Subclavian venous catheterization remains the most commonly used blind approach due to consistent landmarks, increased patient comfort, and lower potential for infection or arterial injury compared with femoral catheterization [1]. However, it may cause various complications. We present a case in which transient hemidiaphragmatic paralysis occurred after right subclavian venous catheterization and propose a mechanism that may have led to this adverse effect.
Case Report
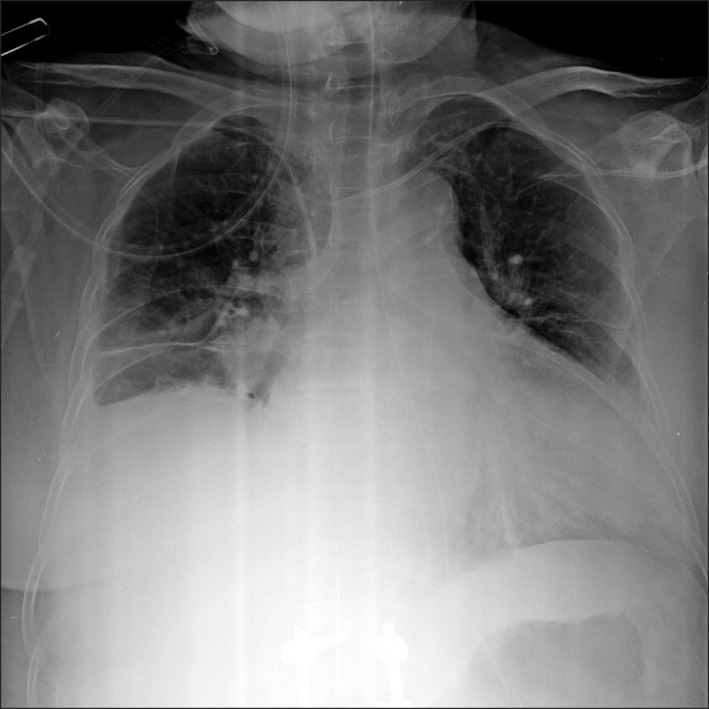
Written informed consent and agreement for publication were obtained from the patient. A 73-year-old woman (height 153 cm, weight 56 kg, ASA II) was admitted to our hospital as an emergency because of acute perforation of the small bowel with hemoperitoneum. The patient's prior medical history was unremarkable. The preoperative chest x-ray was normal (Fig. 1). On emergency department admission, preoperative insertion of a central venous catheter was planned for the purpose of emergency volume resuscitation. A 7 Fr. catheter (ARROWgard Blue®; Arrow International Inc., Pennsylvania, USA) was passed into the right subclavian vein through an infraclavicular approach at the first attempt. Blood returned freely through the catheter. The chest x-ray confirmed the proper placement of the catheter, but it also showed an elevation of the right hemidiaphragm. The medical team did not notice this finding. The patient underwent segmental resection of small bowel with mesenteric repair. The operation was uneventful. The patient was transferred to the intensive care unit.
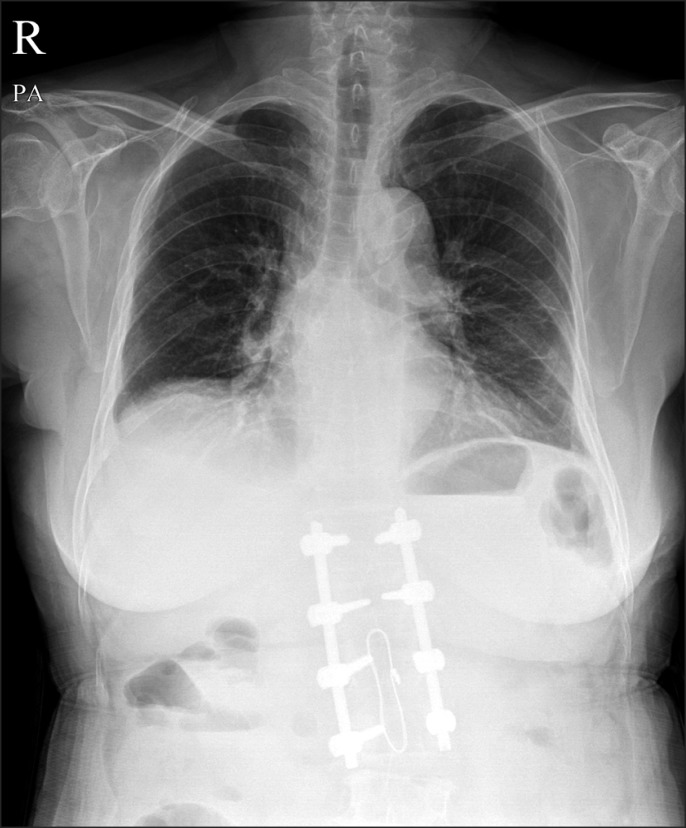
On the third postoperative day, an anesthesiologist incidentally noted in a chest x-ray the elevation of the right hemidiaphragm with a small effusion (Fig. 2). The patient did not complain of any dyspnea and the arterial blood gas data were normal. Ultrasound evaluation of both diaphragms with a low-frequency curvilinear probe as previously described [2] demonstrated a decreased motion of the right diaphragm compared with that of the left diaphragm. In M mode settings, left and right diaphragm excursion were 2.08/4.32 cm and 0.87/1.97 cm during quiet and deep breathing, respectively. There were no subphrenic or hepatic mass lesions.
On the fourth postoperative day, the patient was transferred to another university hospital for further treatment of the injuries. On admission, the right subclavian catheter was removed. On follow-up, a chest x-ray after the withdrawal showed the right hemidiaphragm had returned to normal (Fig. 3). Any other therapeutic intervention was not performed. The postoperative recovery was uneventful.
Discussion
Phrenic nerve paralysis following central venous catheterization is a rare complication and is not well recognized. There have been several case reports describing phrenic nerve paralysis following central venous catheterization, in which a number of mechanisms have been proposed. The mechanisms include direct nerve injury as a result of repeated attempts at venipuncture [3], compression by hematoma produced by an inadvertent arterial puncture during catheterization [4], lidocaine instillation during the procedure [5], venous wall inflammation in association with long-standing indwelling catheter [6], and rigid catheter impinging upon the thin venous wall and compressing the phrenic nerve [7].
In our case, phrenic nerve paralysis occurred immediately following right subclavian catherization and resolved completely after catheter removal. This suggests a reversible paralysis resulting from nerve compression rather than direct nerve injury to the phrenic nerve, which may cause irreversible paralysis. It is also unlikely that compression of the phrenic nerve by hematoma caused the hemidiaphragmatic paresis, because the central venous catheter was successfully placed at the first attempt. We hypothesize that an anatomical variation of the phrenic nerve was responsible for transient hemidiaphragmatic paralysis.
The phrenic nerve arises chiefly from the fourth cervical ventral ramus with occasional contributions from the third and fifth rami. It is formed at the upper part of the lateral border of the scalenus anterior muscle and descends almost vertically across its anterior surface behind the prevertebral fascia. At the root of the neck, it ordinarily runs anterior to the suclavian artery and posterior to the subclavian vein to enter the thorax. However, Paraskevas et al. [8] reported that the phrenic nerve crossed anterior to the subclavian vein 0.3-0.5 cm lateral to the jugulo-subclavian junction or traversed the anterior wall of the subclavian vein, just 1.4 cm lateral to the jugulo-subclavian junction. In addition, the accessory phrenic nerve may contribute to this complication. Codesido and Querri-Guttenburg [9] reported a case of accessory phrenic nerve passing through an annulus of the subclavian vein located 1 cm from the jugulo-subclavian junction. Similarly, Talbot [10] reported in one specimen the presence of an accessory phrenic nerve passing through the subclavian vein and dividing it into two channels. Therefore, the phrenic nerve (or accessory phrenic nerve) can be directly compressed by a rigid catheter near the jugulo-subclavian junction following catheterization, as postulated in our case. Both the successful catheterization at the first attempt and complete recovery of hemidiaphragm after catheter removal support this postulation. Paraskevas et al. [8] recommended that the puncture site should be more lateral to the outmost portion of the subclavian vein to minimize the risk of nerve impairment.
In summary, transient hemidiaphragmatic paralysis after subclavian venous catheterization can also be attributed to the anatomical variations of the phrenic nerve. Therefore, it is important to have a thorough knowledge of the relevant anatomy and anatomical variations to perform a central venous catheterization safely and efficiently.