The effect of sugammadex on the vascular tone of isolated rat aorta
Article information
The γ-cyclodextrin, sugammadex, produces a rapid reversal of the neuromuscular blockade induced by the nondepolarizing agents rocuronium and vecuronium via encapsulation, leading to rapid recovery from muscle relaxants used in surgery. It has been reported that intravenous administration of sugammadex rarely causes hypotension induced by anaphylaxis and hypersensitivity reactions [1,2]. As histamine, released from mast cells and basophils activated by anaphylaxis or type I hypersensitivity reactions causes vasodilation, which seems to contribute to sugammadex-induced hypotension observed in previous reports via the indirect mechanism [3]. Conversely, sugammadex may produce coronary vasospasm in variant angina, which leads to cardiac arrest [4]. However, the direct effect of sugammadex on vasoreactivity (vascular tone) remains unknown. Thus, we investigated the direct effect of sugammadex on the contraction induced by the contractile agonist, norepinephrine released from sympathetic nerve endings, and by the voltage-operated calcium channel activator, KCl, using isometric tension measurements of isolated rat aorta, as described previously [5]. We obtained approval for this experimental protocol from the Animal Care and Use Committee of Gyeongsang National University. After 60 mM KCl or norepinephrine (10−6 M) produced a sustained and stable contraction in isolated endothelium-intact and endothelium-denuded rat aortas, sugammadex (10−6 to 3 × 10−4 M) was cumulatively added to the organ bath to produce sugammadex dose-response curves. Sugammadex (10−6 to 3 × 10−4 M) had no effect on the contraction induced by norepinephrine (10−6 M, Fig. 1A and 1B) or 60 mM KCl (Fig. 1C and 1D) in the isolated endothelium-intact and -denuded rat aortas. The results suggest that sugammadex itself, in a dose that exceeds the clinical dose of sugammadex (10−5 M), has no direct effect on voltageor receptor-operated calcium channels or endothelium-derived vasodilators, including nitric oxide, which contribute to vascular tone modulation. However, the present study has the following limitations. First, as protein kinase C and Rho-kinase in vascular smooth muscle are involved in vasoconstriction mediated by calcium sensitization, further study regarding the effect of sugammadex on the contraction induced by the protein kinase C stimulant phorbol 12,13-dibutyrate or the Rho-kinase stimulant NaF is needed. Second, small resistance arterioles such as the mesenteric artery rather than the aorta as a conduit vessel are mainly involved in the regulation of peripheral vascular resistance. In spite of these limitations, the results of the present study, when taken together, suggest that sugammadex has no direct effect on the vascular tone of isolated vessels.
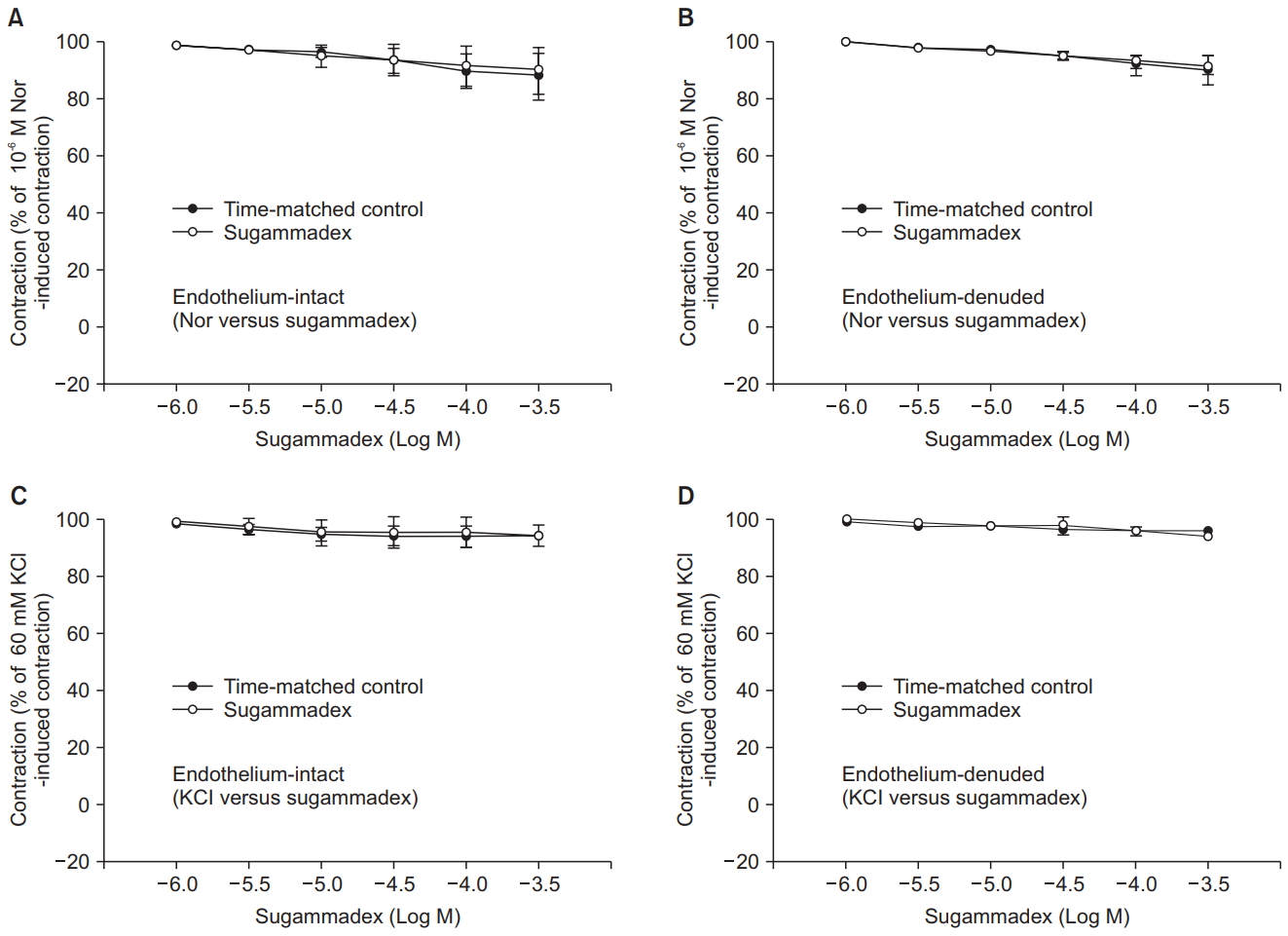
Effect of sugammadex on the contractions induced by norepinephrine (Nor) or KCl in isolated endothelium-intact rat aortas (Nor: N = 7; KCl: N = 8) and -denuded (Nor: N = 7; KCl: N = 6). Data are shown as mean ± standard deviation (SD) and are expressed as the percentage of contraction induced by norepinephrine or KCl. N indicates the number of isolated rat aortic rings.
Notes
Funding Statement
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2016R1D1A1B03930451).
