Postoperative delirium in elderly patients with critical limb ischemia undergoing major leg amputation: a retrospective study
Article information
Abstract
Background
Critical limb ischemia has been identified as a risk factor for the incidence of postoperative delirium in elderly patients. Limb amputation is the last option in critical limb ischemia treatments. We investigated the incidence and predisposing factors of postoperative delirium in patients undergoing major leg amputation.
Methods
From January 2012 to December 2016, 121 patients aged over 60 years who had undergone major leg amputation were enrolled in this study. Various factors related to the patients’ outcomes were assessed, including demographic, preoperative laboratory, anesthetic, surgical, and postoperative indicators.
Results
Twenty two patients were excluded and 99 patients were assigned to either the delirium group or no delirium group. Forty of them (40%) developed a delirium during 30 days postoperatively. Univariate analysis implied that end-stage renal disease on hemodialysis, alcohol consumption, C-reactive protein, staying in an intensive care unit (ICU), duration of an ICU stay, occurrence of complications, and mortality during six months, were the factors that accounted for significant differences between the two groups. In multivariate analysis, three factors were significantly related to the development of delirium: mortality during six months (odds ratio [OR] = 13.86, 95% CI [2.10–31.90]), alcohol (OR = 8.18, 95% CI [1.13–16.60]), and hemodialysis (OR = 4.34, 95% CI [2.06–93.08]).
Conclusions
Approximately 40% of the elderly patients suffered from postoperative delirium in major leg amputation. Identifying those with risk factors for postoperative delirium and intervening at the early stage will be of great benefit in major leg amputations for the elderly population.
Introduction
Postoperative delirium is defined as an acute change in cognitive status characterized by fluctuating consciousness and inattention, occurring within 30 days after a surgery [1]. The incidence of postoperative delirium varies from 2% to 72%, with higher rates among elderly patients [2]. The significance of etiological parameters differs, depending on the studies; however, old age has been proven to be a common predisposing factor [3]. A reduced cognitive reserve of elderly patients is a greater risk for delirium or cognitive decline in the postoperative period [4]. As the population of the elderly has been growing over decades, the occurrence of postoperative delirium will also continue to increase.
Postoperative delirium results in a prolonged recovery time, difficulty in postoperative care, longer intensive care unit and hospital stays, as well as higher mortality and morbidity rates [5]. The assessment of risk factors is important for preventing and managing delirium in patients. However, fluctuating symptoms may lead to delays of the diagnosis and treatment. In the hypoactive delirium subtype, which is more common in the elderly, the patient outwardly seems calm or somnolent, so it is frequently missed, although related with a poor prognosis [1,6].
Critical limb ischemia is the most advanced form among the peripheral artery diseases and has been identified as a risk factor for postoperative delirium in elderly patients [3]. Limb amputation is the last option when revascularization is no longer possible in critical limb ischemia treatments [7]. The identified risk factors of postoperative delirium in lower limb ischemia are age, end-stage renal failure, multiple occlusive lesions, cognitive impairment, and critical limb ischemia [2]. However, no study has specifically analyzed the occurrence and risk factors of postoperative delirium in patients with critical limb ischemia with a focus on only major leg amputation surgery. A few investigations exist that included amputated populations and were associated with postoperative delirium in critical limb ischemia, but they either contained various types of amputation surgery or enrolled only a small number of patients with a major amputation [8–10]. We aimed to investigate the incidence and perioperative predisposing factors of postoperative delirium in elderly patients undergoing a major leg amputation.
Materials and Methods
Ethical approval for this retrospective study was obtained from the Institutional Review Board of our hospital. Patients who were 60 years or older undergoing major leg amputation from January 2012 to December 2016 were recruited and followed up for six months. They were either assigned to a delirium group or a no delirium group. Postoperative delirium was assessed using the Confusion Assessment Scale (CAM), which is sensitive, specific, reliable and easy to use for the identification of delirium [11]. The presence of delirium was evaluated once a day, for 30 days postoperatively.
Demographic data including gender, age, height, weight, body mass index, and the physical status according to the American Society of Anesthesiologists were collected through chart reviews. The physical performance status was scored with the Eastern Cooperative Oncology Group (ECOG) scale; 0: Fully active, able to carry on all pre-disease performance without restriction, 1: Restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature, 2: Ambulatory and capable of all selfcare but unable to carry out any work activities. Up and about more than 50% of waking hours, 3: Capable of only limited selfcare, confined to bed or chair more than 50% of waking hours, 4: Completely disabled. Cannot carry on any selfcare. Totally confined to bed or chair, 5: Dead [12]. Comorbidities were divided into the following categories: hypertension, diabetes mellitus, end-stage renal disease on hemodialysis, cardiac (angina pectoris, myocardial infarction, rhythm disorder, valve disorder, cardiomyopathy, and heart failure), neurologic (cerebrovascular accident, transient ischemic attack, and Parkinson’s disease), renal (acute renal failure, chronic renal failure, glomerulopathy, and glomerulonephritis), pulmonary (chronic obstructive disease and asthma), and hepatic (liver cirrhosis) diseases. Other predisposing factors such as alcohol, smoking, visual and hearing aids were also evaluated. Alcohol consumption was marked if more than one drink of distilled alcohol or a bottle of beer was consumed two or more times a week.
Preoperative laboratory variables were hemoglobin, sodium, potassium, blood urea nitrogen (BUN), creatinine, albumin, total protein, the erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), fasting blood sugar (FBS), PaO2, and PaCO2.
Anesthetic and surgical data were extracted from the anesthesia records. Types of anesthesia (general or regional anesthesia), anesthesia duration, types of operation (above or below knee amputation), duration of the operation, estimated blood loss (EBL), transfusion of blood products, and use of inotropics were included in the operative data.
Postoperatively, patients were evaluated by intensive care unit (ICU) stays, duration of ICU stays, occurrence of complications, as well as hospital stays and mortality during six months.
All statistical analyses were performed using the SPSS statistics software (version 20.0, IBM Corp., USA). Differences in categorical values were assessed using the chi-square test. If more than 20% of the expected frequencies were less than 5, Fisher’s exact test was conducted. The Kolmogorov-Smirnov test was used to test for normality in continuous variables. Group differences were tested using the Mann-Whitney U test or student t tests as applicable. P values less than 0.05 were considered significant. Variables with statistical significance in univariate analyses were assessed by multivariate logistic regression analysis to determine the degree of the variables’ association with the odds ratio (OR) and 95% CI.
Results
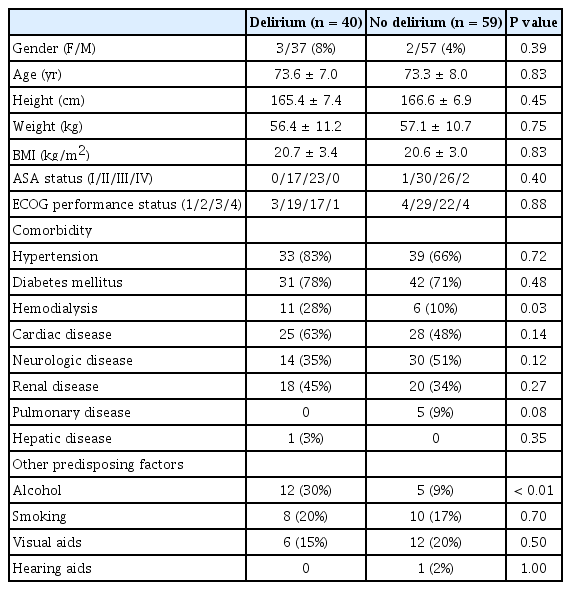
Out of the 121 patients, 99 patients were included in the study. Twenty two were excluded because of pre-existing dementia and mental changes, communication difficulty, and a concomitant additional surgery. Forty of the 99 subjects (40%) undergoing major leg amputation postoperatively developed a delirium during 30 days. Physical characteristics (gender, age, height, weight, and body mass index), American Society of Anesthesiologists status, and ECOG performance status were similar in both the delirium and no delirium groups (Table 1). In a comparison of comorbidities, only end-stage renal disease on hemodialysis was significantly higher in the delirium group (28%) than in the no delirium group (10%) (P = 0.025). The number of patients who ingested more than one drink of distilled alcohol or a bottle of beer two or more times a week was significantly different between the groups (30% vs. 9%, P < 0.01).
With regard to the preoperative laboratory variables, the CRP level in the delirium group of 143.1 ± 84.6 mg/L was significantly higher than in the no-delirium group with 93.9 ± 81.4 mg/L (P < 0.01) (Table 2).
There were no significant differences related to types of anesthesia (general or regional anesthesia), anesthesia duration, types of operation (above or below knee amputation), duration of the operation, EBL, transfusion of blood products, and use of inotropics during the procedure (Table 3).
Postoperatively, the number of patients who were treated in an ICU was higher in the delirium group (24/40, 60%) than in the no delirium group (15/59, 25%) (P < 0.01) and the mean durations of ICU stays also differed between the two groups (17.2 ± 15.6 days vs. 7.8 ± 12.1 days, P = 0.04, respectively) (Table 4). The rate of complications was higher in the delirium group (11/40, 28%) than in the no delirium group (5/59, 8%) (P = 0.02). The types of postoperative complication were sepsis, septic shock, pneumonia, wound problems, heart failure, acute renal failure, and multi-organ failure. The mortality during six months was also significantly higher in the delirium group (14/40, 35%) than in the no delirium group (3/59, 5%) (P < 0.01).
The univariate analysis indicated that end-stage renal disease on hemodialysis, alcohol consumption, CRP, ICU stays, duration of ICU stays, occurrence of complications, and mortality during six months were the factors that accounted for the differences between the two groups and they were further evaluated in a multivariate logistic regression analysis (Table 5). Three factors were significantly related to the development of delirium: mortality during six months (OR = 13.86, 95% CI [2.10–31.90]), alcohol (OR = 8.18, 95% CI [1.13–16.60]), and end-stage renal disease on hemodialysis (OR = 4.34, 95% CI [2.06–93.08]).
Discussion
In this retrospective study, the incidence of delirium following major leg amputation was 40% postoperatively. Endstage renal disease on hemodialysis, alcohol consumption, the preoperative CRP level, the number of patients treated in an ICU, durations of ICU care, as well as rates of complication and mortality during six months were significantly different between the two groups. Among those variables, mortality during six months, alcohol, and hemodialysis were significantly related to the development of delirium in multivariate logistic regression. Alcohol and hemodialysis could be regarded as independent predicting factors of delirium. For the mortality during six months, its preceding relationship to delirium is unclear, so we could not affirm it to be a predicting factor.
The incidence of postoperative delirium varies depending on the types of procedure. In patients who underwent vascular surgery such as aortic, carotid, endovascular, bypass, endarterectomy, arteriovenous shunt, percutaneous intervention, and amputation, the occurrence ranged from 5% to 43% [5,8–10,13]. Two published incidence rates of delirium after any kind of leg amputation were 17% [9] and 20% [10]. One study reported that the incidence rate associated with major leg amputation (below and above knee amputations) was 61% (11/18) [8].
Amputation surgery was established as a predictor of postoperative delirium occurrence in vascular surgical procedures [9,10]. Critical limb ischemia is frequently related to systemic atherosclerosis and its negative impacts on patients’ outcomes [14]. In addition, systemic atherosclerosis contributes to cognitive decline in elderly patients and cognitive impairment is a well-known risk factor for delirium [15,16]. However, to our knowledge, no study has specifically investigated the incidence and risk factors of delirium after surgery with a sole focus on only lower limb amputation which this investigation of major leg amputation (below and above knee amputations) did. Limb ischemia is often accompanied by limitations of physical performance, which is a significant risk factor for delirium [17]. The ECOG scale for performance status was applied to all patients at admission to evaluate their daily living abilities [12]. Most patients (88%, 87/99) were on grade 2 or 3, which indicated they were unable to carry out any work activities or that they were only capable of limited selfcare. Five percent (5/99) of the patients were even completely disabled and could not carry on any selfcare. However, our results revealed no significant correlation between daily functioning and delirium.
The rate of delirium in our study was 40% (40/99), which is slightly lower compared with research by van Eijsden et al. [8] where 11 out of 18 patients (61%) undergone major amputation surgery. However, in that study, the number of subjects with amputation procedures was small and all included critical limb ischemia patients were relatively old, with a median age of 78 years (interquartile range of 71–82 years). Our patients’ median age was 71 years (interquartile range 69–78 years) and the mean age was similar in both the delirium and no delirium group (73.6 ± 7.0 vs. 73.3 ± 8.0, respectively). Although we could not establish a relationship between delirium and age, advanced age has been identified as a strong risk factor for postoperative delirium [3,5,9]. Age represents a potent risk factor for delirium, probably due to the accumulation of medical and other comorbidities with declined reserves throughout later life [18].
A recent study on lower limb ischemia reported that endstage renal disease is an important risk factor of delirium, suggesting that delirium with an increased BUN level may result from the general metabolic disturbance associated with renal insufficiency rather than from a high BUN alone [5]. Fukunishi et al. [19] suggested that two factors, advanced age and long-term hemodialysis, were closely related to the delirium development in patients on hemodialysis therapy. The presence of end-stage renal disease on hemodialysis was investigated as an independent significant predictor among several comorbidities in our study. However, the electrolyte imbalance did not contribute to delirium occurrence. Serum creatinine levels were similar in both groups (2.6 ± 2.7 mg/dl vs. 2.2 ± 2.6 mg/dl, P = 0.468, respectively). The BUN level was higher in the delirium group (31.3 ± 18.2 mg/dl vs. 25.0 ± 15.4 mg/dl) but with a low statistical significance (P = 0.06). Cognitive impairment in dialysis is thought to be associated with cerebrovascular disease and increased mortality [20].
Alcohol consumption is known as an independent risk factor for delirium in some surgeries [21]. In that report, authors determined alcohol abuse if patients consumed more than one drink or bottle of beer on a daily basis in colorectal surgery for carcinoma. In the subjects with critical limb ischemia undergoing surgery, daily intake of alcohol was a potential risk factor in the univariate analyses, but the multivariate analysis did not confirm it as an independent predicting factor [8]. It should be noted that we defined alcohol consumption extensively, compared to previous studies. However, defining alcohol consumption and abuse, as well as quantifying the amount of consumed alcohol is not as easy as commonly thought. Alcohol consumption might have been estimated inaccurately which is one of our study’s weak points.
The definitive pathophysiological process of delirium remains uncertain but inflammation has been proposed as one of the possible mechanisms. There exists evidence about the relationship of CRP with neuroinflammatory processes. CRP is associated with the activation of vascular endothelial cells, a process that may explain the susceptibility of patients with organic brain disease to delirium caused by systemic inflammatory conditions [22]. Although there are conflicting research findings about CRP in delirium, one study revealed that CRP levels at or soon after admission appear to be highly predictive of delirium and recovery in acute medical inpatients [23]. Another investigation even demonstrated that with an increase in the postoperative CRP level to 100 mg/L, the risk of delirium after surgery increased by almost 90% [10]. In the present study, preoperative CRP was identified as a potential risk factor for delirium in univariate analysis, but we did not find the relationship between the elevated CRP levels and the occurrence of delirium in our multivariate evaluation.
The CAM has been widely used as a standardized tool for the identification of delirium and was developed for non-psychiatrically trained personnel [24], but its sensitivity was as low as 50% when used by individuals with minimal training [25]. In this study, registered nurses in clinical wards administered the CAM to the patients but individual variation with regard to the degree of training could still exist. A delirium diagnosis needs to be confirmed by skilled physicians, using elaborate criteria such as in the DSM (Diagnostic and Statistical Manual of Mental Disorders) or the ICD-10 (International Statistical Classification of Diseases and Health-related Problems, 10th revision). The possibility of inaccurate diagnosis is one of the limitations in our study.
In conclusion, this study investigated the incidence and risk factors of postoperative delirium following major leg amputation. We found that approximately 40% of the elderly patients suffered from delirium after major leg amputation. Among the perioperative variables, mortality during six months, alcohol, and hemodialysis were significantly related to the development of delirium. Patients with an elevated CRP level in the preoperative evaluation, ICU stays, longer duration of ICU stays, and postoperative complications, tended towards delirium development in the postoperative period. An accurate diagnosis, early intervention, and appropriate management of elderly patients with risk factors for postoperative delirium in leg amputation surgery need to be taken into consideration by physicians.