 |
 |
| Korean J Anesthesiol > Volume 74(3); 2021 > Article |
|
Pediatric difficult airway is defined as a situation wherein the operator (anesthesiologist or intensivist) experiences difficulty with mask ventilation, direct or assisted laryngoscopy, tracheal intubation, supraglottic airway device use, or surgical airway. It is a clinical scenario that can quickly escalate into an emergency, and it is a risk factor for morbidity and mortality. The incidence of difficult tracheal intubation is up to 3%, and 1 of 5 cases are unanticipated (mostly related to unidentified facial dysmorphic features). Complications occur in ≥ 20% of children (mainly hypoxemia), and they are frequently associated with repeated attempts at laryngoscopy (≥ 3 attempts) and intubation (≥ 2 attempts) [1].
Written informed consent for the publication of this article was obtained from the parents of the patients.
We present the case of 2 toddlers with Pierre Robin sequence and difficult airway, who underwent rescue intubation with an i-gel® (Intersurgical Ltd, Wokingham, Berkshire, UK) supraglottic airway device during the perioperative care of cleft palate surgery. Both were 20-month-old children who were classified as American Society of Anesthesiologists physical status II and weighed 9–10 kg. Multiple attempts at laryngoscopy (Cormack-Lehane ≥ 3b) and videolaryngoscopy were performed by experienced pediatric operators, and episodes of desaturation (with abundant secretions and some blood) occurred in both cases [2]. Considering the difficult airway, repeated attempts at laryngoscopy, and hypoxemia episodes, we decided to perform intubation using a supraglottic airway device. We inserted an i-gel® airway device (nº 2) for mechanical ventilation and performed a fibroscopy (2.8 mm) through a double-swivel elbow (with seal-opening), while visualizing the following structures: epiglottis partially covering the larynx (classification of fiber optic vision through supraglottic device grade 3-4), larynx with supraglottic edema and secretions, trachea, and carina [3]. We passed an uncuffed tracheal tube (nº 4) through the elbow (maintaining mechanical ventilation), removed the supraglottic device using another tracheal tube as a stabilizer, and connected it again to the ventilator. Finally, we checked the waveform capnography and the correct placement of the tube proximal to the carina by performing a new fibroscopy again.
Pierre Robin sequence is defined as the presence of micrognathia, glossoptosis, and airway obstruction (as well as cleft palate in 50% of patients); it is associated with respiratory and feeding difficulties to varying degrees. The incidence varies from 1 : 5,000 to 1 : 85,000, owing to variable clinical presentations, which may lead to underdiagnosis of patients with mild symptoms who may present with unanticipated difficult airways [4]. The latter occurred in 1 patient who had not been diagnosed with the Pierre Robin sequence when scheduled for surgery. The second child had a history of the Pierre Robin sequence. However, as his anatomical conditions seemed favorable, the anesthesiologist decided to perform a direct laryngoscopy under sedation as a first approach to case management.
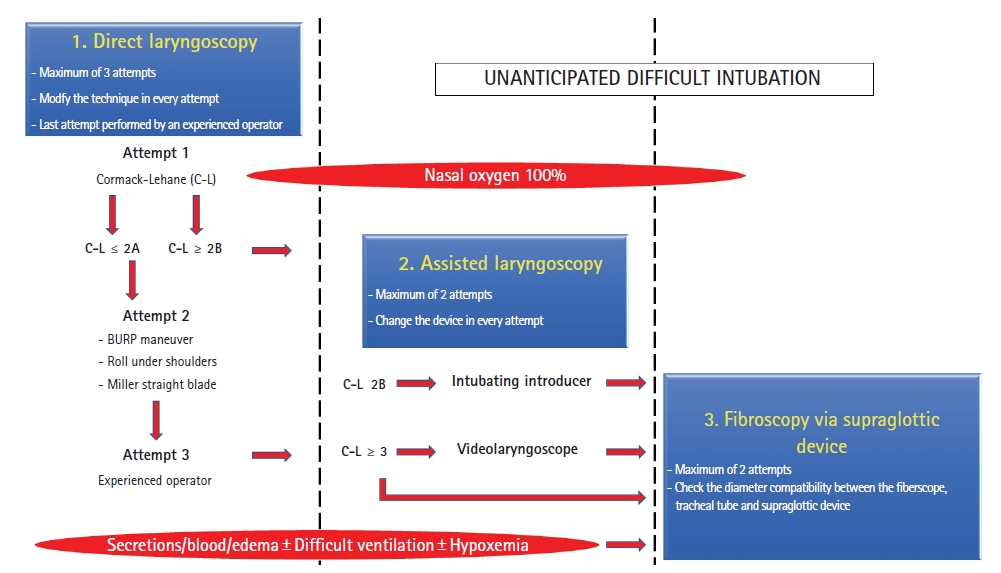
The management of unanticipated difficult tracheal intubation in pediatric patients should be based on early identification and the use of evidence-based algorithms. Such algorithms should be adapted to the available resources and clinical experience and simplified to the minimum necessary information to ensure the adherence of professionals and ease of use. Moreover, intubation attempts should be limited, techniques and/or operators should be changed at every attempt, and intubation assistance devices should be used promptly. The damage produced by repeated attempts at intubation (secretions, bleeding, and supraglottic edema) may compromise ventilation and oxygenation. Supraglottic airway devices are the best choice for rescue ventilation, and they can be used as conduits for intubation (Video 1). Fibroscopy-guided intubation through a supraglottic device is well described in the literature, but however, guidelines for the difficult airway management indicate to perform this technique in the late stages of the process [5].
i-gel® supraglottic airway devices have an optimal profile for the management of difficult airways in children, given the ease of insertion (non-inflatable cuff), high leak pressures (> 25 cmH2O) that permits more demanding positive pressure ventilation, a gastric channel for decompression of the stomach, and a wide airway diameter that allows the introduction of endotracheal tubes and fiberscopes with different diameters [6].
Fibroscopy-guided intubation through a supraglottic airway device has higher rates of global success, higher rates of first-attempt success in children younger than 1 year, and lower rates of hypoxemia than videolaryngoscopy (permits mechanical ventilation during the procedure). Since laryngoscopy and videolaryngoscopy are performed in apnea cases, they may be associated with hypoxemia, a higher number of intubation attempts (given the need to interrupt the technique for patient ventilation), and more airway damage. It is also important to check the compatibility of the diameters of the fiberscope, tracheal tube, and supraglottic airway device and examine the passage of the tracheal tube through the elbow with seal-opening to complete the intubation procedure without disconnecting from mechanical ventilation [6,7].
Therefore, based on our experience, we strongly recommend the early use of fibroscopy-guided intubation using the i-gel® supraglottic device for unanticipated tracheal intubation with a Cormack-Lehane ≥ 3 (Fig. 1) or secretions, bleeding, or hypoxemia to achieve a high success rate. Although the first-line supraglottic devices for this technique are Air-Q® and Aura-i® (having more studies published), i-gel® has the following advantages over them: (1) provides a wider airway channel that provides better visual field and permits the passage of tracheal tubes and fiberscopes with larger diameters; (2) obviates the need to disconnect mechanical ventilation for the passage of tracheal tubes, unlike with the use of Air-Q®.
In conclusion, we consider fibroscopy-guided intubation through a supraglottic device as a safe and effective procedure, which should be performed promptly as an intubation rescue technique in pediatric patients, since it reduces the number of attempts at laryngoscopy and intubation. Moreover, we consider i-gel® as an excellent supraglottic device for performing this procedure, although further studies providing new evidence on its application are needed.
NOTES
Author Contributions
Ramón Eizaga Rebollar (Conceptualization; Supervision; Writing – original draft; Writing – review & editing)
Elena Borreiros Rodríguez (Data curation; Resources)
Ana Mercedes Martínez-Almendros Fernández (Investigation; Resources)
Paula Lozano Hierro (Investigation; Methodology; Resources)
Luis Miguel Torres Morera (Supervision; Writing – review & editing)
Fig. 1.
Algorithm for the management of unanticipated difficult intubation in our pediatric anesthesia program. BURP: backward upward rightward pressure.
References
1. Fiadjoe JE, Nishisaki A, Jagannathan N, Hunyady AI, Greenberg RS, Reynolds PI, et al. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med 2016; 4: 37-48.


3. Park C, Bahk JH, Ahn WS, Do SH, Lee KH. The laryngeal mask airway in infants and children. Can J Anaesth 2001; 48: 413-7.


4. Cladis F, Kumar A, Grunwaldt L, Otteson T, Ford M, Losee JE. Pierre Robin sequence: a perioperative review. Anesth Analg 2014; 119: 400-12.


5. Black AE, Flynn PE, Smith HL, Thomas ML, Wilkinson KA. Development of a guideline for the management of the unanticipated difficult airway in pediatric practice. Paediatr Anaesth 2015; 25: 346-62.


6. Jagannathan N, Ramsey MA, White MC, Sohn L. An update on newer pediatric supraglottic airways with recommendations for clinical use. Paediatr Anaesth 2015; 25: 334-45.


7. Burjek NE, Nishisaki A, Fiadjoe JE, Adams HD, Peeples KN, Raman VT, et al. Videolaryngoscopy versus fiber-optic intubation through a supraglottic airway in children with a difficult airway: an analysis from the multicenter pediatric difficult intubation registry. Anesthesiology 2017; 127: 432-40.


- TOOLS









