 |
 |
| Korean J Anesthesiol > Volume 73(5); 2020 > Article |
|
Obesity in surgical patients presents with numerous challenges for anesthesiologists. Difficult airways, associated comorbidities, and postoperative pulmonary and thromboembolic complications are some of the difficulties encountered. Combining regional blocks with general anesthesia helps overcome many of these difficulties by reducing the opioid requirement and decreasing the incidence of postoperative nausea/vomiting, thus allowing early ambulation [1]. Regional blocks are quite popular and efficacious in the management of pain associated with breast surgeries and form an important component of multimodal pain management. Amongst them, thoracic epidural and thoracic paravertebral block (TPVB) are most commonly used, but they may be associated with complications, such as accidental dural puncture, epidural abscess/hematoma, spinal cord injury, pneumothorax etc. Moreover, these techniques might be technically difficult in patients with obesity even under ultrasound guidance. In the quest of safer techniques, novel blocks or alternative approaches to existing techniques have been devised to be pain free with minimal inherent risks. One such approach of the paravertebral block has recently been introduced as the “mid-transverse process to pleura” (MTP) block [2].
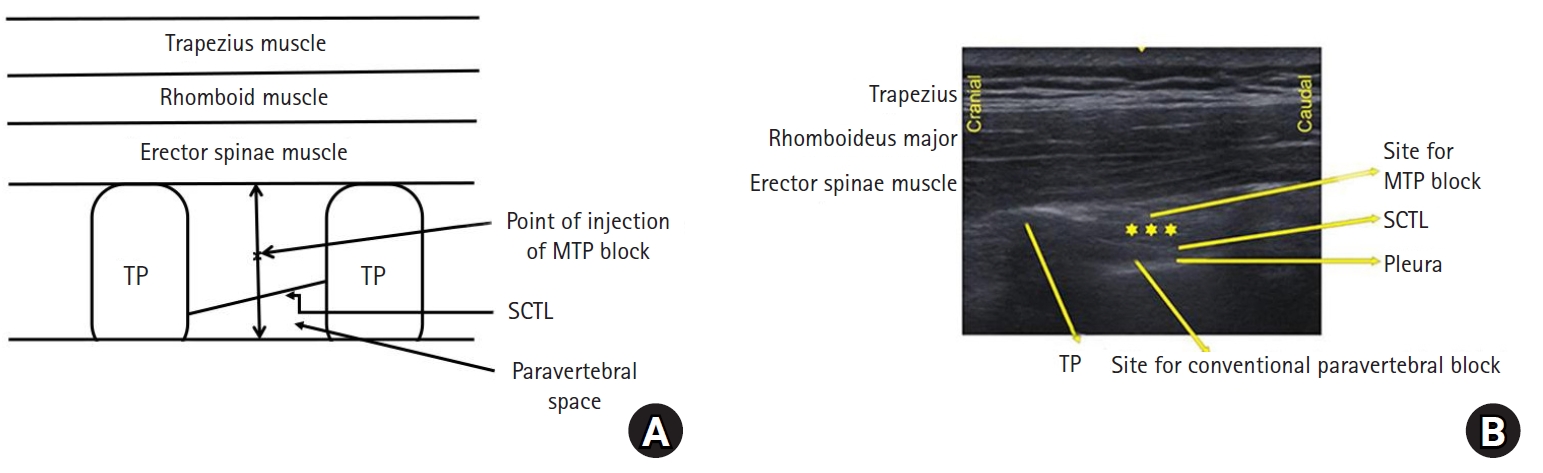
A 64-year-old woman with morbid obesity, weighing 100 kg (body mass index: 41.66 kg/m2), was scheduled for modified radical mastectomy. She had known hypertension, type II diabetes mellitus, and obstructive sleep apnea. In the block room, the patient was premedicated with intravenous midazolam 1 mg and fentanyl 50 µg. In the sitting position and under sterile conditions, the T4 spine was palpated, and a high‑frequency linear ultrasound probe (LOGIQe, GE Healthcare, China) was placed longitudinally, approximately 2.5 cm lateral to the midline. After skin infiltration with a local anesthetic, a 100-mm short-bevel echogenic needle (Contiplex®, B. Braun, Germany) was inserted in-plane from the cranial to the caudal direction. The desired end point for the needle tip was the midpoint of the line between the posterior border of the transverse process and the pleura (Fig. 1A). A titrated bolus of 20 ml of 0.5% ropivacaine was injected at the target site after confirming the spread with 2 ml of normal saline (Fig. 1B). Thereafter, a 20-gauge catheter was threaded through the needle, with the catheter tip placed approximately 3 cm beyond the needle tip. Sensory mapping with a cold swab and pinprick with a 20-gauge needle over the anterior and lateral chest walls revealed a dermatomal block from T1 to T7 30 min after the administration. General anesthesia was induced in accordance with the institutional protocol. Intraoperatively, 0.5% ropivacaine infusion was maintained at 8 ml/h. The hemodynamic parameters were stable throughout the surgical procedure, with no further requirement of opioids after 150 µg of fentanyl administered at the anesthetic induction. Postoperatively, analgesia was maintained with intravenous paracetamol 1 g every 8 h and infusion of 0.2% of ropivacaine at the rate of 8 ml/h in the postoperative period up to 72 h. The patient required additional rescue analgesia in the third postoperative hour, which was induced with an injection of diclofenac 75 mg. Overall, postoperatively, her visual analogue scale score at rest and on movement remained in the ranges of 2–3/10 and 3–4/10, respectively, with analgesia maintained with a ropivacaine 0.2% infusion, paracetamol (1 g, 8 hourly), and a single rescue dose of diclofenac, as aforementioned. The patient was extremely satisfied, had ambulatory capacity, and had no pain or nausea/vomiting.
The reduced opioid requirement, decreased incidence of postoperative nausea and vomiting, early ambulation, and better recovery profile made the regional nerve blocks all the more important for multimodal pain management. With an increased use of ultrasound in regional anesthesia, the current trend is to go more peripheral and look for more specific targets depending on the desired outcome; thus, making the fascial and plane blocks more popular. The recently described fascial blocks for thoracic surgeries include the erector spinae plane, retrolaminar, intercostal paraspinal, and MTP blocks. The MTP block, described by Costache et al. [2] is the most recent one. It involves deposition of the drug midway between the transverse process and the pleura. Costache et al. [2] postulated that the local anesthetic deposited at this point may reach the paravertebral space through several possible mechanisms, such as medially through the gap between the superior costotransverse ligament (SCTL) and vertebral bodies, through fenestrations in SCTL, and laterally through the internal intercostal membrane. Syal et al. [3] described the role of this novel technique in a patient with multiple rib fractures with excellent pain relief, while Bhoi et al. [4] reported this block in three patients scheduled for modified radical mastectomy with favorable results. The present patient with morbid obesity was managed safely and successfully with multimodal analgesia with the MTP block. Postoperatively, continuous infusion of 0.2% ropivacaine met the analgesic requirements to a great extent. Only paracetamol was used as an adjunct, and a single rescue dose of diclofenac was required. A reduced opioid requirement was advantageous in avoiding postoperative nausea/vomiting, excessive sedation, respiratory depression, constipation, etc. All this helped the patient achieve early ambulation and recovery. The advantage of the MTP block over the conventional TPVB is that the visualization of SCTL is not required, which might be difficult in patients with obesity. The second advantage is that the target point of the needle is very superficial and far from structures, such as the pleura and neurovascular bundles, making this novel block much safer.
In conclusion, the MTP block is a safe option in patients with obesity scheduled for breast surgery, although well-designed controlled studies are warranted for evaluating the statistical significance.
NOTES
Author Contributions
Rashmi Syal (Conceptualization; Data curation; Visualization; Writing – original draft; Writing – review & editing)
Rakesh Kumar (Conceptualization; Data curation; Supervision; Writing – original draft; Writing – review & editing)
Swati Chhabra (Conceptualization; Data curation; Resources; Writing – original draft; Writing – review & editing)
Mussavvir Agha (Data curation; Resources; Writing – review & editing)
Fig. 1.
Mid-transverse process to pleura (MTP) block. (A) Schematic line diagram representing the needle position in the MTP block. (B) Ultrasound image of the MTP block with the transducer placed in a parasagittal orientation and an in-plane needle insertion.
TP: transverse process, SCTL: superior costotransverse ligament. *denotes the site for local anesthetic infiltration for the MTP block.
References
1. Ingrande J, Brodsky JB, Lemmens HJ. Regional anesthesia and obesity. Curr Opin Anesthesiol 2009; 22: 683-6.

2. Costache I, de Neumann L, Ramnanan CJ, Goodwin SL, Pawa A, Abdallah FW. The mid-point transverse process to pleura (MTP) block: a new end-point for thoracic paravertebral block. Anaesthesia 2017; 72: 1230-36.











