|
 |
|
|
Abstract
Tension pneumothorax during ventilating bronchoscopy for foreign body removal is a rare but life-threatening complication. The authors present a case of cardiac arrest caused by tension pneumothorax in a 9-month-old girl who underwent ventilating bronchoscopy for foreign body (peanut) removal. Tension pneumothorax was due to tracheobronchial lacerations caused by a bronchoscope. The patient was successfully resuscitated by cardiopulmonary resuscitation and chest tube insertion. The airway injury was effectively repaired by thoracotomy under extracorporeal membrane oxygenation.
Ventilating bronchoscopy is a useful means of removing a foreign body from the airway, an important, common cause of accidental death in childhood [1]. Many complications can occur during ventilating bronchoscopy [2], and tension pneumothorax during ventilating bronchoscopy is a rare but a life-threatening complication [3,4]. Early diagnosis and prompt management are essential for a good outcome. Therefore, tension pneumothorax caused by tracheal laceration should be ruled out when ventilation is impaired during anesthetic management for ventilating bronchoscopy [5]. We report a case of cardiac arrest induced by tension pneumothorax during ventilating bronchoscopy and anesthetic management for the repair of tracheal laceration under extracorporeal membrane oxygenation (ECMO).
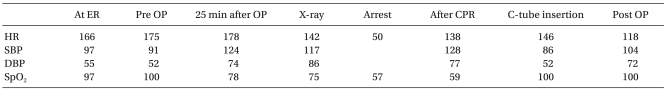
A 9-month-old, 10-kg girl without any relevant medical history was presented at our emergency room because she had aspirated a peanut 5 hours previously. Chest computed tomography showed a foreign body at the carina and the proximal right main bronchus, and emphysema in both lung fields (Fig. 1).
The patient was not premedicated. Anesthesia was induced intravenously with thiopental 60 mg and rocuronium 6 mg after administering atropine 0.2 mg. A rigid bronchoscope was inserted by an otolaryngologist after confirming adequate muscle relaxation. Anesthesia was maintained with 100% oxygen and sevoflurane.
Approximately 25 minutes after the start of the operation, SpO2 gradually decreased to 78% from 100%. Accordingly, the surgeon was asked to stop the procedure, and an uncuffed endotracheal tube (ID 4.0, Euromedical, Denmark) was intubated and fixed at 10 cm. Left lung sounds were heard clearly, but no right lung sounds were evident on auscultation. SpO2 did not improve despite manual ventilation with 100% O2 and an increased inspiratory pressure airway was detected. Accordingly, a simple chest radiograph was taken.
While waiting for the result of the chest radiograph, the otolaryngologist extubated the endotracheal tube and attempted to re-insert the rigid bronchoscope in order to check for possible causes of the airway obstruction, such as, residual foreign body. Meanwhile, the heart rate decreased to 50 beats/min, and SpO2 decreased to 57% (blood pressure was not measured). Atropine 0.2 mg and epinephrine 1 µg were injected intravenously, but vital signs did not improve and no carotid artery pulse was palpable. External cardiac compression was performed and epinephrine 10 µg was injected intravenously three times. Heart rate and blood pressure then recovered, and thus, cardiac compression was stopped. However, SpO2 did not improve (Table 1).
The simple chest radiograph revealed tension pneumothorax (Fig. 2). A chest tube was immediately inserted into the right thorax and a massive air leak was observed. At this time, the sounds of both lungs were clearly heard and SpO2 improved to 100%. Follow up chest radiography showed a significant reduction of the right tension pneumothorax and a scattering of subcutaneous emphysema at the left upper chest and around the neck (Fig. 3).
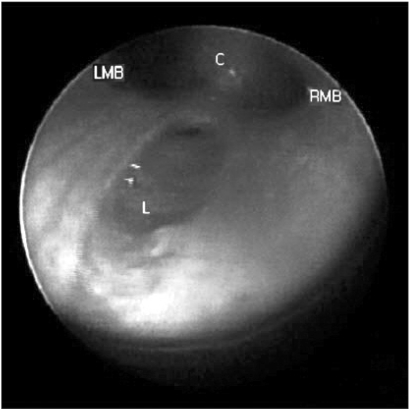
The tension pneumothorax suggested major tracheobronchial injury and a subsequent bronchoscopic examination revealed three major sites of laceration, one in the mid trachea of length 1.5 cm, a second in the distal trachea of length 2 cm (immediately above the carina) (Fig. 4), and a third in the right main bronchus of length 1 cm.
We decided to perform emergent primary closure of these sites via right thoracotomy. An arterial line was placed in the left radial artery to monitor blood pressure continuously. Arterial blood gas analysis showed; pH 7.10, PaCO2 63 mmHg, PaO2 77 mmHg, HCO3- 19.6 mmol/L at FiO2 1.0, ETCO2 24 mmHg, and SpO2 100%. After a rigid bronchoscope examination confirmed the absence of remaining foreign body, an uncuffed ID 4.5 endotracheal tube was inserted into the left main bronchus for single lung ventilation under fiberoptic bronchoscopic guidance. However, the patient did not tolerate single lung ventilation well and her SpO2 decreased to 79%. In view of the facilitation of surgical approach and the risks of hypoxemia and hypoventilation, ECMO was decided upon for respiratory support during the operation.
A central venous catheter was inserted into the left internal jugular vein. After 1,000 units of heparin was injected as a bolus, a 10 Fr catheter (Fem-Flex II Femoral cannula®, Edwards Lifesciences, Irvine, CA, USA) was placed in the right internal jugular vein for drainage, and a 12 Fr catheter was placed in the right femoral vein for perfusion using a sono-guided Seldinger technique (Fig. 5). ECMO flow was maintained at 0.7-0.8 L/min, and SpO2 remained at 98-100% without mechanical ventilation.
At the initiation of ECMO, fetanyl 5 µg/kg and midazolam 0.1 mg/kg were injected. Anesthesia was maintained with continuous intravenous infusions of sufentanil 5 µg/kg/h, midazolam 0.1 mg/kg/h, and vecuronium 0.1 mg/kg/h during ECMO. Dopamine was infused at 5 µg/kg/min and vital signs were stabilized. An activated clotting time (ACT) of approximately 200 seconds was maintained and arterial blood gas analysis under maximal ECMO support showed; pH 7.34, PaCO2 41 mmHg, PaO2 81 mmHg, and HCO3- 22.1 mmol/L at FiO2 1.0. When the ECMO flow rate reduced, it was recovered by pulling the cannula in the internal jugular vein slightly. Body temperature, measured using an oral thermometer, fell to as low as 35.0℃ after ECMO was initiated, and thus, a forced air warmer was applied to prevent further hypothermia. No significant bleeding problem was encountered during the procedure.
Total anesthesia time was 8 hr 25 min, estimated blood loss was 300 ml, and urine output was 120 ml; 250 ml of crystalloid solution and 1 unit of packed red blood cells were administered. ECMO was maintained postoperatively to minimize airway pressure. In the intensive care unit (ICU), the mechanical ventilation was performed using pressure control mode (inspiratory airway pressure 10 cmH2O, pressure support 11 cmH2O, respiratory rate 20/min, FiO2 0.5 and PEEP 3 cmH2O), which resulted in the expiratory tidal volume of 49 ml.
Vital signs were stable in the ICU, and the patient awoke with no signs of respiratory or neurologic deficit on the first postoperative day. Electroencephalography (EEG) showed no significant abnormality. The patient was subsequently weaned from ECMO first postoperative day. The simple chest radiograph taken in the ICU showed reduced subcutaneous emphysema and no residual pneumothorax. The patient was discharged on the sixth postoperative day.
Ventilating bronchoscopy has the risk of severe complications, such as, infection, laryngeal edema, laryngospasm, bronchospasm, bleeding, hypoxia, pneumomediastinum, and pneumothorax [2]. Tension pneumothorax is a rare but life-threatening complication [3,4]. Rothmann and Boeckman [6] reported that the probability of pneumothorax during rigid bronchoscopy for the removal of a foreign body is approximately 1%. Therefore, the possibility of pneumothorax should be suspected when ventilation worsens during ventilating bronchoscopy [7]. However, an early diagnosis of pneumothorax during anesthesia is not easy because the symptom is masked by anesthesia [5]. Tension pneumothorax during surgery may manifest as a reduction in oxygen saturation, a rapid increase in airway pressure, hypotension, and/or tachycardia [8]. In this case, airway lacerations caused by the bronchoscope were responsible for the tension pneumothorax.
The reasons for the delayed diagnosis in the present case were that the reduction in oxygen saturation and the diminished right lung sounds were mistakenly attributed to airway obstruction by a foreign body. Pneumothorax might have been diagnosed earlier if excessive resonance had been confirmed by percussion. In addition, if lung sounds had been checked more carefully, it might have been easier to determine whether the respiratory failure was due to foreign body obstruction or tension pneumothorax. Furthermore, it would have been safer to evaluate airway with a fiberoptic bronchoscope inserted through the endotracheal tube under ventilation rather than attempt airway assessment using a ventilating bronchoscope after extubation.
During surgery on the trachea and bronchus, a double lumen endotracheal tube or a univent tube may be appropriate for adults and older children. However, in small children, because conventional single lung ventilation methods are likely to fail to maintain adequate ventilation and oxygenation, the elective application of ECMO may be a good option [9]. ECMO was also useful during the postoperative course in the described case because it can minimize inspiratory airway pressure during mechanical ventilation.
During ECMO, heparin was administered as a single bolus of 100 unit/kg followed by continuous intravenous infusion at 20-60 unit/kg/min [10]. Anticoagulation was accomplished by titrating heparin administration to maintain an ACT of between 180 and 220 seconds [10]. Furthermore, levels of blood anticoagulation were monitored hourly, and the amount of heparin administered was carefully controlled to prevent bleeding complications.
In addition, because the ECMO machine was not equipped with a sevoflurane vaporizer and almost no mechanical ventilation was performed during ECMO, intravenous opioids and midazolam were added for anesthesia.
Summarizing, the tension pneumothorax should be considered when inspiratory pressure is increased and oxygen saturation is decreased during ventilating bronchoscopy. Effective communication between the operator and anesthesiologist is essential when unexpected complications are encountered to facilitate the prompt planning of coping strategies.
References
1. Steen KH, Zimmermann T. Tracheobronchial aspiration of foreign bodies in children: a study of 94 cases. Laryngoscope 1990; 100: 525-530. PMID: 2329912.


2. Hasdiraz L, Oguzkaya F, Bilgin M, Bicer C. Complications of bronchoscopy for foreign body removal: experience in 1,035 cases. Ann Saudi Med 2006; 26: 283-287. PMID: 16883083.



3. Harar RP, Pratap R, Chadha N, Tolley N. Bilateral tension pneumothorax following rigid bronchoscopy: a report of an epignathus in a newborn delivered by the EXIT procedure with a fatal outcome. J Laryngol Otol 2005; 119: 400-402. PMID: 15949108.


4. Gallagher MJ, Muller BJ. Tension pneumothorax during pediatric bronchoscopy. Anesthesiology 1981; 55: 685-686. PMID: 7305058.


5. Baumann MH, Sahn SA. Tension pneumothorax: diagnostic and therapeutic pitfalls. Crit Care Med 1993; 21: 177-179. PMID: 8428465.


6. Rothmann BF, Boeckman CR. Foreign bodies in the larynx and tracheobronchial tree in children: a review of 225 cases. Ann Otol Rhinol Laryngol 1980; 89: 434-436. PMID: 7436247.


7. Ibrahim AE, Stanwood PL, Freund PR. Pneumothorax and systemic air embolism during positive-pressure ventilation. Anesthesiology 1999; 90: 1479-1481. PMID: 10319799.


8. Hunter AR. Problems of anaesthesia in artificial pneumothorax. Proc R Soc Med 1955; 48: 765-768. PMID: 13266824.



9. Skinner SC, Hirschl RB, Bartlett RH. Extracorporeal life support. Semin Pediatr Surg 2006; 15: 242-250. PMID: 17055954.


10. Sohn YS. ECMO in pediatric population. J Korean Pediatr Cardiol Soc 2004; 8: 44-51.
Fig. 1
Preoperative chest computed tomography (CT). Preoperative chest CT scan shows a foreign body in the carina and right proximal main bronchus.
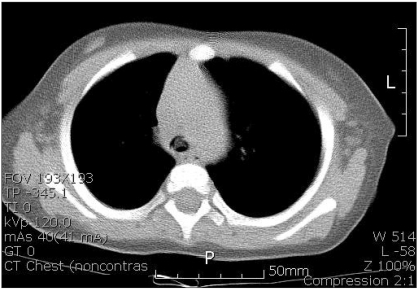
Fig. 2
Tension pneumothorax. Intraoperative chest simple radiograph shows right pneumothorax with total right lung collapse and mediastinal shift. Pneumomediastinum and diffuse subcutaneous emphysema are also evident at the neck and upper chest wall. The stomach is severely distended and the liver displace to the inferior, left side.

Fig. 3
Chest radiograph after chest tube insertion. A chest tube is inserted in the right thorax, and the size of the pneumothorax decreases. The radiograph shows retroperitoneal air collection with subcutaneous emphysema at the left chest wall and in the neck region.

Fig. 4
Laceration of the trachea. The posterior portion of the trachea is lacerated longitudinally just above the carnina. RMB: right main bronchus, C: carina, LMB: left main bronchus, L: lacerated site in carina.
- TOOLS