|
 |
|
|
Abstract
General anesthesia is the main strategy for almost all thoracic surgeries. However, a growing body of literature has reported successful cases of non-intubated thoracic surgery with regional anesthesia. This alternative strategy not only prevents complications related to general anesthesia, such as lung injury, incomplete re-expansion and intubation related problems, but also accords with trends of shorter hospital stay and lower overall costs. We experienced a successful case of non-intubated thoracoscopic decortication for a 68-year-old man who was diagnosed as empyema while the patient kept spontaneously breathing with moderate sedation under thoracic epidural anesthesia. The patient showed a fast recovery without concerns of general anesthesia related complications and effective postoperative analgesia through thoracic epidural patient-controlled analgesia device. This is the first report of non-intubated thoracoscopic surgery under thoracic epidural anesthesia in Korea, and we expect that various well designed prospective studies will warrant the improvement of outcomes in non-intubated thoracoscopic surgery.
In the past, thoracic surgery was widely performed to treat gunshot wounds in World War I without general anesthesia (GA), and it formed the basis of developing understanding of thoracic operations [1]. As the double-lumen tube was developed, one-lung ventilation with GA became the main strategy for thoracic surgery compared to use of regional anesthesia technique. However, this strategy revealed impaired cardiac function and adverse effects related to ventilator associated lung injury, such as barotrauma, volutrauma, and atelectrauma [2]. Moreover, as there has been a significant improvement in minimally invasive thoracic surgery in the last 2 decades, increasing reports began to report successful cases of non-intubated thoracic surgery with regional anesthesia.
We report a successful case of non-intubated video-assisted thoracoscopic surgery (VATS) for decortication of empyema under thoracic epidural anesthesia (TEA) in a patient with poor respiratory performance. Despite a high risk of postoperative deterioration of respiratory function, the patient showed a fast recovery without complications and postoperative pain was effectively controlled via a thoracic epidural patient-controlled analgesia (PCA) device. This is the first reported case in the literature, even though non-intubated thoracoscopic surgery has been increasingly performed in certain conditions in Korea.
A 68-year-old male patient (height: 160 cm, weight: 38 kg) visited our hospital, presenting with a cough, sputum and pain in the right side of the chest, arising 2 weeks ago. The patient had no history of chronic disease.
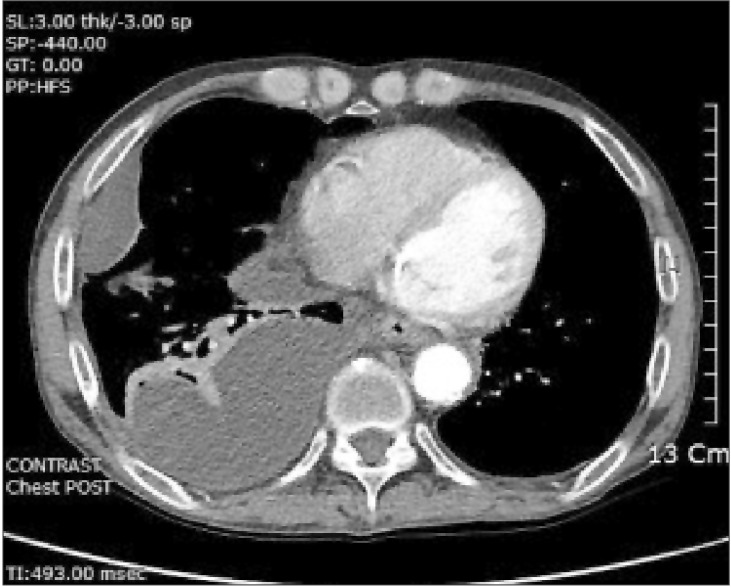
The chest computed tomography (CT) indicated a large amount of unilateral loculated effusion in the right lower lung (Fig. 1). The patient's preoperative diagnosis was empyema with parapneumonic effusion. The results of the pulmonary function test (PFT) showed a severe obstructive pattern: the forced expiratory volume in 1 second was 37% and the ratio of forced expiratory volume in 1 second to forced vital capacity was 45%. The patient was newly diagnosed as chronic obstructive pulmonary disease and the peripheral oxygen saturation was maintained at 96% with 2 L/min of oxygen by nasal prong.
At first, the patient was referred to the department of radiology for the insertion of percutaneous drainage catheter. However, catheter insertion failed due to severe loculation. Therefore, decortication under VATS was scheduled. Considering the patient's impaired pulmonary performance, we decided to employ the TEA technique with monitored anesthesia care, keeping the patient sedated with spontaneous ventilation throughout the operation.
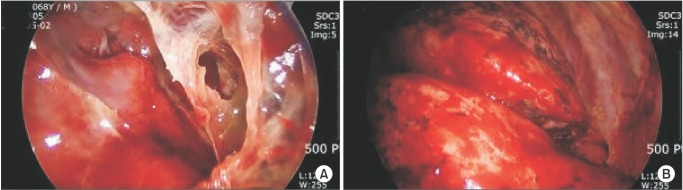
On arriving at the operating room, the patient was monitored by noninvasive blood pressure, electrocardiography, pulse oximetry, and bispectral index (BIS). Invasive arterial blood pressure was set for arterial blood gas and real-time hemodynamic status monitoring. While performing thoracic epidural catheter insertion by the paramedian approach at the T4-5 interspace, the patient was sedated by administration of dexmedetomidine at loading dose of 0.8 µg/kg for 10 min, followed by a maintenance infusion at 0.4 µg/kg/h with high flow nasal cannula oxygen therapy at a flow rate of 30 L/min (FiO of 0.4). After the injection of 14 ml of 0.375% ropivacaine through an epidural catheter, the extent of sensory block was confirmed to be over T3 to T9 dermatomes. Prior to the beginning of VATS, the administration of intravenous propofol and remifentanil was additionally started via target controlled infusion for stable sedation and to prepare against an incomplete block, titrated to maintain a BIS score of 50 to 70 throughout the surgery. Once either hemithorax was opened by inserting two 12 mm trocars in the 7th intercostal space at midaxillary line and the 8th intercostal space at posterior axillary line on the right lung, the nondependent lung was collapsed gradually. Although paradoxical respiration and mediastinal shift might induce inefficient tidal volume and hemodynamic instability, the patient did not show cardiac compromise or significant respiratory derangement. He maintained 95–98% of SpO2 with respiratory rate of 15–20 breaths/min. Then, the surgeon instillated 3 ml of 0.25% bupivacaine for the vagus nerve block to minimize visceral sensation and suppress cough reflex. The surgeon identified pleural peel covering the parietal pleura and atelectatic lung (Fig. 2A), and then removed the pleural fluid and debris covering the base of basal segment and perforated abscess cavity in the posterior basal segment, as a result, a completely expanded lung could be confirmed (Fig. 2B). An intraoperative arterial blood gas analysis showed the following: pH 7.308, PaCO2 37.6 mmHg, PaO2 119.9 mmHg, and SaO2 97.6%. His vital signs were stable. The total operating time was 80 min. After complete wound closure, the patient was woken, then asked to cough and breathe deeply so that the collapsed lung was effectively re-expanded.
Postoperative pain was effectively controlled by thoracic epidural PCA device: provided at 6 ml/h of 0.15% ropivacaine with 3.5 µg/ml fentanyl. That enabled a visual analogue score (VAS) of around 1 or 2. The patient was fully recovered in 2 weeks without any complications.
Conventionally, GA with mechanical one-lung ventilation was the main anesthetic choice for thoracic surgery; however, patients have been at risk of numerous postoperative complications, such as lung injury, incomplete re-expansion and intubation related problems. As minimally invasive thoracic surgery has been significantly improved in the last 2 decades, increasing the body of research reported successful cases of non-intubated thoracic surgery with regional anesthesia while the patient is being woken or sedated.
GA with one-lung ventilation has potential complications, which increase mortality and morbidity. Mechanical ventilation itself can cause lung injury, which makes the related area undergo inflammatory change progressing to interstitial edema, restricted lung compliance, ventilation-to-perfusion mismatch and loss of surfactant [3]. In addition, mechanical one-lung ventilation induces ventilation-to-perfusion mismatch at the dependent lung, which leads to a hypoxic state sufficient to cause tissue acidosis, alveolar edema, vascular congestion and cytokine release [4]. The rationale for regional anesthesia for thoracic surgery is that patients can escape from these kinds of complications of GA with one-lung ventilation, which leads to a lower morbidity and faster recovery.
Numerous types of thoracic procedures can be carried out under regional anesthesia, ranging from drainage of pleural effusion, pleurodesis, or decortication to wedge resection, lobectomy, tracheal resection or excision of mediastinal mass [5]. It is known that regional anesthesia provides better hemodynamic stability, less thrombotic complications, and reduced surgical stress response compared to GA [6]. For non-intubated thoracic surgeries, patients should be carefully selected and excluded in case having following contraindications, which overlap with exclusion criteria of regional anesthesia; hemodynamically unstable patients, INR > 1.5 or current antiplatelet therapy, sleep apnea, unfavorable airway or spinal deformity, previous ipsilateral thoracic surgery, asthma, extreme obesity (body mass index > 35 kg/m2), preoperative decompensated heart disease, several pleural adhesion over targeted hemithorax, intracranial hypertension, patient unable to cooperate with the procedure, and so on [7,8]. In addition, caution must be taken with regard to complications related to regional anesthesia, which occurs rarely but can be potential, such as epidural hematoma, spinal cord injury, and inadvertent high anesthetic level.
In our case, the patient's PFT revealed impairment in pulmonary function, it was expected that he would be at a higher risk of postoperative respiratory complications related to one-lung ventilation of GA. Additionally, as the patient had not any contraindications for employing non-intubated VATS, he was the optimal candidate of non-intubated thoracic surgery for escaping from possible complications of one-lung ventilation with GA. In any patient's condition, we should determine surgical and anesthetic techniques by considering the risk benefit ratio in conventional one-lung ventilation under GA or non-intubated thoracic surgery under regional anesthesia.
Regional anesthesia for non-intubated thoracic surgery has various approaches including intercostal nerve block, paravertebral nerve block, TEA and intrapleural analgesia [9]. TEA itself provides a sufficient analgesic effect covering the chest wall and pleural cavity, therefore it is known to be suitable for most thoracic surgeries. Additional ipsilateral stellate ganglion block and intrathoracic vagus nerve block can abolish coughing reflex triggered by surgical manipulation. Remifentanil infusion also helps to blunt the possible cough reflex. We performed TEA with intravenous remifentanil administration in addition to a vagus nerve block, which resulted in providing a suitable anesthesia level for the surgery without a harmful cough reflex throughout the entire procedure. Moreover, PCA using a thoracic epidural catheter effectively controlled postoperative pain, resulting in the VAS of the patient remaining at 1 or 2. Given that TEA can provide superior postoperative analgesia, as well as intraoperative analgesia, it has reasonable advantages over GA.
For non-intubated thoracic surgery, the surgeon and the anesthesiologist team must work closely, cooperating and communicating with each other through the entire procedure. Inexperienced and poorly cooperative surgical teams may confront with a difficulty in performing the non-intubated anesthesia of thoracic surgery. Based on previous literature findings, the overall conversion rate to GA ranges from < 1% to 9% [10]. The most common causes of conversion are surgical difficulties, such as strong adhesions, major bleeding, and significant mediastinal movement. Non-surgical causes include suboptimal analgesia, persistent hypoxemia, and tachypnea. For early conversion to intubated GA, anesthesiologist team should always be ready to proceed to rapid orotracheal intubation which is technically challenging for the anesthesiologist at patient's lateral decubitus position [11,12]. While surgical openings are rapidly covered with transparent drape with chest tube insertion to avoid lung collapse, the anesthesiologist should assist patient's ventilation with high flow 100% oxygen. It is recommended to insert a single-lumen endotracheal tube under bronchoscopic guidance followed by inserting a bronchial blocker without changing the patient's position. It has been reported that a skilled anesthesiologist can conduct a double-lumen intubation in the lateral decubitus position [13]. If one-lung ventilation is not inevitable to complete the operation, a single lumen tracheal tube or supraglottic devices will be useful for mechanical ventilation. Preoperative positioning of additional bed sheet under the back of the patient on the operating table can be used to rapidly change the patient from lateral position to supine position.
In conclusion, we have presented that TEA with moderate sedation could be a feasible strategy for thoracoscopic surgery in patients with complicated respiratory function. Regional anesthesia strategy certainly reduced the length of hospital stay, overall costs and morbidity rates in selected cohorts, even if several biases existed [14]. In recent years, studies regarding the advantage of non-intubated thoracoscopic surgery have been based on observational or retrospective case series to date. We expect that the available data will substantially increase and evidence-based detailed protocols will be developed in the foreseeable future as the growing numbers of clinicians become aware that regional anesthesia can be an alternative strategy for thoracic surgery, which will allow us to improve outcomes in carefully selected patients.
References
2. Mineo TC, Pompeo E, Mineo D, Tacconi F, Marino M, Sabato AF. Awake nonresectional lung volume reduction surgery. Ann Surg 2006; 243: 131-136. PMID: 16371748.



3. Pavone LA, Albert S, Carney D, Gatto LA, Halter JM, Nieman GF. Injurious mechanical ventilation in the normal lung causes a progressive pathologic change in dynamic alveolar mechanics. Crit Care 2007; 11: R64PMID: 17565688.



4. Schilling T, Kozian A, Huth C, Bühling F, Kretzschmar M, Welte T, et al. The pulmonary immune effects of mechanical ventilation in patients undergoing thoracic surgery. Anesth Analg 2005; 101: 957-965. PMID: 16192502.


5. Kiss G, Castillo M. Nonintubated anesthesia in thoracic surgery: general issues. Ann Transl Med 2015; 3: 110PMID: 26046051.


6. Piccioni F, Langer M, Fumagalli L, Haeusler E, Conti B, Previtali P. Thoracic paravertebral anaesthesia for awake video-assisted thoracoscopic surgery daily. Anaesthesia 2010; 65: 1221-1224. PMID: 20569246.


7. Hung MH, Hsu HH, Cheng YJ, Chen JS. Nonintubated thoracoscopic surgery: state of the art and future directions. J Thorac Dis 2014; 6: 2-9. PMID: 24455169.


8. Chen JS, Cheng YJ, Hung MH, Tseng YD, Chen KC, Lee YC. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011; 254: 1038-1043. PMID: 21869676.


9. Yang JT, Hung MH, Chen JS, Cheng YJ. Anesthetic consideration for nonintubated VATS. J Thorac Dis 2014; 6: 10-13. PMID: 24455170.


10. Mineo TC, Tacconi F. From “awake” to “monitored anesthesia care” thoracic surgery: A 15 year evolution. Thorac Cancer 2014; 5: 1-13. PMID: 26766966.



11. Nakanishi R, Yasuda M. Awake thoracoscopic surgery under epidural anesthesia: is it really safe? Chin J Cancer Res 2014; 26: 368-370. PMID: 25232207.


12. Mineo TC, Tacconi F. Nonintubated thoracic surgery: a lead role or just a walk on part? Chin J Cancer Res 2014; 26: 507-510. PMID: 25400414.


13. Gonzalez-Rivas D, Fernandez R, de la, Rodriguez JL, Fontan L, Molina F. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014; 19: 552-555. PMID: 25006214.



14. Tacconi F, Pompeo E. Non-intubated video-assisted thoracic surgery: where does evidence stand? J Thorac Dis 2016; 8(Suppl 4): S364-S375. PMID: 27195134.