Pretreatment of magnesium sulphate improves intubating conditions of rapid sequence tracheal intubation using alfentanil, propofol, and rocuronium - a randomized trial
Article information
Abstract
Background
We investigated the effects of a magnesium sulfate pretreatment on intubating conditions and cardiovascular responses during rapid sequence tracheal intubation (RSI) in this double-blind randomized study.
Methods
Adult patients (n = 154) were randomly allocated to a rocuronium-0.6, rocuronium-0.9, or magnesium group. The magnesium group was pretreated with 50 mg/kg MgSO4, and the other two groups received the same volume of isotonic saline. Anesthesia was induced with alfentanil, propofol, and either 0.6 mg/kg (rocuronium-0.6 and magnesium groups) or 0.9 mg/kg (rocuronium-0.9 group) rocuronium. An anesthesiologist, blinded to the group assignments, performed RSI and assessed the intubating conditions. Systolic arterial pressure (SAP) and heart rate (HR) were recorded before the magnesium sulfate or normal saline was administered, before anesthesia induction, before intubation, and every minute after intubation for 5 min.
Results
Airway features were similar among the three groups. The intubating conditions were improved significantly in the magnesium group (P < 0.001) compared with the other two groups. Significant increases in SAP at 1 min after intubation were observed in the rocuronium-0.6 and -0.9 groups when compared with the magnesium group (P < 0.05). HR was comparable among the three groups (P > 0.05). No hypertensive episode occurred during the immediate post-intubation period in the magnesium group (P = 0.001), and tachycardia occurred most frequently in the rocuronium-0.6 group (P < 0.05).
Conclusions
MgSO4 administered prior to RSI using alfentanil, propofol, and rocuronium may improve intubating conditions and prevent post-intubation hypertension.
Introduction
Rapid sequence intubation (RSI), also called rapid sequence induction, rapid tracheal intubation, or fast tracheal intubation, is required for patients with a high risk for aspiration, even when it is not an emergency situation [1]. This procedure involves preoxygenation, rapid administration of a series of drugs, cricoid pressure assessment, and prompt intubation within 1 min of administering a non-depolarizing neuromuscular blocking agent (NMBA). Hypertension or tachycardia may be aggravated in response to sympathetic stimulation by tracheal intubation during or immediately after RSI, and inadequate muscle paralysis may lead to vocal cord or diaphragm movement or cough [2-4].
Magnesium sulfate (MgSO4) has two distinctive advantages when used during tracheal intubation. First, it potentiates the effects of NMBAs such as cisatracurium, mivacurium, vecuronium, and rocuronium [5-8]. Succinylcholine has been considered the drug of choice for RSI; however, it is contraindicated in a number of clinical situations, including major burn or crush injuries (> 48 h), major spinal cord injuries, and history of malignant hyperthermia [9,10]. Rocuronium can be used as an alternative agent in such cases. The onset of action, from the administration of rocuronium until 95% suppression of the first twitch [11], is faster at higher doses of rocuronium [3] and is shortened by pretreatment with MgSO4 [8]. Second, MgSO4 has anti-adrenergic effects by decreasing catecholamine release from the adrenal medulla or adrenergic nerve endings, and it causes vasodilation and an anti-arrhythmic effect on the heart [12,13]. Magnesium-treated patients show more stable arterial pressure and heart rate with a lower plasma concentration of catecholamines during tracheal intubation [14].
Considering these advantages of MgSO4, we hypothesized that with MgSO4 pretreatment, RSI conditions would improve and the hemodynamic responses following RSI would be more stable. Thus, we investigated intubating conditions during RSI among patient groups administered a high dose of rocuronium or a conventional dose of rocuronium with or without MgSO4 pretreatment.
Materials and Methods
This study was approved by the Institutional Review Board (approval number, B-1011-056-004; Seoul National University Bundang Hospital, South Korea) and is registered at clinicaltrials. gov (NCT01153256). All subjects provided written informed consent to participate in the study.
This double-blind, randomized, controlled trial was conducted in patients aged 20-65 years with American Society of Anesthesiologists classification I or II, who were scheduled for elective operations under general anesthesia. Preoperative exclusion criteria were an emergent operation, pregnancy, neuromuscular disease, renal disease, body mass index > 30 kg/m2 or < 16.5 kg/m2, anticipated difficult airway due to any disease or abnormal condition of the airway, chronic medication use with calcium channel blockers or magnesium-containing drugs, and a known history of allergy to MgSO4 or other anesthetic drugs.
Using the sealed envelope method, eligible patients were randomly allocated into one of three groups: 0.6 mg/kg rocuronium with MgSO4 pretreatment (magnesium group), 0.6 mg/kg rocuronium with isotonic saline instead of MgSO4 (rocuronium-0.6 group), and 0.9 mg/kg rocuronium with isotonic saline (rocuronium-0.9 group). Midazolam (0.03 mg/kg) was administered intravenously 5 min prior to transferring the patients to the operating room. Standard monitoring (electrocardiogram, pulse oximetry, and non-invasive blood pressure) was established upon arrival in the operating room. Patients in the magnesium group received 50 mg/kg MgSO4 in 100 ml of isotonic saline over 15 min. Patients in both rocuronium groups (0.6 and 0.9) received the same volume of isotonic saline in place of MgSO4 over the same time period. Patients were simultaneously preoxygenated with 100% oxygen for 5 min. Anesthesia was induced identically in the three groups using 10 µg/kg alfentanil followed by 2 mg/kg propofol. Rocuronium (0.6 mg/kg in the magnesium and rocuronium-0.6 groups and 0.9 mg/kg in the rocuronium-0.9 group) was administered without interruption. To maintain blinding of the study, rocuronium was diluted in isotonic saline to a 10 ml total volume. All study drugs (MgSO4, isotonic saline, rocuronium) were prepared by one anesthesia nurse, and the attending anesthesiologist was unaware of the group allocations.
Mask ventilation was not performed until tracheal intubation unless the peripheral oxygen saturation (SpO2) decreased below 95%. Tracheal intubation was performed 50 s after rocuronium administration by one blinded expert anesthesiologist. Cases in which tracheal intubation was not completed within 60 s after rocuronium administration were regarded as failed cases and were excluded from the study.
After intubation, anesthesia was maintained with oxygen, medical air, and 1.5% sevoflurane. Whenever hypertension [systolic arterial pressure (SAP) ≥ 150 mmHg] or tachycardia [heart rate (HR) ≥ 110 bpm] occurred during the 5-min post-intubation period, an intravenous calcium channel blocker (0.5-1 mg nicardipine) or β-blocker (5-10 mg esmolol) was administered, respectively. Intravenous ephedrine (5-10 mg) or atropine (0.5 mg) was administered in the event of hypotension (SAP ≤ 80 mmHg) or bradycardia (HR ≤ 50 bpm), respectively.
Intubating conditions were assessed as a primary outcome using the intubation scoring system of the Good Clinical Research Practice guidelines [11]. SAP and HR were recorded at eight time points: baseline before MgSO4 or normal saline were administered (T-baseline), before induction (T-induction), before intubation (T-intubation), and every minute for 5 min thereafter (T1, T2, T3, T4, and T5). The incidences of nicardipine, esmolol, ephedrine, or atropine administration were evaluated. Adverse events, including a burning sensation in the MgSO4-infused arm, a heat sensation in the body, palpitations, and arrhythmia, were evaluated during MgSO4 or saline administration.
Statistical analysis
The primary outcome variable used for the power calculation analysis was the different proportion of the incidence of intubating conditions among three groups. The pilot cases of each group were distributed as follows; magnesium group (16/2/2 in excellent, good, and poor intubation condition), rocuronium-0.9 group (8/6/5), and rocuronium-0.6 group (6/8/8). When type I error has been set at 0.01, this study has power of 99% with 51 patients per group. Assuming a dropout rate of 10%, 56 patients were recruited for each group. The data are reported as mean ± standard deviation or number (%). Differences in intubating conditions among the three groups were analyzed using the chi-square test. For multiple comparisons by Bonferroni correction, the desired alpha cut-off value (0.05) was divided by the number (3) of the comparisons we made (P < 0.05/3). SAP and HR were analyzed using repeated-measures analysis of variance, and Tukey's test for post hoc analysis was performed to detect any significant differences among groups. SPSS software ver. 18.0 (Chicago, IL, USA) was used, and a P value < 0.05 was considered to indicate significance.
Results
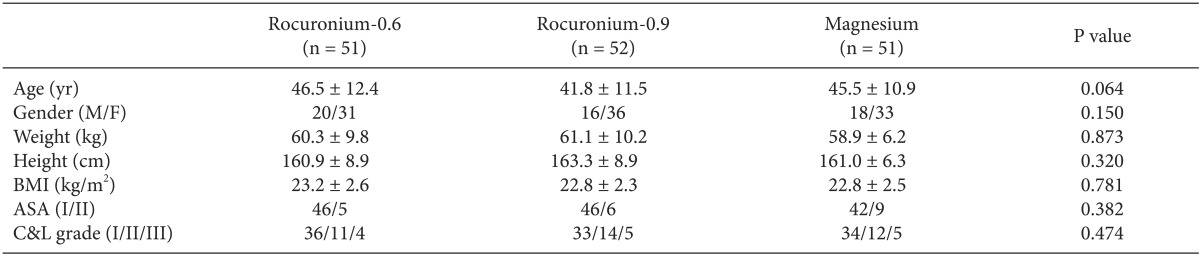
In total, 168 patients were recruited between October 2010 and March 2011, and 154 patients were finally analyzed (Fig. 1). Airway features were comparable among the groups (Table 1). No patient showed hypoxemia (SpO2 < 95%) in the 1-min apnea period during anesthetic induction.
Significant differences in the intubating conditions were observed among the three groups (P < 0.001) (Fig. 2A). Intubating conditions were significantly better in the magnesium group than in the rocuronium-0.6 (P < 0.001) or rocuronium-0.9 group (P = 0.001). A significant difference was observed between the rocuronium-0.6 and rocuronium-0.9 groups (P = 0.008). When both excellent and good intubating conditions were regarded as clinically acceptable, significant differences remained among the three groups (P < 0.001; Fig. 2B). There were more cases with clinically acceptable intubating conditions in the magnesium group than in the rocuronium-0.6 (P < 0.001) or rocuronium-0.9 group (P = 0.004). The incidence of clinically acceptable intubating conditions also differed significantly between the rocuronium-0.6 and rocuronium-0.9 groups (P = 0.002).

Intubating conditions in the three groups. (A) The incidence (%) when intubating conditions are evaluated as excellent, good, and poor. (B) The incidence (%) when excellent and good intubating conditions are considered clinically acceptable conditions, and poor conditions are considered clinically unacceptable. Intubating conditions among the three groups show statistically significant differences (P < 0.001) in both (A, B). Rocuronium-0.6 group: 0.6 mg/kg rocuronium, Rocuronium-0.9 group: 0.9 mg/kg rocuronium, Magnesium group: 0.6 mg/kg rocuronium with magnesium sulphate pretreatment.
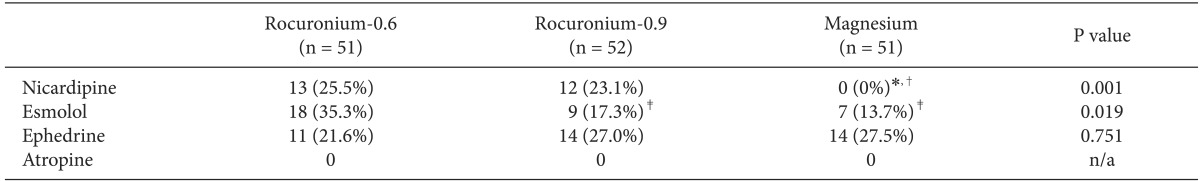
Changes in SAP were significantly different among the three groups (P < 0.05; Fig. 3A). SAP of the magnesium group differed from SAP of the rocuronium-0.6 (P < 0.05) and rocuronium-0.9 groups (P < 0.05). SAP at 1 min (T1) following intubation was significantly lower in the magnesium group compared with the rocuronium-0.6 (P < 0.001) and rocuronium-0.9 groups (P < 0.001). However, changes in HR (Fig. 3B) were comparable among the groups (P > 0.05). The incidences of administering each cardiovascular drug during the post-intubation period are shown in Table 2. No patient in the magnesium group required nicardipine (P = 0.001), and esmolol was administered most frequently in the rocuronium-0.6 group P < 0.05 (corrected). Hypotension did not occur frequently after intubation in any group; the incidences of ephedrine administration were comparable among the groups (P > 0.05). No patient required atropine.

Changes in systolic arterial pressure (A) and heart rate (B) in the three groups. Rocuronium-0.6 group: 0.6 mg/kg rocuronium, Rocuronium-0.9 group: 0.9 mg/kg rocuronium, Magnesium group: 0.6 mg/kg rocuronium with magnesium sulphate pretreatment, T-baseline: before magnesium sulphate or normal saline was administered, T-induction: before induction, T-intubation: before intubation, T1, T2, T3, T4, and T5: 1, 2, 3, 4, and 5 min after intubation, respectively. *P < 0.05 compared with the rocuronium-0.6 and the rocuronium-0.9 group.
Minor adverse events occurred more frequently in the magnesium group than in the other groups (P < 0.001). Two patients (6.7%) in the rocuronium-0.6 group and one (3.3%) in the rocuronium-0.9 group experienced a burning sensation in the vein. In the magnesium group, eight patients (15.7%) reported a burning sensation in the vein, and 11 patients (21.6%) experienced a heat sensation in the body. Palpitations without arrhythmia were reported in three patients (5.9%) in the magnesium group. These adverse events resolved spontaneously and did not require further treatment. Arrhythmia other than tachycardia or bradycardia was not detected in any patient.
Discussion
We showed that intubating conditions during RSI were improved and that hypertension after RSI could be effectively prevented by additional administration of MgSO4. These findings seem to result from the potentiation of NMBA action and attenuation of the cardiovascular response by MgSO4.
At higher doses of rocuronium, the onset of action is faster [3]; therefore, it is conceivable that the rocuronium dose was a factor in determining the intubating conditions during RSI. However, in a previous study, there was no difference in the frequency of excellent or clinically acceptable intubation conditions during RSI between a group receiving 0.9-1.0 mg/kg rocuronium and a group receiving 1.2 mg/kg rocuronium [10]. In addition, Lysakowski et al. [15] reported that when propofol is used as an RSI induction agent, just a two-fold ED95 (0.6 mg/kg) of rocuronium was adequate to achieve intubation conditions similar to those produced by succinylcholine. Larsen et al. [16] used alfentanil and propofol as RSI induction agents and also reported that 0.6 mg/kg rocuronium could substitute for succinylcholine.
Our results showed that 0.6 mg/kg rocuronium was sufficient to achieve excellent or clinically acceptable intubating conditions when MgSO4 was used as a pretreatment. The outcome of the magnesium group was even better than that of the rocuronium-0.9 group. Hubbard et al. reported that it took at least 4-6 min for MgSO4 to affect the end-plate potential after increasing the magnesium concentration [17]; thus, we administered MgSO4 for 15 min prior to anesthesia induction. Czarnetzki et al. also showed that the onset time of rocuronium was shortened to an average of 77 s when MgSO4 was preadministered, which is similar to our study (60 mg/kg for 15 min before induction of anesthesia) [8]. Therefore, MgSO4 shortened the onset of rocuronium action, which consequently played a role in improving the RSI intubating conditions in our study.
In addition, clinically unacceptable RSI intubating conditions can result in cardiovascular instability during the immediate post-intubation period. Rapid-onset opioids such as alfentanil or remifentanil have often been administered to facilitate RSI and attenuate the cardiovascular response [18-20]. However, the best opioid and the optimal dose remain unknown. Although high doses of opioids can blunt the cardiovascular response to intubation, they often result in prolonged hypotension and bradycardia [18,21]. Furthermore, some clinicians worry about potential opioid side effects such as respiratory muscle rigidity and vocal cord closure during RSI [22-24].
MgSO4 can decrease SAP through a direct relaxing effect on blood vessels and by anti-adrenergic effects mediated by calcium antagonism. Sakuraba et al. [25] reported that prior administration of MgSO4 (40 mg/kg) effectively limited the intubation-induced cardiovascular changes after RSI. Compared with the rocuronium-0.6 and rocuronium-0.9 groups, the magnesium group had an understandably lower SAP at the T1 point (Fig. 3A). However, SAP at the T1 point was not different from the baseline SAP in the rocurocnium-0.6 and -0.9 groups, i.e., severe hypertensive episodes were not observed even though MgSO4 was not administered. Two factors should be considered. First, alfentanil, which blunts the intubation response, was administered to all patients for anesthesia induction. Second, esmolol was administered immediately if HR increased to > 110/min after intubation. This procedure might have kept SAP from rising steeply at T1. Thus, we should consider the frequency of nicardipine and esmolol usage together. Arterial pressure in the magnesium group remained stable for the entire observation period, even though nicardipine was never administered to any case in the magnesium group. Although the HR records were not different among the three groups (Fig. 3B), the frequency of esmolol administration was lowest in the magnesium group. Consequently, prior administration of MgSO4 for RSI had an additional effect on SAP and HR stability. This could be particularly advantageous in patients with cardiovascular or cerebrovascular disease and those in whom severe hypertension or tachycardia should be avoided [26].
Although MgSO4 can be clinically useful during RSI, adverse events must be considered. Complaints from the patients in the magnesium group included heat sensations in the body, burning sensations in the vein, and palpitations. These symptoms resolved spontaneously without further management and did not interrupt the MgSO4 infusion. No severe adverse effects were reported in a systematic review of studies on the postoperative analgesic effects of magnesium (MgSO4 dose 30-50 mg/kg or 3-4 g bolus administration in recruited studies) [27]. Thus, pretreatment with MgSO4 prior to NMBAs during RSI can be used with only minor adverse events.
This study had two limitations. First, we did not compare the intubating conditions with succinylcholine, and second, the time course of rocuronium was not monitored. There are currently no non-depolarizing NMBAs that have a shorter duration than succinylcholine, whether MgSO4 is co-administered or not [3]. Interactions between MgSO4 and non-depolarizing NMBAs (vecuronium, mivacurium, cisatracurium, or rocuronium) have been widely investigated in many clinical studies, which have reported shortened onset time, prolonged clinical duration, or increased potency of non-depolarizing NMBAs by MgSO4 [5-8,28]. Moreover, an intraoperative MgSO4 infusion could reduce the total requirement for a non-depolarizing NMBA when given with neuromuscular monitoring [29,30], which in turn would not delay recovery from neuromuscular blockade, particularly during long surgeries. However, it may still be a concern during short surgeries. Thus, we should be cautious when using MgSO4 with a non-depolarizing NMBA during short-duration surgeries or in special situations when difficult mask ventilation or difficult intubation is expected.
In conclusion, our results confirmed that pretreatment with MgSO4 improved intubating conditions during RSI using alfentanil, propofol, and rocuronium. Moreover, MgSO4 was an effective adjuvant to prevent hypertension and tachycardia following RSI. These results will be beneficial to patients with cardiovascular or cerebrovascular disease, as it is desirable to prevent severe fluctuations in arterial pressure and/or HR during or immediately after tracheal intubation in these patients.