The effects of hip abduction with external rotation and reverse Trendelenburg position on the size of the femoral vein; ultrasonographic investigation
Article information
Abstract
Background
Femoral vein (FV) catheterization is required for critically ill patients, patients with difficult peripheral intravenous access, and patients undergoing major surgery. The purpose of this study was to evaluate the effects of hip abduction with external rotation (frog-leg position), and the frog-leg position during the reverse Trendelenburg position on diameter, cross-sectional area (CSA), exposed width and ratio of the FV using ultrasound investigation.
Methods
Ultrasonographic FV images of 50 adult subjects were obtained: 1) in the neutral position (N position); 2) in the frog-leg position (F position); 3) in the F position during the reverse Trendelenburg position (FRT position). Diameter, CSA, and exposed width of the FV were measured. Exposed ratio of the FV was calculated.
Results
The F and FRT positions increased diameter, CSA and exposed width of the FV significantly compared with the N position. However, the F and FRT positions had no significant effect on exposed ratio of the FV compared with the N position. The FRT position was more effective than the F position in increasing FV size.
Conclusions
The F and FRT positions can be used to increase FV size during catheterization. These positions may increase success rate and reduce complication rate and, therefore, can be useful for patients with difficult central venous access or at high-risk of catheter-related complication.
Introduction
Central venous catheterization is necessary for aggressive fluid resuscitation, for central venous pressure monitoring, in patients with lack of peripheral venous access, and administration of parenteral nutrition and medication likely to induce phlebitis when administered through a peripheral vein [1].
The femoral vein (FV) was not a preferred route for central venous catheterization because of its higher incidence of catheter colonization, bacteremia and venous thrombosis compared with the internal jugular and the subclavian vein [2-5]. However, several studies found that catheter-associated infection rate and thrombosis rate were not increased significantly by femoral vein catheterization when compared to catheterization at other sites [6-9]. In addition, there were advantages using the FV for central venous catheterization during cardiopulmonary resuscitation. Easily identifiable anatomic landmarks make cannulation easy, and the distance from the head and chest makes cannulation possible without risk of pneumothorax and does not interfere with cardiopulmonary resuscitation [10].
Although FV catheterization is relatively easy, it is challenging to insert a FV catheter by standard landmark-oriented approach in patients with severe hypotension or cardiac arrest [11]. Maneuvers that increase FV size may improve success rate of cannulation, but knowledge of methods to increase FV size is limited [12-17] despite a number of well established maneuvers being suggested as methods to increase the size of the internal jugular and subclavian veins [18-24].
There are few reports evaluating the effect of both the frog-leg position and the reverse Trendelenburg position (RT) on FV size. The purpose of this study was to evaluate the effects of the frog-leg position, alone or during the reverse Trendelenburg position, on diameter, cross-sectional area (CSA), exposed width and ratio of the FV using ultrasound investigation.
Materials and Methods
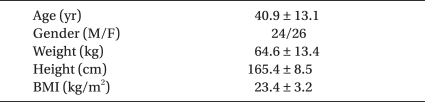
After obtaining approval of the Institutional Review Board and written informed consent, fifty patients (American Society of Anesthesiologists physical status I-II and between the ages of 18 and 65 years) scheduled for elective surgery under general anesthesia were enrolled. All participants did not require central venous catheterization. Patients with hypovolemia, systolic blood pressure < 90 mmHg, inability to externally rotate or abduct the hip joint, history of deep vein thrombosis, or FV catheterization or surgery in the inguinal region were excluded. Among the 50 enrolled subjects, 24 were male and 26 were female, with a mean age of 40.9 ± 13.1 years. Demographic data are shown in Table 1.
The following definitions were used :
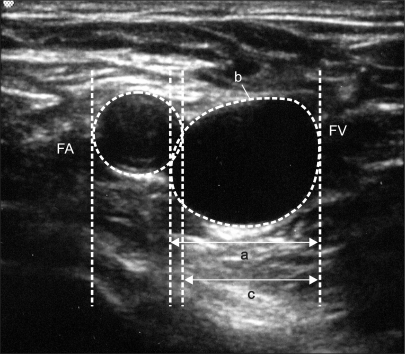
Diameter: longest distance of the line segment that passes through the FV (Fig. 1).
CSA: total area of the FV when viewed from a transverse plane (Fig. 1).
Exposed width of the FV: FV length not overlapped by the femoral artery (FA) (Fig. 1).
Exposed ratio of the FV: ratio of exposed width to FV diameter.
All measurements were performed after the end of the surgery, with anesthesia maintained using end-tidal sevoflurane 1.0-1.5 vol% in an oxygen/N2O mixture, and neuromuscular blockade was not reversed.
Ultrasound images were obtained from the right common FV using a SonoSite M-turbo (SonoSite®, Bothell, Washington, USA) with a 5-12 MHz linear transducer. The transducer was held over the pulsation of the FA, just above the bifurcation of the great saphenous vein. The FV was identified by its collapsibility under gentle pressure generated by the transducer. Diameter, CSA, and exposed width of the FV were measured according to each position: 1) in the horizontal supine position with the leg straight (neutral position; N position); 2) in the frog-leg position (F position); 3) in the F position during the RT position (FRT position). The F position was achieved by abduction and external rotation of the hip along with flexion of the knee, so that the right sole of the foot touched the medial epicondyles of the left femur and tibia. The reverse Trendelenburg position was achieved by tilting the operating table to an angle of 15 degrees, measured by a protractor at the center of the operating table.
All ultrasound images were obtained by the same investigator. Measurements were made after patients had been in position for at least 1 minute. The image showing the largest FV size was chosen. When the investigator outlined FV circumference, CSA was automatically calculated by the ultrasound machine.
Data were analyzed using the repeated measurement of analysis of variance using SPSS version 18.0 (SPSS Inc., Chicago, Illinois, USA). P values were adjusted using a Bonferroni correction at an overall significance level <0.05. Data were presented as mean ± SD.
Results
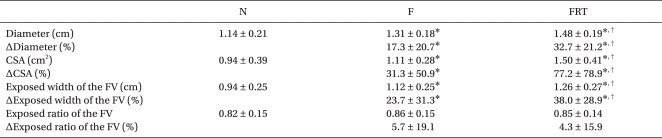
The F and FRT positions significantly increased FV diameter, CSA, and exposed width (17.3% and 32.7%, P < 0.001; 31.3% and 77.2%, P < 0.001; 23.7% and 38.0%, P < 0.001; respectively) (Fig. 2, Table 2) compared with the N position. However, exposed ratio of the FV was not significantly increased (P = 0.061) (Table 2).
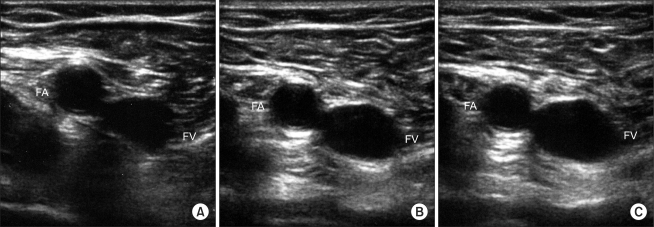
Ultrasonographic images of the femoral vein in a subject in the neutral (A), frog-leg (B), and frog-leg position during the reverse Trendelenburg position (C). Diameter, cross-sectional area, and exposed width of the femoral vein increased significantly in the frog-leg position and the reverse Trendelenburg position with the frog-leg position. FV: femoral vein, FA: femoral artery.
Discussion
This study demonstrated that the F and FRT positions significantly increased diameter, CSA, and exposed width of the FV. The FRT position was more effective than the F position in increasing FV size.
The RT position has been reported to increase FV CSA. Stone et al. [12] reported that the RT position significantly increased CSA by 55.2% in awake adults. Kim et al. [13] reported that the RT position increased CSA by 50% in awake adults. Suk et al. [14] reported that the RT position increased CSA by 21.1% in infants and 24.7% in children, both anesthetized. We did not study the RT position alone. However, from our results that the F position increased FV CSA by 31.3% and the FRT position increased CSA by 77.2%, we can infer that the increase in CSA had been amplified by the RT position.
Although central venous catheterization is valuable in acute resuscitation, its complication rate is approximately 15% [10]. Reported rates of central catheter-related complications range from 5-19% for mechanical complications [2,10,25], 5-26% for infectious complications [2,3,26], and 2-26% for thrombotic complications [4,5,9]. Arterial puncture and hematoma are the most common mechanical complications during FV catheterization. Our study demonstrated that the F and FRT positions significantly increased FV size. From this result, we can infer that complication rate may decrease by placing patients in the F or FRT position before performing FV catheterization.
Many studies have used diameter and CSA as values representing FV size [12-17]. In this study, in addition to diameter and CSA, we measured exposed width of the FV, because that is where cannulation should be done. The anatomic relationship between the FA and FV has been evaluated but results vary [27,28]. Baum et al. [27] demonstrated that among the 200 vessel pairs evaluated, 35% of the FA was parallel to the FV in the medial-lateral plane, and 65% overlapped the FV in the anterior-posterior plane at various degrees. Warkentine et al. [28] reported that the FV was completely or partially overlapped by the FA in 12% of cases. Overlapping of the FV by the FA can lead to inadvertent arterial catheterization or arteriovenous fistula. Therefore, the larger the exposed width of the FV is, the greater the chances of a successful FV cannulation without complications.
In this study, in spite of the significant increase in diameter, CSA and exposed width of the FV, exposed ratio of the FV was not significantly increased in the F or FRT position compared with the N position. This result is similar to that of Hopkins et al. [29]; however, it is inconsistent with the report of Werner et al. [16]. Hopkins et al. [29] found that the percentages of FV overlapped were similar between the straight and F positions in children. Werner et al. [16] reported that the mean percentage of FV accessible in the F position was significantly greater than in the leg straight (70.4 ± 26.6). Meanwhile, in our study, exposed ratio of FV insignificantly increased from 0.82 ± 0.15 to 0.86 ± 0.15. Conflicting results between the two studies arose from a difference in baseline values (70.4 and 0.82), which was perhaps due to differences in positioning or measurement technique.
Our study has several limitations. One investigator obtained all ultrasonographic images in order to achieve consistency of measurement, but the investigator was not blinded to the positions, which might have introduced bias into the study. We did not examine the actual success rates of cannulation. Further studies are required to demonstrate whether the F and FRT positions actually improve success rate of FV cannulation. Our study was limited to non-obese adults. Future studies should include assessing FV size in pediatric, geriatric and obese patients. Despite the significant increase in FV size in the RT position, the RT position may be not appropriate in all situations, as it decreases venous return to the heart. This may decrease preload and induces hypotension in hemodynamically unstable patients. For patients with hypotension, the RT position should be carefully performed under close monitoring of blood pressure.
In conclusion, this study demonstrated that both the F and FRT positions were associated with significant increases in diameter, CSA, and exposed width of the FV in adult subjects. The FRT position was more effective than the F position in increasing FV size. These findings suggest that the F and FRT positions can be used to increase FV size during catheterization, which may increase success rate and reduce complication rate. Therefore, these positions can be useful for patients with difficult central venous access or at high-risk of catheter-related complication.