|
 |
| Korean J Anesthesiol > Volume 76(4); 2023 > Article |
|
Abstract
Background
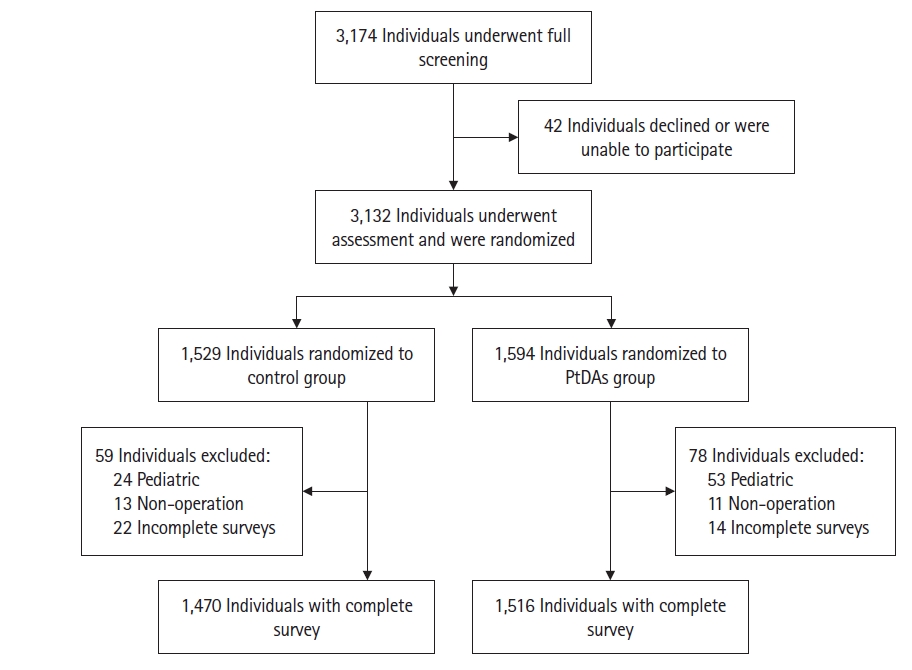
Methods
Results
Acknowledgments
NOTES
Funding
The authors received no specific funding for this study. This work was supported by a research grant from the Chi Mei Medical Center and Taipei Medical University (Grant No. 107CM-TMU-12). The sponsoring organization was not involved in the study design, data analysis, or interpretation.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
Li-Kai Wang (Data curation; Formal analysis; Investigation)
Yao-Tsung Lin (Data curation; Formal analysis; Investigation)
Jui-Tai Chen (Data curation; Formal analysis; Investigation)
Winnie Lan (Formal analysis; Writing ŌĆō original draft)
Kuo-Chuan Hung (Data curation; Investigation)
Jen-Yin Chen (Data curation; Investigation)
Kuei-Jung Liu (Data curation; Investigation)
Yu-Chun Yen (Formal analysis; Investigation)
Yun-Yun Chou (Formal analysis; Investigation)
Yih-Giun Cherng (Conceptualization; Formal analysis; Investigation; Methodology; Project administration; Resources; Supervision; Writing ŌĆō review & editing)
Ka-Wai Tam (Conceptualization; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Supervision; Writing ŌĆō review & editing)