 |
 |
| Korean J Anesthesiol > Volume 73(3); 2020 > Article |
|
Abstract
Background
Blood component mistransfusion is generally due to preventable clerical errors, specifically pretransfusion misidentification of patient/blood unit at bedside. Hence, electronic devices such as barcode scanners are recommended as the standard instrument used to check the patientŌĆÖs identity. However, several healthcare facilities in underdeveloped countries cannot afford this instrument; hence, they usually perform subjective visual assessment to check the patientŌĆÖs identity. This type of assessment is prone to clinical errors, which precipitates significant level of anxiety in the healthcare personnel transfusing the blood unit. Hence, a novel objective method in performing pretransfusion identity check, the ŌĆśSandesh Positive-Negative (SPON) protocol,ŌĆÖ was developed.
Methods
A nonrandomized study on bedside pretransfusion identity check was conducted, and 75 health care personnel performed transfusion. The intervention was performed by matching a custom-made negative label with blood component with the positive label of the same patient available at bedside who was about to receive transfusion.
Results
In total, 85.3% of the subjects were anxious while performing pretransfusion identity check based on the existing standard practice. After the implementation of the SPON protocol, only 38.7% experienced either mild, moderate or severe anxiety. The overall level of satisfaction also increased from 8.0% to 38.7% and none were dissatisfied. Although only 9.3% were dissatisfied about the existing practice, approximately 70.7% felt the need for a better/additional protocol. Clerical error was not observed.
Transfusion of blood and its components occasionally results in serious hemolytic reactions due to the transfusion of wrong blood type, which is considered a human clerical error. This type of error may occur at the initial stages of blood collection, labeling, grouping, and transportation, or more importantly, this error may possibly be observed when a healthcare personnel fails to perform final bedside identity check between the patient and blood component unit before transfusion. The World Health Organization has established several policies and guidelines for a safe blood transfusion [1].
Pretransfusion final identity check, which ensures the transfusion of the right unit for the right patient, is best achieved by using various electronic transfusion management systems [2ŌĆō5]. However, in healthcare facilities that cannot afford these expensive instruments, identity check is performed by the healthcare personnel initiating the transfusion (transfusionist) by visually matching patientŌĆÖs details available at bedside with the compatibility label attached to the blood component unit and transfusion prescription [1,6]. This is a subjective and self-confirmatory method performed based on the transfusionistŌĆÖs subjective clinical assessment. Occasionally, clerical errors due to stress, increased workload, or mere negligence during this process, resulting in fatal and legal consequences, can be observed. Hence, the transfusionist may experience a significant level of anxiety. Therefore, the use of a cost-effective objective method would be beneficial. Hence, a novel ŌĆśSandesh Positive-Negative (SPON) protocolŌĆÖ for checking the patientŌĆÖs identity with the blood components before transfusion was developed and evaluated.
This study aimed to compare the SPON protocol with the standard protocol for the final identity check of blood components at bedside to ensure the transfusion of the right blood unit for the right patient. The primary study hypothesis was to compare the two protocols with respect to the transfusionistsŌĆÖ anxiety and satisfaction levels. The secondary hypothesis was to observe the chances of avoidable clerical errors/near-miss events of mismatched transfusion. Hence, a novel negative label was created that would match with the characters of a positive label only if it belonged to the same patient.
This study was approved by the Kasturba Medical College and Hospital Institutional Ethics Committee (IEC-457/2017). The study was also registered in the Clinical Trial Registry of India (CTRI/2017/10/010002 [Registered on 04/10/2017], principal investigator ŌĆō Dr. Sandesh U). All subjects provided written informed consent for inclusion in the study. Subjects with the following characteristics were included in the study: (a) a healthcare personnel authorized to perform blood component transfusion (if required for the patient as advised by the consultant doctor) and (b) who had performed at least 50 transfusions earlier in his/her healthcare profession. A total of 75 subjects were enrolled in the study. They were further divided into 3 groups of 25 based on their job profile: (1) doctors/consultant anesthesiologists, (2) postgraduate students of anesthesiology and intensive care, and (3) nurses. The procedure in the SPON protocol was explained and also demonstrated with hands-on training experience by allowing them to perform the procedure using sample labels. The procedure was demonstrated several times until each of the subjects had completely and accurately performed the protocol.
The blood component unit arrives at the site of transfusion along with the compatibility report and label. At bedside, initially, the transfusionist visually matches the blood unit with the compatibility label and report and subsequently further matches all of these with the patientŌĆÖs details (present on the patientŌĆÖs wristband/and patientŌĆÖs hospital records). Once all the details are matched and the blood component is considered as the ŌĆśright unitŌĆÖ for the ŌĆśright patient,ŌĆÖ the transfusionist affixes his/her signature on the compatibility form confirming that the identity check is properly performed. Furthermore, this entire process executed by the transfusionist is cross-checked by another personnel (termed ŌĆśdouble checkŌĆÖ), and after the cross-checking, the transfusion is initiated.
It basically comprises matching two labels having patientŌĆÖs details at bedside of a patient who is about to receive transfusion. The protocol consists of the following components (Fig. 1):
Typically, each patient admitted to any hospital is provided with a distinctive label for identification with details regarding the patientŌĆÖs name, age, gender, ward, hospital unique identification number, and other details. The positive label is the similar label that is available at the patientŌĆÖs bedside at the site of transfusion (Fig. 1A, a).
It is a custom-made label with four rectangular punched-out spaces/gaps (Fig. 1A, b). It has exactly similar dimensions as that of the positive label. In this label, patient details similar to the positive label could be printed. Hence, when patient details are printed on this negative label, due to gaps, some of the characters corresponding to these gaps will not be printed. The unprinted/blank negative label is made available at the blood bank so that when a request for blood or its component unit is received, patientŌĆÖs details are printed on the negative label concurrently along with the routinely printed compatibility label and compatibility report using an integrated software program.
It is a customized label strip that has places to paste two labels and affix a signature (Fig. 1A, c).
The positive and negative labels, label strip, and compatibility label are all sticky labels that can be peeled off and pasted on to another surface.
Hence, the blood component is sent to the site of transfusion along with the negative label, SPON label strip, compatibility report, and compatibility label.
At the site of transfusion, upon receipt of blood component with the abovementioned items, the transfusionist initially performs the standard protocol; subsequently, the SPON protocol is performed.
Step 1: Two positive labels that are available near the patient are pasted on spaces provided in SPON label strip (Fig. 1).
Step 2: Subsequently, the negative label is peeled off, aligned correctly on top of one of the positive labels, and pasted over it. This now forms the combined positive-negative (P-N) label (Fig. 2). The gaps in the negative label will be filled by characters from the underlying positive label. Hence, the characters in the combined P-N label form a continuum by characters partly from the negative label and remaining from the underlying positive label (corresponding to the gaps in the negative label). This continuum of characters will be accurate and comprehensible only when both the negative label on top and underlying positive label belong to the same patient.
Step 3: The combined P-N label is further compared with the adjacent second positive label and ensured that both P-N label and second positive label match exactly with each other. This is again possible only if both the positive and negative labels belong to the same patient (Fig. 2).
Step 4: Subsequently, the transfusionist affixes his/her signature in the space provided in the label strip to confirm the authenticity of the properly performed SPON protocol. The negative label can also be made light colored, which makes its characters in the combined P-N label stand out and aid in better comparability.
Step 5: Furthermore, the whole SPON label strip containing the combined P-N label, positive label, and signature is attached to the patientŌĆÖs record file for future reference.
After completing these steps, the transfusion is initiated.
The transfusionist subsequently answered a written questionnaire about performing a new protocol, and the results were interpreted based on their responses. The questionnaire included the following parameters: anxiety about blood transfusion, reason for anxiety, satisfaction about the existing standard protocol, need for new protocol, difficulty and workload in performing the new protocol, and the anxiety and satisfaction after the implementation of the new protocol. Anxiety level was measured based on the perception of anxiety by the transfusionists as none, mild, moderate, or severe. Satisfaction levels were assessed based on the perception of satisfaction as dissatisfied, satisfied, and highly satisfied.
In addition to the above parameters, the following were also noted: (a) number of times identity check was performed with anxiety about the existing protocol, which was quantified as either once or twice and several times; (b) whether the transfusionists properly performed the identity check as cross-checked by another personnel (double checking) after their initial safety check; (c) number of near-miss events that occurred in a transfusionistŌĆÖs profession earlier (ŌĆśnear-missŌĆÖ events were considered errors that could result in the transfusion of an incorrect blood component if left undetected, but these errors were recognized before the transfusion was performed [7]); (d) amount of workload perceived by the transfusionist while performing the new protocol, quantifiable as nothing, manageable/minimal, moderate, or excessive extra work; and (e) whether the new protocol was considered worthy and whether it would be recommended for future implementation on a standard basis.
It is further emphasized that the SPON protocol was performed in addition to and after the standard protocol. This was performed on purpose because bypassing the existing standard protocol would have raised serious questions about ethical issues and patient safety as the new protocol was experimental and was being implemented for the first time.
Anticipating 47% discordant pairs in anxiety and satisfaction before and after the implementation of the new protocol, with 95% confidence level and a power of 80%, a minimum of 68 subjects were required in this study. Hence, 75 subjects who met the inclusion criteria were enrolled in this study.
Data was summarized using descriptive statistics. Comparisons before and after the implementation of the new protocol were performed using McNemarŌĆÖs test and the chi-squared tests. A P value of < 0.05 was considered statistically significant. Data were analyzed using the Statistical Package for the Social Sciences (SPSS) software version 15 (SPSS South Asia, India).
A total of 85.3% (64/75) of the subjects were anxious about the process of blood transfusion with reference to the existing standard protocol used to check patientŌĆÖs identity (Table 1) due to fear of complications of mistransfusion. Moreover, in their professional career, 72.0% (54/75) of the transfusionists had near-miss events at least once, 14.7% (11) twice, and 13.3% (10) three or several times. Furthermore, the identity check of approximately 64.0% did not undergo cross-examination by a second personnel (double checking). Hence, approximately 69.3% (52/75) themselves performed the identity check twice or several times. Moreover, although only 9.3% (7/75) were dissatisfied about the existing protocol, approximately 70.7% (53) felt the need for a new/better or an additional protocol. After the implementation of the SPON protocol, only 38.7% (29/75) experienced any degree of anxiety (P = 0.001 in consultants, P = 0.001 in trainees, P = 0.012 in nurses). However, in total subjects, there are no differences with respect to the distribution of anxiety levels. The proportion of subjects being highly satisfied increasing from 8.0% to 38.7% (P = 0.011), and none of them were dissatisfied (Table 1). Additionally, 48.0% felt minimal but manageable extra work in performing the protocol. Moreover, 84.0% (63/75) considered the new protocol worthy, and 89.3% (67/75) recommended for its implementation on a regular basis (Table 2). None of the subjects had experienced difficulty in performing the protocol, and clerical error was not observed during the study.
Transfusion of blood and its components is a complex multistep process involving several diverse healthcare professionals, namely, doctors, laboratory technologists, and nurses apart from donors and recipients. Accordingly, errors can occur during any of these steps starting from the initial stages of blood collection until transfusion, causing fatal complications. Contributory causes for these errors are mostly due to the widely recognized ŌĆśhuman factorsŌĆÖ such as increased workload, slips and lapses, fatigue, lack of attention, and taking shortcuts and omission of essential steps [7]. Patients are at a higher risk of a wrong blood transfusion than any other transfusion-related complications [8,9]. This type of error is frequently observed at the patientŌĆÖs bedside just prior to the transfusion due to inappropriate identity check [10ŌĆō13]. Similarly, in hospital areas requiring many blood components (e.g., large-sized wards, intensive care units [ICUs], and where several operating rooms are situated in one complex), the number of components arriving is significantly higher compared to hospital areas not requiring blood components. Often, they may have been ordered and expected simultaneously at close intervals for two or more patients positioned nearby. Hence, there are chances that the healthcare personnel transporting them may accidently deliver it to the wrong operating room/ward, probably leading to mistransfusion.
These potentially serious errors can nearly be eliminated by removing the manual steps/human factors and introducing certain tools, for example, patient identification bracelets with barcodes and barcode readers, radio-frequency identification devices, automated analyzers in laboratories, or mechanical and electronic locks that provide safe end-to-end electronic control across the whole transfusion process [3,4,5,10]. However, in healthcare facilities that cannot afford these expensive instruments, the standard method of identity check is performed by the transfusionist by visually matching the patientŌĆÖs details with the compatibility report and compatibility label (attached on the blood component) [1]. This process is completely subjective as it is solely based on the transfusionistŌĆÖs assessment; as a result, the transfusionist may perform the identity check more than once. Moreover, considering that the procedure is purely subjective, clerical errors are significantly possible due to various factors described earlier. Occasionally, the compatibility label is only matched with the compatibility report and is not matched with the patientŌĆÖs identity details on the wristband or at bedside. Considering that both the compatibility label and report are generated by the same laboratory computer, the two will always match even if wrong blood component is being transfused. All these factors result in a significant level of anxiety and dissatisfaction in the transfusionist. Hence, to address the need for an objective method that is not only practical and simple but also inexpensive, the SPON protocol was developed and evaluated.
Most of the transfusionists were anxious about the process of transfusion with the existing standard protocol (Table 1). The major reason for this anxiety was the fear of mistransfusion due to judgmental errors. The most common anticipated serious consequences of these errors were the fear of losing the patientŌĆÖs life (44.0%) and legal consequences (30.7%). Awareness regarding legal complications was more common in consultants than in postgraduate students and nurses. Due to the significant level of anxiety regarding clerical errors, approximately 69.3% of the subjects admitted having performed the identity check twice or several times. Moreover, although cross-examination of the identity checked by a second personnel (double check) was recommended and considered as part of the standard procedure, the identity check of approximately 64.0% (48/75) of the transfusionists did not undergo cross-examination. The common reason for this was the lack of healthcare personnel available at the time of cross-examination. Furthermore, evidence regarding the safety of performing bedside check by one or two healthcare staff does not exist [6]. Hence, 70.7% (53/75) felt the need for a new/better or an additional protocol for identity check.
The P-N label works based on the lock and key principle where only a unique key would fit into the respective keyhole of its corresponding lock to unlock it. In the SPON protocol, the P-N label is a proof of compatibility as the negative label will match with its corresponding positive label only if it belongs to the same patient. Although most of the steps in the SPON protocol are objective, the final step requires visual confirmation and judgment. Even then, it is significantly easier to determine any disparity between the positive and combined P-N label as they both lie adjacent to each other (Fig. 2). It is easier to compare thetwo items precisely when placed nearby rather than farther away. After the implementation of the protocol, the proportions of the transfusionists who rated the anxiety as mild, moderate, or severe decreased considerably from 85.3% to only 38.7%. Moreover, none of the subjects were dissatisfied with an overall increase in satisfaction levels.
Adding an extra phase to an existing protocol seemed to increase the transfusionistsŌĆÖ workload as 48% felt that the new protocol added extra, but minimal and manageable, work. Nevertheless, 84% felt that the extra effort was absolutely worthwhile (Table 2). They believed that the benefits of this minimal extra effort outweigh far greater than the consequences of a mistransfusion with respect to mortality and legal concerns. The SPON protocol was proven to be simple and easily comprehensible since none of the subjects had experienced difficulty in performing the protocol.
Clerical errors were not observed during the study probably because the overall incidence of clerical errors has drastically decreased over the years due to the comprehensive reporting of incidents and implementation of standard policies and the subjects were extra vigilant due to their conscious enrolment in the study. However, approximately 28% (21) reported to have experienced near-miss events in their profession more than once, causing a significant level of anxiety. ŌĆśNear-missŌĆÖ events comprise a third of all SHOT reports, which was comparable to our study [7,14]. These were mainly observed in the ICU/general ward where blood components were erroneously placed near a different patient or in a common area. It was also noted that although those events were promptly avoided with the existing standard protocol itself, the subjects felt that a new protocol would have reduced the anxiety they experienced during those events. Hence, although the SPON protocol may be comparable to the standard protocol in terms of avoiding clerical errors, it is absolutely superior in terms of reducing anxiety and improving satisfaction levels. Therefore, most of the subjects recommended the protocol for implementation on a standard basis.
Traditional double checking performed by two medical personnel is also considered a subjective way that is dependent on the assessment of the second personnel; hence, when double checking is performed, objective confirmation is not provided. Hence, the SPON protocol performed by one transfusionist may provide an objective confirmation over traditional double checking. However, an adverse effect as a result of the omission of the standard double checking can be possibly observed, leading to errors and ethical concerns. Hence, the SPON protocol would yield superior results if used as an additional rather than a replacement method to the existing standard method, which also formed the basis for designing this study.
However, the study had the following limitations. First, the study could not be conducted as a randomized cross-over study to avoid the significant period effect and carryover effect. Second, this study comprised a small sample size; hence, clerical errors were not clearly evaluated considering that the estimation of errors required a large sample size (in this study, the incidence of clerical errors was significantly low even with the existing standard protocol). Furthermore, the implementation of any new method on a large scale involves ethical issues, specifically if it involves errors leading to significant morbidity. Third, clerical errors were not observed in the present study sample, which is possibly due to the conscious enrolment of subjects for the new protocol; hence, the subjects were extra vigilant.
The SPON protocol is more confirmatory than the existing protocol due to its dual subjective and objective nature indicating the right blood for the right patient. Importantly, evidence regarding the appropriate performance of identity check exists as the final label strip is attached to the patientŌĆÖs hospital record file. This is considered beneficial in addressing possible medicolegal concerns or litigations in the future as erroneous transfusion amounts to medical negligence, resulting in punishment and warranting huge monetary compensation. Moreover, the cost of this additional protocol per patient was estimated to be merely 0.4 Indian National rupee/0.0058 US dollar/0.0044 Pound Sterling [15]. Since it does not require any additional infrastructure and manpower, it can be easily implemented and possibly be incorporated as a standard operating protocol for safe transfusion by regulatory authorities specifically in Third World countries. It can also be a major database used in the hemovigilance systems of any country [9].
Therefore, the ŌĆśSPON protocolŌĆÖ is a simple and cost-effective objective method when performing final bedside identity check of blood components for an improved transfusion practice.
Acknowledgments
The authors acknowledge the cooperation from the Departments of Transfusion Medicine and Information Systems of Kasturba Medical College and Hospital, Manipal, Karnataka, India. The Transfusion Medicine Department contributed to the organization of label printing. The Department of Information Systems contributed to the integration of computer software.
NOTES
Author Contributions
Sandesh Udupi (Conceptualization; Formal analysis; Investigation; Methodology; Supervision; Writing ŌĆō original draft; Writing ŌĆō review & editing)
Kriti Puri (Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Validation; Writing ŌĆō original draft; Writing ŌĆō review & editing)
Fig.┬Ā1.
Components of Sandesh Positive-Negative (SPON) protocol. (A) a: Positive label, b: negative label, and c: SPON label strip. (B) Pasting the second positive label on the SPON label strip.
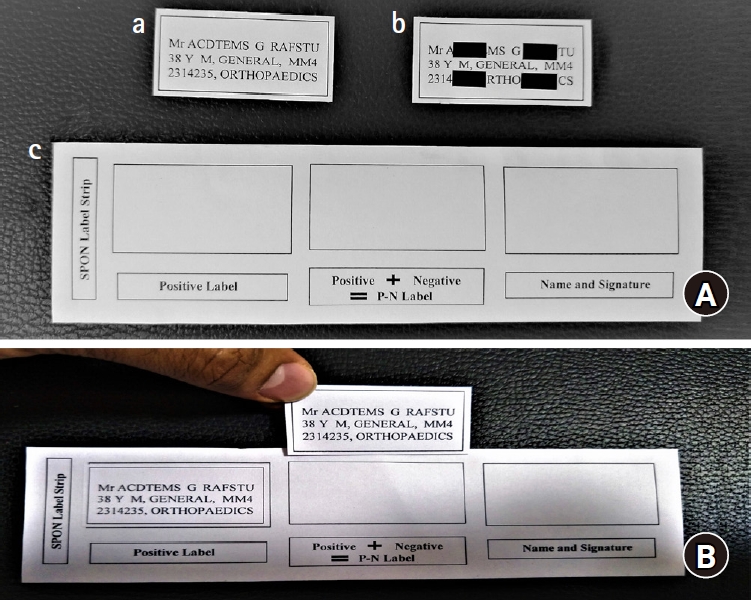
Fig.┬Ā2.
Steps of SPON protocol. (A) Process of alignment of the negative label on top of the positive label. (B) The Sandesh Positive-Negative label strip with the positive label, combined positivenegative label, and signature.

Table┬Ā1.
Table Showing Anxiety and Satisfaction Levels before and after the Implementation of the New Protocol
Table┬Ā2.
SubjectsŌĆÖ Opinion regarding Extra Work, Worthiness, and Recommendation about the New Protocol
References
1. World Health Oranization. Blood transfusion safety: Safe and rational clinical use of blood [Internet]. Geneva: WHO [cited 2019 Jun 8]. Available from https://www.who.int/bloodsafety/clinical_use/en/Handbook_EN.pdf
2. Joint United Kingdom (UK) Blood Transfusion and Tissue Transplantation Services Professional Advisory Committee. Transfusion Guidelines: Safe transfusion ŌĆō right blood, right patient, right time and right place [Internet]. UK: JPAC [cited 2019, Jun 8]. Available from https://www.transfusionguidelines.org/transfusion-handbook/4-safe-transfusion-right-blood-right-patient-right-time-and-right-place
3. Davies A, Staves J, Kay J, Casbard A, Murphy M. End-to-end electronic control of the hospital transfusion process to increase the safety of blood transfusion: strengths and weaknesses. Transfusion 2006; 46: 352-64.


4. Murphy M, Kay J. Barcode identification for transfusion safety. Curr Opin Hematol 2004; 11: 334-8.


5. Turner C, Casbard A, Murphy M. Barcode technology: its role in increasing the safety of blood transfusion. Transfusion 2003; 43: 1200-9.


6. Joint United Kingdom (UK) Blood Transfusion and Tissue Transplantation Services Professional Advisory Committee. Transfusion Administration to the patient [Internet]. UK: JPAC [cited 2019, Jun 8]. Available from https://www.transfusionguidelines.org/transfusion-handbook/4-safe-transfusion-right-blood-right-patient-right-time-and-right-place/4-10-administration-to-the-patient
7. Bolton-Maggs P, Cohen H. Serious Hazards of Transfusion (SHOT) haemovigilance and progress is improving transfusion safety. Br J Haematol 2013; 163: 303-14.



8. Serious Hazards of Transfusion [Internet]. Manchester: SHOT [cited 2019 Jun 8]. Available from https://www.shotuk.org/
9. International Haemovigilance Network. [Internet]. Leiden [cited 2019 Jun 8]. Available from https://www.ihn-org.com/
11. Serious Hazards of Transfusion. Report and Summary 2003 [Internet]. Manchester: SHOT [cited 2019 Jun 8]. Available from. Accessed https://www.shotuk.org/shot-reports/reports-and-summaries-2003/
12. Callum J, Kaplan H, Merkley L, Pinkerton PH, Rabin Fastman B, Romans RA, et al. Reporting of near-miss events for transfusion medicine: improving transfusion safety. Transfusion 2001; 41: 1204-11.


13. Dzik W, Murphy M, Andreu G, Heddle N, Hogman C, Kekomaki R, et al. An international study of the performance of sample collection from patients. Vox Sang 2003; 85: 40-7.


14. Serious Hazards of Transfusion. Annual Shot Report 2012 [Internet]. Manchester: SHOT [cited 2019 Jun 8]. Available from https://www.shotuk.org/wp-content/uploads/myimages/SHOT-Annual-Report-20121.pdf
15. Xe Money Transfer. XE Currency Converter - Live Rates [Internet]. Newmarket: Xe Money Transfer [cited 2019 Apr 8]. Available from https://www.xe.com/currencyconverter/









