 |
 |
| Korean J Anesthesiol > Volume 72(2); 2019 > Article |
|
Abstract
Background
We investigated the effect of irrigation fluid on coagulation according to the hemodilution level using rotational thromboelastometry (ROTEM).
Methods
Venous blood was taken from 12 healthy volunteers and divided into four specimen tubes that were diluted to various levels (0%, 10%, 20%, and 40%) using an irrigation fluid composed of 2.7% sorbitol and 0.54% mannitol.
Results
Significant prolongation of clotting time was observed in the 40% diluted sample using both INTEM (P = 0.009) and EXTEM (P = 0.001) assays. However, the clot formation time was prolonged significantly in the 10%, 20%, and 40% diluted samples using both INTEM (P < 0.001) and EXTEM (P = 0.002, P < 0.001, and P < 0.001, respectively) assays. A significant decrease of α-angle of INTEM and EXTEM were observed in the 10% (P < 0.001), 20% (P < 0.001 and P = 0.001, respectively), and 40% (P < 0.001) groups compared with the 0% dilution group. The maximum clot firmness (MCF) of INTEM decreased significantly in the 20% (P < 0.001) and 40% (P < 0.001) diluted samples. In the MCF of EXTEM and FIBTEM assays, 10% (P = 0.009 and P = 0.015, respectively), 20% (P = 0.001), and 40% (P < 0.001) samples showed a significant decrease compared with the 0% sample. Nevertheless, most of the ROTEM values were within the reference range, except the 40% sample.
Postoperative hemorrhage has been shown to be a major complication of transurethral resection of the prostate (TURP) [1]. In particular, coagulopathy occurs when there is excessive absorption of irrigation fluid [2]. Serious postoperative hematuria, accompanied with hemorrhagic symptoms, has been reported, that may result from disseminated intravascular coagulopathy (DIC) [3]. Although hemostatic problems after TURP are common and implicated in the morbidity of the procedure [4,5], the mechanism regarding the effect of irrigation fluid absorption on coagulopathy remains unclear.
A previous clinical study found that absorption of irrigation fluid during TURP may impair the blood coagulation cascade, inhibiting the clotting factor activity or lowering the coagulation factor concentration through hemodilution [6]. However, in that study, the median irrigation fluid amount absorbed was only 406 ml that was certainly not enough to determine the effect of irrigation fluid absorption in large amounts. In general, adverse symptoms (i.e., nausea, vomiting, mental change, or DIC) are more common if irrigation fluids of 1 L to 2 L are absorbed, which occurs in 5% to 20% of the operations [7–10].
Rotational thromboelastometry (ROTEM; Tem International GmbH, Germany), which is known as a point-of-care tool, can detect the coagulation pathway derangement very rapidly, providing a comprehensive assessment of the patient’s hemostatic status [11–13]. To date, whether the conventional coagulation test, such as prothrombin time, can significantly and accurately reflect hypocoagulability remains unknown [14]. Moreover, prothrombin time and activated partial thromboplastin time reflect only limited parts of the coagulation system and do not provide information regarding the full coagulation pathway [15].
In this current study, under the hypothesis that greater absorption of irrigation fluid may cause more severe derangement in the coagulation cascade, we used ROTEM to investigate how blood coagulation changed based on the degree of hemodilution by an irrigation fluid composed of 2.7% sorbitol and 0.54% mannitol.
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (B-1703/386-303) and registered at ClinicalTrials.gov (NCT03105180). Written informed consent was obtained from 12 healthy volunteers who had no history of medications related to hemostasis, such as anti-coagulants, anti-platelets, or non-steroidal anti-inflammatory agents.
In total, 10 ml of fresh venous blood was obtained from an antecubital vein and immediately placed in citrate-containing polypropylene tubes (VacutainerⓇ, Becton Dickinson, UK). In order to reduce thromboplastin contamination, blood samples were collected using a two-syringe sampling technique. After securing the antecubital vein, an initial 5 ml of blood sample was aspirated and discarded. Thereafter, 10 ml of blood was drawn and put into 4 citrate-containing polypropylene tubes by 2 ml. The remained 2 ml of blood was discarded. One tube was used as a control (baseline). To crease 10%, 20%, and 40% dilution groups, 200, 400, and 800 μl of a fluid composed of 2.7% sorbitol and 0.54% mannitol (UrosolⓇ; CJ HealthCare, Korea) were added to the other three tubes, respectively, after discarding the same volume of blood. The individual mixing process was performed for about 10 min prior to the ROTEM analysis.
ROTEM analyses were performed by a single investigator in accordance with the manufacturer’s (TEM International GmbH, Germany) recommendations. We analyzed the following four ROTEM parameters: clotting time (CT), clot formation time (CFT), alpha (α)-angle, and maximum clot firmness (MCF). The intrinsically activated tests of ROTEM assays activated with phospholipid and ellagic acid (INTEM) and extrinsically activated tests of ROTEM assays activated with tissue factor (EXTEM) values – offering information regarding the intrinsic and extrinsic pathways, respectively – were assessed using in-TEMⓇ (0.2 M CaCl2 20 μl and thromboplastin-phospholipid 20 μl) and ex-TEMⓇ (0.2 M CaCl2 20 μl and tissue factor 20 μl) reagents, respectively. The change of fibrin polymerization was examined using an extrinsically activated tests of ROTEM assays activated with cytochalasin D followed by tissue factor (FIBTEM) test with fib-TEMⓇ reagent (0.2 M CaCl2 20 μl with cytochalasin D and tissue factor 20 μl).
Based on our previous works [16,17], as well as other published data [18], 12 volunteers were estimated to adequately power the study (80%) at the 5% significance level to detect 20% differences in MCF of FIBTEM from the control samples.
Data are expressed as the mean (SD). Repeated measures analysis of variance test was used to compare the baseline values with values after the dilution. Thereafter, to compare the differences among the dilution levels, paired t-test was used with Bonferroni correction. Due to multiple comparisons, a P value less than 0.017 (0.05/3) was considered statistically significant. Data were analyzed using SPSS for Windows software (ver. 22; IBM Corp., USA) or Sigma Plot 10.0 (Systat Software, Inc., USA).
In the present study, twelve healthy volunteers – six males and six females – were included (Table 1).
The following hypocoagulable pattern was observed with increased degree of hemodilution with respect to the ROTEM parameters (Table 2): an increase in CT and CFT, as well as a decrease in α-angle and MCF. Most of the ROTEM values were within the reference range, except the 40% dilution group.
Fig. 1 demonstrates the INTEM parameters in each dilution group. A significant prolongation of CT was observed in the 40% dilution group compared with the 0% dilution group (Fig. 1A, P = 0.009). CFT of INTEM showed a significant increase in the 10%, 20%, and 40% dilution groups compared with the 0% dilution group (Fig. 1B, P < 0.001). A significant decrease of α-angle of INTEM was observed in the 10%, 20%, and 40% dilution groups compared with the 0% dilution group (Fig. 1C, P < 0.001). MCF of INTEM decreased significantly in the 20% and 40% dilution groups compared with the 0% dilution (Fig. 1D, P < 0.001).
Fig. 2 demonstrates the EXTEM parameters in each dilution group. CT of EXTEM was prolonged significantly in the 40% dilution group compared with the 0% dilution group (Fig. 2A, P = 0.001). Significant increase of CFT of EXTEM was observed in the 10%, 20%, and 40% dilution groups compared with the 0% dilution group (Fig. 2B, P = 0.002, P < 0.001, and P < 0.001, respectively). A significant decrease of α-angle of EXTEM was observed in the 10%, 20%, and 40% groups compared with the 0% dilution group (Fig. 2C, P < 0.001, P = 0.001, and P < 0.001, respectively). In the MCF of EXTEM, the 10%, 20%, and 40% dilution groups showed a significant decrease compared with the 0% dilution group (Fig. 2D, P = 0.009, P = 0.001, and P < 0.001, respectively).
MCF of FIBTEM decreased significantly in the 10%, 20%, and 40% dilution groups compared with the 0% dilution group (Fig. 3, P = 0.015, P = 0.001, and P < 0.001, respectively).
In this study, we investigated the blood coagulation status according to the degree of hemodilution by an irrigation fluid composed of 2.7% sorbitol and 0.54% mannitol, and showed a hypocoagulable tendency in the overall ROTEM parameters, except CT of INTEM and EXTEM in 10% and 20% dilution groups.
There are three factors inherent in the operation that may promote coagulopathy in TURP: irrigation fluid absorption, dissemination of prostatic tissue substances, and excessive blood loss [19]. Özmen et al. [10] evaluated the correlation between the amount of irrigation fluid used and the prothrombin time; they concluded that most coagulation factors after TURP were reduced in proportion to the hemodilution by irrigation fluid. Our ROTEM results support their findings with convincing evidences of that coagulation status became hypocoagulable according to the hemodilution levels.
Interestingly, CFT, α-angle, and MCF values were more sensitively affected after hemodilution by a mixture of 2.7% sorbitol-0.54% mannitol fluid compared with the CT values. Each parameter represents a different coagulation step. CT indicates the beginning of clotting. Both CFT and α-angle indicate the initial rate of fibrin polymerization, and MCF indicate the maximal strength of a clot [20]. Although the initiation of clotting was not seriously impacted, the stabilization of the clot with fibrin polymerization seemed to be disturbed primarily following the hemodilution by an irrigation fluid composed of 2.7% sorbitol and 0.54% mannitol during endoscopic procedures. Therefore, careful attention to coagulopathy is required and monitoring of the function and level of fibrinogen is also necessary especially when a large amount of irrigation fluid absorption that is combined with surgical bleeding is suspected.
Based on the results of this in vitro study, there are several things to consider when using this irrigation fluid composed of 2.7% sorbitol and 0.54% mannitol in clinical practice. First, the amounts of absorbed irrigation fluid should be monitored during surgery to predict the potential coagulopathy. This is warranted because a high degree of hemodilution can cause greater coagulation impairment. It has previously been shown that during TURP, irrigation fluid is absorbed at a rate of 10 to 30 ml/min, and the average volume absorbed is 400–700 ml during hysteroscopic transcervical resection of the endometrium (TCRE) [8,21,22]. In the present study, although hypocoagulable change was observed in the 20% hemodilution group, each value of ROTEM parameter was within the normal reference range. Conversely, 40% dilution caused profound coagulation impairment, which is beyond the normal range. Absorption of large amount of irrigation fluid (> 1 to 2 L) occurs in approximately 9% of patients undergoing TCRE and in about 20% of patients undergoing TURP [8]. Therefore, if the irrigation fluid volume absorbed is greater than the known average amount, blood coagulation status should be checked. Second, the amount of absorbed irrigation fluid has previously been shown to be associated with surgery time [23,24]. Therefore, a longer operation time may hinder the coagulation cascade as a result of absorbing large amounts of irrigation fluid. Furthermore, intraoperative hemorrhage has been established to accompany the consumption of coagulation factors [25], thus, the combination of intraoperative hemorrhage and the absorption of irrigation fluid may worsen coagulopathy, especially with long operation time. For this reason, surgery time should also be monitored carefully. The final consideration is the technique of tissue resection. A monopolar or bipolar resection method has been used to resect prostatic or endometrial tissue. An introduction of bipolar resection to clinical practice enabled surgeons to work with isotonic saline as an irrigation fluid and low-voltage current. Hemodilution via isotonic saline administration has been known to cause hypercoagulable change in the coagulation cascade [26]. Bipolar resection, via the use of isotonic saline as the irrigation fluid, seems to be a better technique when compared with monopolar resection, considering the effect of irrigation fluid on the blood coagulation and the technical advantage of bipolar resection in reducing blood loss [27]. However, further study is needed to investigate an association between the occurrence of coagulopathy and the type of prostate resection in a clinical setting.
There are several limitations to this present study. First, because this study was performed in an in vitro setting, it may have little clinical relevance. The strength of an in vitro study is controllability and reproducibility. In this study, the dilution range was controlled to maximize clinical applicability, enabling the evaluation of the potential risk for coagulation disturbance associated with irrigation fluid. Further studies should be conducted to better determine the absorbed volume of irrigation fluid that causes clinical coagulation abnormality. Second, the study population consisted of mostly young adults. To extend our findings to the general population, further studies will be required aimed at clarifying the role of age on the effect of irrigation fluid with respect to the blood coagulation pathway. Finally, 40% hemodilution may be a rare case in clinical practice. However, with ongoing surgical bleeding and long operation time, severe hemodilution via absorption of irrigation fluid can occur, requiring close monitoring of coagulopathy.
In conclusion, this in vitro study showed that blood became hypocoagulable when it was diluted with a fluid composed of 2.7% sorbitol and 0.54% mannitol. There seems to be a disturbance of clot stabilization with fibrin polymerization rather than an initiation of clotting in the coagulation pathway.
Fig. 1.
INTEM parameters in each dilution group: (A) CT, (B) CFT, (C) α-angle, and (D) MCF; 0% (black), 10% (grey), 20% (dark grey), and 40% (pale grey) diluted groups using a fluid composed of 2.7% sorbitol and 0.54% mannitol. Values are mean (SD). CT: clotting time (s), CFT: clot formation time (s), α-angle (°), MCF: maximum clot firmness (mm). The short dash lines refer to the reference range. *Significant differences from 0% diluted group (P < 0.017).
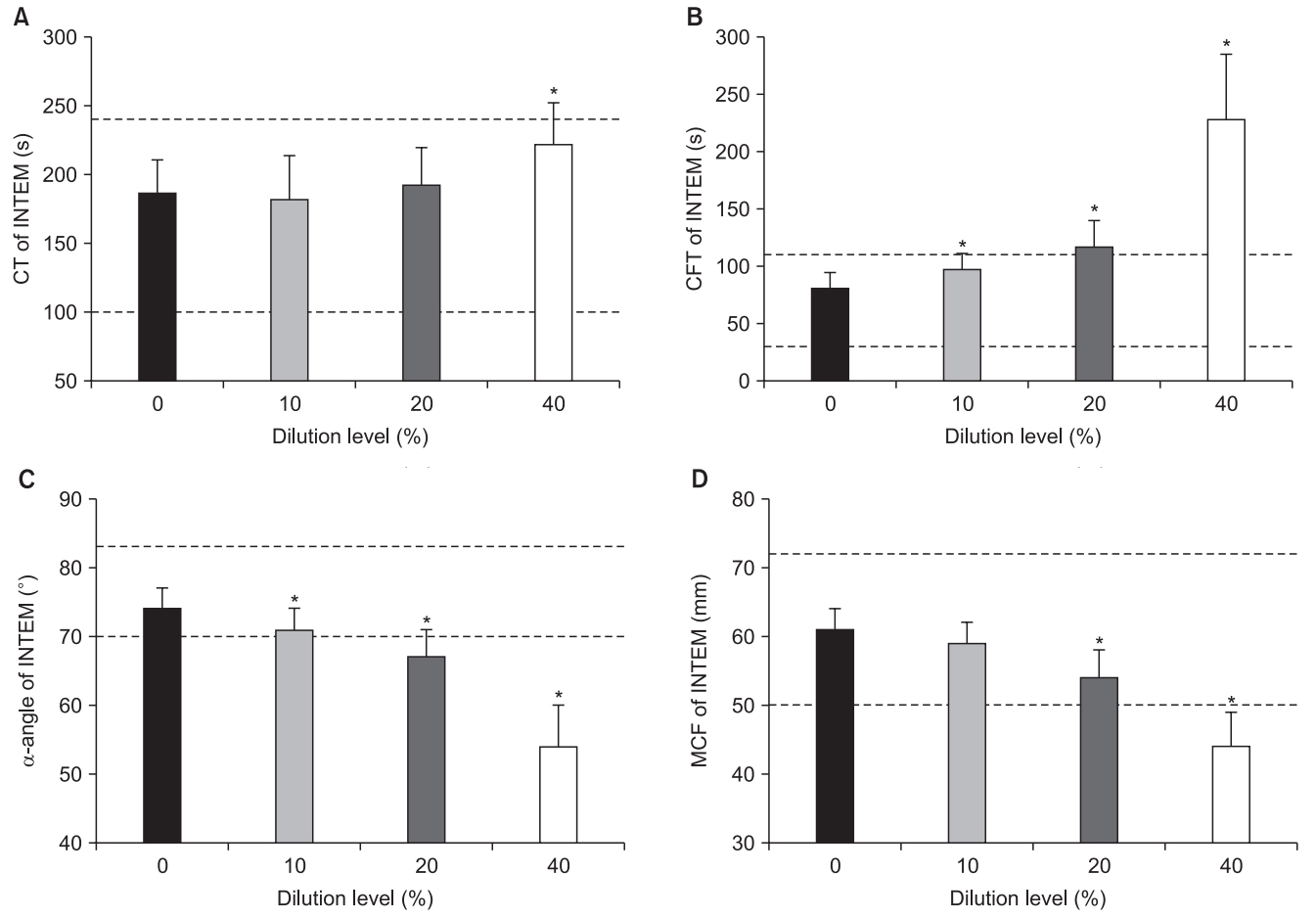
Fig. 2.
EXTEM parameters in each dilution group: (A) CT, (B) CFT, (C) α-angle, and (D) MCF; 0% (black), 10% (grey), 20% (dark grey), and 40% (pale grey) diluted groups using a fluid composed of 2.7% sorbitol and 0.54% mannitol. Values are mean (SD). CT: clotting time (s), CFT: clot formation time (s), α-angle (°), MCF: maximum clot firmness (mm). The short dash lines refer to the reference range. *Significant differences from 0% diluted group (P < 0.017).
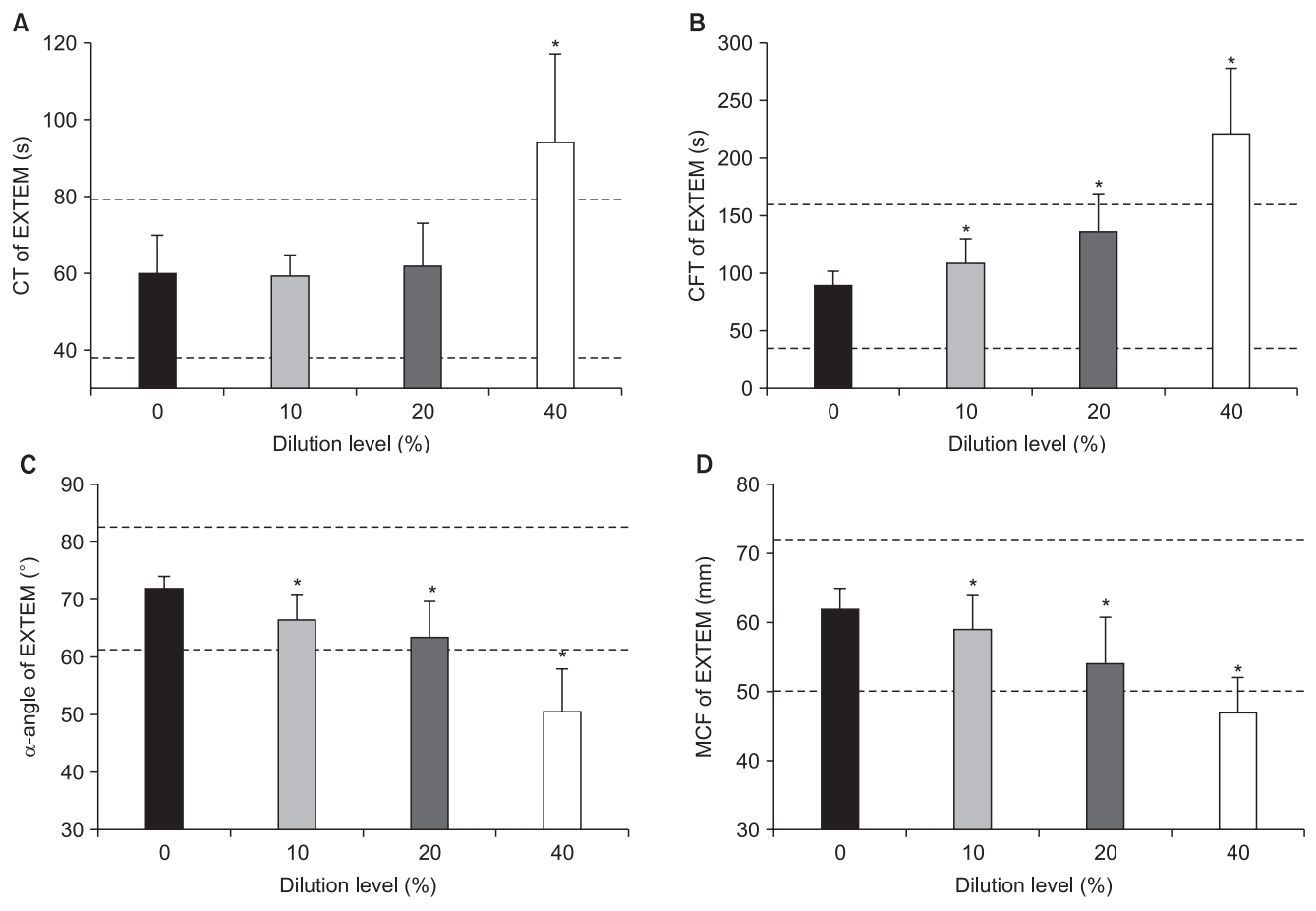
Fig. 3.
MCF of FIBTEM in each dilution group: 0% (black), 10% (grey), 20% (dark grey), and 40% (pale grey) diluted groups using a fluid composed of 2.7% sorbitol and 0.54% mannitol. Values are mean (SD). MCF: maximum clot firmness (mm). The short dash lines refer to the reference range. *Significant differences from 0% diluted group (P < 0.017).
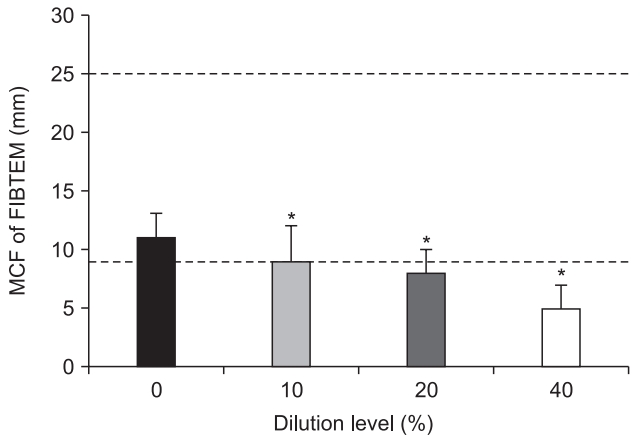
Table 1.
Characteristics of Patients (n = 12)
| Gender (M/F) | 6/6 |
| Age (yr) | 32 ± 4 |
| Height (cm) | 168 ± 8 |
| Weight (kg) | 59 ± 12 |
| BMI (kg/cm2) | 21 ± 3 |
Table 2.
Changes in ROTEM Parameters according to the Hemodilution
| Reference range |
Dilution level |
|||||
|---|---|---|---|---|---|---|
| 0% | 10% | 20% | 40% | P value | ||
| INTEM | ||||||
| CT (s) | 100–240 | 186 ± 24 | 181 ± 32 | 192 ± 27 | 221 ± 31* | 0.003 |
| CFT (s) | 30–110 | 81 ± 14 | 98 ± 13* | 117 ± 23* | 228 ± 57* | < 0.001 |
| α (°) | 70–83 | 74 ± 3 | 71 ± 3* | 67 ± 4* | 54 ± 6* | < 0.001 |
| MCF (mm) | 50–72 | 61 ± 3 | 59 ± 3 | 54 ± 4* | 44 ± 5* | < 0.001 |
| EXTEM | ||||||
| CT (s) | 38–79 | 60 ± 10 | 59 ± 6 | 62 ± 11 | 94 ± 23* | < 0.001 |
| CFT (s) | 34–159 | 90 ± 12 | 109 ± 21* | 137 ± 32* | 221 ± 57* | < 0.001 |
| α (°) | 63–83 | 73 ± 2 | 68 ± 4* | 65 ± 6* | 53 ± 7* | < 0.001 |
| MCF (mm) | 50–72 | 62 ± 3 | 59 ± 5* | 55 ± 6* | 47 ± 5* | < 0.001 |
| FIBTEM | ||||||
| MCF (mm) | 9–25 | 11 ± 2 | 9 ± 3* | 8 ± 2* | 5 ± 2* | < 0.001 |
Values are presented as mean ± SD. ROTEM: rotational thromboelastometry, INTEM: intrinsically activated test of ROTEM assays (activation with phospholipid and ellagic acid), EXTEM: extrinsically activated tests of ROTEM assays (activation with tissue factor), FIBTEM: extrinsically activated tests of ROTEM assays (activation with cytochalasin D followed by tissue factor), CT: clotting time, CFT: clot formation time, α: alpha-angle, MCF: maximum clot firmness.
References
1. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol 2006; 50: 969-79.


2. Ekengren J, Hahn RG. Blood loss during transurethral resection of the prostate as measured by the HemoCue photometer. Scand J Urol Nephrol 1993; 27: 501-7.


3. Friedman NJ, Hoag MS, Robinson AJ, Aggeler PM. Hemorrhagic syndrome following transurethral prostatic resection for benign adenoma. Arch Intern Med 1969; 124: 341-9.


4. Doll HA, Black NA, McPherson K, Flood AB, Williams GB, Smith JC. Mortality, morbidity and complications following transurethral resection of the prostate for benign prostatic hypertrophy. J Urol 1992; 147: 1566-73.


5. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol 1989; 141: 243-7.


6. Shin HJ, Na HS, Jeon YT, Park HP, Nam SW, Hwang JW. The impact of irrigating fluid absorption on blood coagulation in patients undergoing transurethral resection of the prostate: a prospective observational study using rotational thromboelastometry. Medicine (Baltimore) 2017; 96: e5468.



7. Olsson J, Nilsson A, Hahn RG. Symptoms of the transurethral resection syndrome using glycine as the irrigant. J Urol 1995; 154: 123-8.


9. Hahn RG. Fluid absorption and the ethanol monitoring method. Acta Anaesthesiol Scand 2015; 59: 1081-93.


10. Ozmen S, Koşar A, Sayin A, Aydin C, Yavuz L. Effect of transurethral resection of the prostate on blood coagulation test results. Urol Int 2003; 70: 27-30.


11. Kashuk JL, Moore EE, Sawyer M, Le T, Johnson J, Biffl WL, et al. Postinjury coagulopathy management: goal directed resuscitation via POC thrombelastography. Ann Surg 2010; 251: 604-14.


12. Johansson PI, Stensballe J. Effect of Haemostatic Control Resuscitation on mortality in massively bleeding patients: a before and after study. Vox Sang 2009; 96: 111-8.


13. Carroll RC, Craft RM, Langdon RJ, Clanton CR, Snider CC, Wellons DD, et al. Early evaluation of acute traumatic coagulopathy by thrombelastography. Transl Res 2009; 154: 34-9.


15. Müller MC, Meijers JC, Vroom MB, Juffermans NP. Utility of thromboelastography and/or thromboelastometry in adults with sepsis: a systematic review. Crit Care 2014; 18: R30.



16. Shin HJ, Na HS, Lee S, Lee GW, Do SH. The effect of hyperglycemia on blood coagulation: In vitro, observational healthy-volunteer study using rotational thromboelastometry (ROTEM). Medicine (Baltimore) 2016; 95: e4703.



17. Shin HJ, Park HY, Na HS, Hong JP, Lee GW, Do SH. The effects of Plasma-Lyte 148 solution on blood coagulation: an in-vitro, volunteer study using rotational thromboelastometry. Blood Coagul Fibrinolysis 2018; 29: 446-50.



18. Roche AM, James MF, Bennett-Guerrero E, Mythen MG. A head-to-head comparison of the in vitro coagulation effects of saline-based and balanced electrolyte crystalloid and colloid intravenous fluids. Anesth Analg 2006; 102: 1274-9.


19. Hahn RG, Berlin T, Lewenhaupt A. Factors influencing the osmolality and the concentrations of blood haemoglobin and electrolytes during transurethral resection of the prostate. Acta Anaesthesiol Scand 1987; 31: 601-7.


20. Whiting D, DiNardo JA. TEG and ROTEM: technology and clinical applications. Am J Hematol 2014; 89: 228-32.


21. Bergeron ME, Ouellet P, Bujold E, Cote M, Rhéaume C, Lapointe D, et al. The impact of anesthesia on glycine absorption in operative hysteroscopy: a randomized controlled trial. Anesth Analg 2011; 113: 723-8.


22. Gravenstein D. Transurethral resection of the prostate (TURP) syndrome: a review of the pathophysiology and management. Anesth Analg 1997; 84: 438-46.


23. Estes CM, Maye JP. Severe intraoperative hyponatremia in a patient scheduled for elective hysteroscopy: a case report. AANA J 2003; 71: 203-5.

24. Molnar BG, Magos AL, Kay J. Monitoring fluid absorption using 1% ethanol-tagged glycine during operative hysteroscopy. J Am Assoc Gynecol Laparosc 1997; 4: 357-62.


25. Ghadimi K, Levy JH, Welsby IJ. Perioperative management of the bleeding patient. Br J Anaesth 2016; 117(suppl 3): iii18-30.













