|
 |
|
|
Abstract
A 53-year-old man had chronic low back and leg pain for four years without any history of trauma or neurological manifestations. There was a reduction in symptoms after a lumbar epidural block. Two hours later after the procedure, the patient complained of perineal numbness and lower extremity weakness. The neurological evaluation revealed loss of sensation in the saddle area and the posterior aspect of the leg. The deep-tendon reflexes were decreased in the leg. The patient was unable to urinate. The MRI revealed a schwannoma at the S3 level of the sacral spine with cauda equina compression. The patient's symptoms improved slightly over the next few hours. The patient had a gradual return of motor function and could feel the Foley catheter. All of the symptoms completely resolved over the next nine hours and the patient was discharged to home once completely recovered. This case illustrates the importance of clinical examination and continued vigilance for evaluation of neurological deterioration after epidural injections.
Many patients that have low back pain present to pain clinics. It is important to accurately diagnose the cause of the pain and provide safe and appropriate treatment. There are many causes of low back pain, and there are a variety of treatments available for the different causes [1]. Drug infusion into the epidural space is a blocking method that has been used for a long time to treat low back pain. The interlaminar approach of epidural blocks and caudal epidural blocks are often used for out-patient treatment. Epidural blocks are safe and simple to perform and commonly used in patients with chronic low back pain. However, these treatments may be used too frequently. Complications associated with epidural blocks are rare, but nevertheless, the anesthesiologist must be vigilant in monitoring patients after the procedure. Here, a male patient that had a history of several years of chronic low back pain is reported. The patient had a lumbar epidural block that triggered a transient cauda equina syndrome. Here we discuss the etiology of the patient's symptoms and treatment.
A 53-year-old patient who had a history of many years of low back pain was admitted to the pain clinic. The low back pain started four years ago. The patient had visited private clinics, Presbyterian Medical Center's department of neurosurgery, pain clinics, and rehabilitation centers. He was treated with analgesics, had many lumber medial branch blocks, and received physical therapy.
The symptoms steadily progressed. Two years before presentation, a lumbar CT was performed that showed a herniated disc. When admitted to the pain clinic, the VAS score for continuous pain was 6-7. Physical therapy did not improve the pain significantly. There was no dyskinesia or paresthesia on physical examination. The reflexes were intact. The straight leg raising test showed that the right leg was within normal limits. However, the straight leg raising test was positive in the left leg at 60 degrees. The patient's pain was predominantly in the gluteal and femoral regions. The lumbar CT from two years ago showed that L4 and L5 were slightly protruded to the left and compressed the dura mater. In addition, L5 and S1 were found to be bulging. There was no additional significant family history. The treatment he had been receiving did not improve the symptoms. The patient complained of severe pain in the gluteal and femoral regions and requested a nerve block. A lumbar epidural block was chosen. The procedure was explained to the patient and he consented to proceed.
The patient lay on his side. By using the loss or resistance method to find the epidural space, 0.1% ropivacaine 12 ml (Naropin®, Astrazeneca, Sweden) and triamcinolone acetonide 40 mg (TAMCETON INJ®, Hannall Inc.) were infused aseptically with a 22 gauge epidural needle (Hakko, Japan) in between the L4 and L5 spaces by the interlaminar approach. After the procedure, the VAS score decreased to 3-4. The patient returned home. Around two hours later, the patient reported hypoesthesia of the perineum and weakness in the lower extremities; he returned for additional care. The neurological examination showed both femurs and the gluteal region had muscle weakness. The S1 to S5 dermatome had hypoesthesia. Deep tendon reflex testing showed that the Achilles' reflex was reduced, bilaterally. The patient reported difficulty urinating. The cauda equina syndrome was suspected. To diagnose the cause of these additional findings, an MRI of the sacrolumbar area was performed. The results showed that the L4 and L5 regions were slightly protruded, which caused slight compression of the left frontal areas of L5 to S1. In addition, a tumor that appeared to be a schwannoma in the left spinal canal at C3 was identified that pressed the cauda equina to the right. There was no sign of a hematoma (Fig. 1-4). Over time, the patient's muscles slowly recovered, and he could feel the Foley catheter. About nine hours after the procedure, the neurological symptoms resolved. The next day the VAS score was 5. The patient was discharged from the hospital. After the MRI results, the patient was examined by the department of neurosurgery. The patient declined surgery, and chose a nerve block instead. However, we were concerned about post epidural block-neurological complications. The epidural block was not performed. Instead, dicode® 120 mg/day (dihydrocodeine tartrate, Hana Pharm Co., Ltd.) and airtal® 200 mg/day (aceclofenac, Daewoong Co. Ltd.) were prescribed and ambulatory care was provided. The patient is being followed with improved symptoms.
There are numerous causes of low back pain, such as a radiculopathy due to a herniated disc, ligament regeneration in the spinal canal area, spinal canal stenosis by regressive change of the zygapophysial joint, and radiating pain from the discogenic pain syndrome. There are different treatments for the different causes [1]. Lower back pain is a common disorder affecting 80% of the world's population at least once in a person's life, and such pain is associated with a very high socialeconomic cost [2]. Therefore, accurately diagnosing the cause of the low back pain and the appropriate treatment is likely to improve the patient's prognosis and reduce the social economic cost.
Spinal tumors reportedly occur in 3-10 out of 100,000 persons. They occur most commonly in the age range of 40-50 [3]; 50% of cases present with thoracic pain, 30% cervical and 20% involve the sacro-lumbar area. Spinal tumors are classified as extradural, intradural-extramedullary, or intradural-intramedullary. Spinal schwannomas account for 25% of adult intradural-extramedullary spinal tumors [4,5] and occur in 3-4 out of every 1 million persons [6]. They are diagnosed by radiologic examination and isotope tests, and they can be suspected based on the patient's neurological symptoms. Simple spinal CTs are the most commonly used diagnostic tests; they show the destruction of the vertebral body or pedicle and soft tissue edema, but only when the loss of spinal matter has progressed.
In the present case, a lumbar CT was performed, but the caudal area was not included in the CT, and the tumor was not visualized. The low back pain was considered to be due to the slight left protrusion of L4-L5 slightly pressing on the dura mater, as well as the expansion of L5-S1; it was assumed the patient was treated for these problems. However, because the symptoms did not improve and there was severe pain in the gluteal and femoral regions, the patient requested a neural block. An epidural block was performed. Drug infusion into the epidural space is one of the oldest treatments for low back pain. Customarily, interlaminar epidural blocks and caudal epidural blocks are performed in the out-patient setting. For caudal epidural blocks a needle is injected through the sacral hiatus to the sacral canal for drug infusion [7]. This approach is widely used for lumbar and sacral dermatome anesthesia and for chronic low back pain treatment [8]. Epidural steroid infusion is effective in patients with radiculopathy due to spinal neural compression [9]. In order to treat the symptoms of the dural compression, from the disc protrusion and the pain in the gluteal and femoral region in the present case, a lumbar epidural block was performed, which reduced the patient's pain score to 3-4 on the VAS.
The cauda equina syndrome compresses multiple nerve roots of the sacro-lumbar area and manifests neurological symptoms such as pain in the back, the pelvis, or the lower extremities, as well as vesical dysfunction. Post-epidural block-cauda equine syndrome is a very rare complication. It is caused by spinal cord compression, ischemia, trauma, neurotoxicity, epidural hematoma, or abscess formation. The patient in the present case did not have neurological symptoms before the epidural block, and the MRI performed after the block did not identify a hematoma or abscess. However, it did show a slight protrusion of L4-L5, which slightly compressed the left-front dura mater of L5-S1; in addition, a tumor was identified that appeared to be a schwannoma in the left spinal canal at C3 that was compressing the cauda equine to the right. Drug infusion in the structurally narrowed epidural space may have increased the pressure in the epidural space and the subarachnoid space. This may have triggered transient nerve root compression by the adjacent organs.
The type of drugs infused in the epidural space play an important role in the effects experienced by the patient. Usubiaga et al. [10] reported compression of the epidural space and the subarachnoid space after lumbar epidural administration of natural saline; the larger the amount and the more rapid the infusion the greater the increase of the compression. McLain et al. [11] reported that drugs infused in the epidural space can form a loculation and temporarily compress the spinal cord; and after the epidural block, it can cause paralysis of the lower extremities. In the present case, 12 ml of the drugs were infused into the epidural space. Several hours later, the neurological symptoms were observed. The infused drugs may have caused a loculation and transiently compressed the spinal cord, which must have been the cause of the cauda equina syndrome.
Another cause of the cauda equina syndrome after an epidural block may be spinal cord ischemia from a spasm of the anterior spinal artery or the Adamkiewicz artery. This occurs with the use of vascular constrictors such as epinephrine, hypotension, and irritation from an epidural catheter. In the present case, no vascular constrictors were used, there was no hypotension, and a catheter was not used. Therefore, the symptoms were unlikely due to ischemia.
When drugs are infused into the epidural space, the local anesthetic can inadvertently be injected into the subdural or subarachnoid space, which can cause neurotoxicity [12]. The anatomical structure of the cauda equina includes the dorsal root of L5 and S1's spinal nerves are located at the most dorsal area of the spinal canal. In the supine position S1 is exposed for hyperbaric local anesthesia. Cauda equina nerve roots do not have the epineural sheath of the peripheral nerves; even low concentrations of anesthetics can cause neurological damage. However, in the present case, hyperbaric anesthetics were not used. The patient's neurological symptoms appeared two hours after the epidural block; the cauda equina syndrome did not appear to be from inadvertent subdural or subarachnoid infusion of the anesthetics. However, a large amount of drug infusion in the narrowed epidural space might have caused an increase in pressure causing the drug to leak into the subarachnoid area. Direct damage to the spinal cord and neural muscles can also cause the cauda equina syndrome. However, the explanation for this is unclear. It was not likely the cause, because when the needle was inserted, there was no neurological pain, dysethesia, or motor abnormality.
Although spinal tumors are rare, they should be suspected when the patient has continuous low back pain [13]. In Korea, there have been reports of spinal tumors identified in patients with symptoms not alleviated by treatment [13,14]. In conclusion, a patient with chronic low back pain due to cauda equina compression from a sacral schwannoma had drugs infused into the structurally narrowed epidural space, which is assumed to have caused a transient cauda equina syndrome.
References
1. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine 2002; 27: 11-16. PMID: 11805628.


2. Frymoyer JW, Cats-Baril WL. An overview of the incidences and costs of low back pain. Orthop Clin North Am 1991; 22: 263-271. PMID: 1826550.


3. Alter M. Edited by Vinken PJ, Bruyn GWStatistical aspect of spinal cord tumors. Handbook of Clinical Neurology. 1975, : New York, N.Y., North-Holland Publishing Company. pp 1-22.
4. De Verdelhan O, Haegelen C, Carsin-Nicol B, Riffaud L, Amlashi SF, Brassier G, et al. MR imaging features of spinal schwannomas and meningiomas. J Neuroradiol 2005; 32: 42-49. PMID: 15798613.


5. Celli P, Trillò G, Ferrante L. Spinal extradural schwannoma. J Neurosurg Spine 2005; 2: 447-456. PMID: 15871485.


6. Seppälä MT, Haltia MJ, Sankila RJ, Jääskeläinen JE, Heiskanen O. Long-term outcome after removal of spinal schwannoma: a clinicopathological study of 187 cases. J Neurosurg 1995; 83: 621-626. PMID: 7674010.


7. Chen CP, Tang SF, Hsu TC, Tsai WC, Liu HP, Chen MJ, et al. Ultrasound guidance in caudal epidural needle placement. Anesthesiology 2004; 101: 181-184. PMID: 15220789.


8. Carette S, Leclaire R, Marcoux S, Morin F, Blaise GA, St-Pierre A, et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med 1997; 336: 1634-1640. PMID: 9171065.


9. White AH, Derby R, Wynne G. Epidural injections for the diagnosis and treatment of low back pain. Spine 1980; 5: 78-86. PMID: 6444766.


10. Usubiaga JE, Usubiaga LE, Brea LM, Goyena R. Effect of saline injection on epidural and subarachnoid space pressures and relation to postspinal anesthesia headache. Anesth Analg 1967; 46: 293-296. PMID: 6067279.

11. McLain RF, Fry M, Hecht ST. Transient paralysis associated with epidural steroid injection. J Spinal Disord 1997; 10: 441-444. PMID: 9355063.


12. Chaudhari LS, Kop BR, Dhruva AJ. Paraplegia and epidural analgesia. Anaesthesia 1978; 33: 722-725. PMID: 717716.


13. Kwon MA, Park JH, Yoo RG, Kim TH, Sim WS. Benign and malignant tumors detected in the patients with intractable chest pain: 2 case reports. Korean J Pain 2005; 18: 255-258.

14. Lee HK, Shin DY, Lee HJ, Kim C. Intercostal neuralgia and spinal cord compression symptom due to spinal tumor: a case report. J Korean Pain Soc 1994; 7: 287-291.
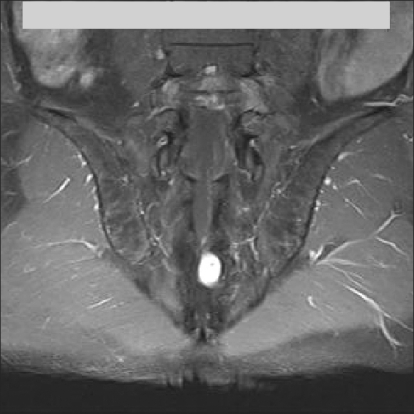
Fig. 1
T1-weighted MR sagittal image shows an isointense schwannoma with cauda equina compression at the S3 level.

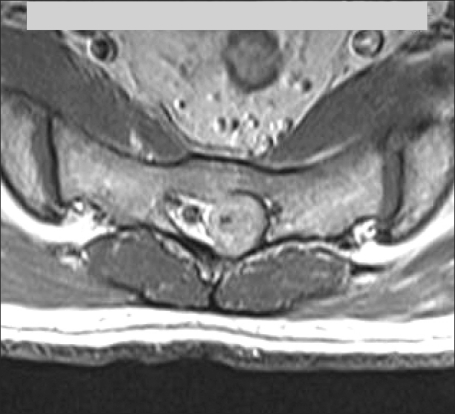
Fig. 2
T2-weighted MR sagittal image shows an isointense schwannoma with cauda equina compression at the S3 level.

- TOOLS