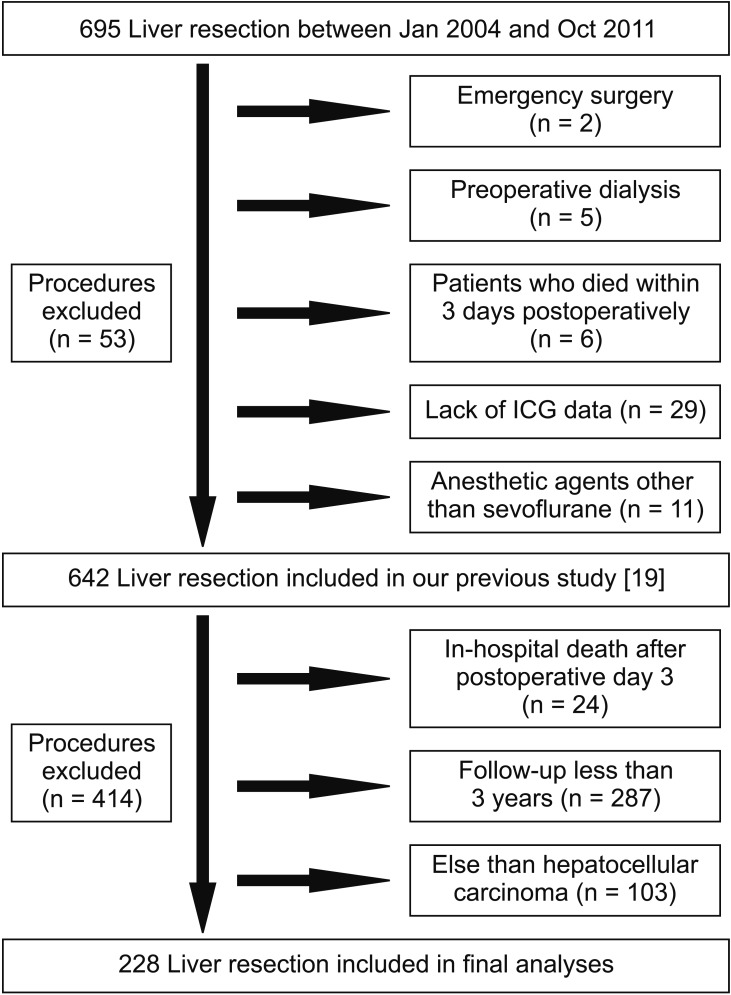
19. Tomozawa A, Ishikawa S, Shiota N, Cholvisudhi P, Makita K. Perioperative risk factors for acute kidney injury after liver resection surgery: an historical cohort study. Can J Anaesth 2015; 62: 753-761. PMID:
25925634.


20. Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53: 982-992. PMID:
19339088.


21. Kalamas AG, Niemann CU. Patients with chronic kidney disease. Med Clin North Am 2013; 97: 1109-1122. PMID:
24182722.


22. Jacques F, El-Hamamsy I, Fortier A, Maltais S, Perrault LP, Liberman M, et al. Acute renal failure following lung transplantation: risk factors, mortality, and long-term consequences. Eur J Cardiothorac Surg 2012; 41: 193-199. PMID:
21665487.



23. Okusa MD, Chertow GM, Portilla D. The nexus of acute kidney injury, chronic kidney disease, and World Kidney Day 2009. Clin J Am Soc Nephrol 2009; 4: 520-522. PMID:
19225036.



24. Ishani A, Xue JL, Himmelfarb J, Eggers PW, Kimmel PL, Molitoris BA, et al. Acute kidney injury increases risk of ESRD among elderly. J Am Soc Nephrol 2009; 20: 223-228. PMID:
19020007.



25. Ishani A, Nelson D, Clothier B, Schult T, Nugent S, Greer N, et al. The magnitude of acute serum creatinine increase after cardiac surgery and the risk of chronic kidney disease, progression of kidney disease, and death. Arch Intern Med 2011; 171: 226-233. PMID:
21325112.


26. Augoustides JG. Serum creatinine as a perioperative biomarker: a challenge for perioperative management and an opportunity for the Cardiothoracic Surgery Trials Network. J Thorac Cardiovasc Surg 2012; 143: 523-524. PMID:
22244568.


27. Basile DP. Rarefaction of peritubular capillaries following ischemic acute renal failure: a potential factor predisposing to progressive nephropathy. Curr Opin Nephrol Hypertens 2004; 13: 1-7. PMID:
15090853.