 |
 |
| Korean J Anesthesiol > Volume 72(5); 2019 > Article |
|
Abstract
Background
This study aimed to determine the optimal location of local anesthetic injection in the interspace between the popliteal artery and posterior capsule of the knee (iPACK), using the anatomical pattern of the articular branch of tibial nerve (ABTN). We hypothesized that injection at the level of ABTN forming a popliteal plexus would mainly spread throughout the popliteal fossa without contacting the tibial or peroneal nerves.
Methods
The anatomical study included 30 soft cadavers. Ultrasound-guided dye injection was performed in legs of 10 cadavers after identifying the position of the ABTN and surrounding structures, followed by dissection to assess its spread. Clinical study was conducted in 15 patients undergoing total knee arthroplasty (TKA) with ultrasound-guided injection in the iPACK. All patients also received continuous adductor canal block. Sensorimotor function of the tibial and common peroneal nerves was determined.
Results
In the distal portion of the popliteal fossa, the tibial nerve and popliteal vessels ran superficially and closely together. The trajectory of ABTN ran lateral to the popliteal vasculature, forming a plexus towards the posterior capsule of the knee below the medial side of the upper edge of lateral femoral condyle. In cadavers, the ABTN and surrounding area of the popliteal plexus were stained with dye after injection. In the clinical study, no patients experienced complete motor or sensory blocks.
The aim of the postoperative analgesics prescribed for total knee arthroplasty (TKA) is to provide adequate pain relief, as well as minimize opioid consumption and enhance rehabilitation [1,2]. It can be a challenge to administer peripheral nerve blocks (PNBs) with other multimodal analgesia methods to provide effective pain relief, while preserving muscle strength for rehabilitation. A recent study found that multiple PNBs, especially when combined with femoral and sciatic nerve blocks (SCB), were more effective in pain relief and physical performance than single PNBs [3]. Therefore, blockade of peripheral nerves that only innervate some parts of the knee does not provide sufficient analgesia in TKA. However, both femoral and SCB may result in muscle weakness and delayed ambulation [4,5]. Tibial nerve block (TNB) may provide sensory analgesia in the posterior aspect of the knee, similar to that of the SCB, without resulting in dorsiflexion motor deficits from common peroneal nerve paralysis. On the other hand, several studies found that the blockade of the common peroneal nerve remains to be determined and could result in delayed rehabilitation [6–8].
The sensory innervations of the posterior aspect of the knee are by the articular branch of the tibial nerve (ABTN), with variable contributions from the posterior branch of the obturator nerve [9]. These branches are delineated as a plexus, which is closely associated with the popliteal vessels at the level of the popliteal fossa. Hence, blockade of the ABTN that forms a popliteal plexus can be used to provide posterior knee analgesia without motor weakness. Recent studies have shown the efficacy of local anesthetic injection into the interspace between the popliteal artery and posterior capsule of the knee (iPACK) and popliteal plexus block (PPB) [10–13] to block the ABTN, common peroneal, and/or obturator nerves in the popliteal region as part of the multimodal regimens for posterior knee analgesia after TKA. For the iPACK, the target of the needle injection point is the level of the femoral shaft adjoining the femoral condyle, or approximately 1–2 fingers’ breadth above the patella. However, there has been a lack of studies exploring relevant neuroanatomy, and the optimal level of injection in the iPACK. Moreover, no prior studies have fully investigated the location of the ABTN and popliteal plexus in the popliteal fossa or its anatomical pathway prior to its entry into the knee capsule.
The objective of this study was to determine the optimal location of iPACK injection by using the anatomical pattern of the ABTN in a cadaver model. We hypothesized that injection at the level of the ABTN forming the popliteal plexus would spread mainly throughout the popliteal fossa without contacting the tibial or common peroneal nerves.
We conducted this observational descriptive study at the King Chulalongkorn Memorial Hospital, Bangkok, Thailand between July and December 2018. This study was approved by the Institutional Review Board of Chulalongkorn University, Bangkok, Thailand in February 2018 (Ref: 475/61), and is registered with clinicaltrials.in.th (TCTR20180728001). This study was divided into two stages: first, a cadaveric dissection was performed to evaluate the anatomical pathway of the ABTN in the popliteal fossa, and determine the optimal location of the ultrasound-guided iPACK technique; second, the efficacy of this technique for inducing PNBs was evaluated in patients undergoing TKA.
We selected 30 embalmed human cadavers (12 males, 18 females; aged 18 years or older), donated for scientific research at the Department of Anatomy, Chulalongkorn University, to determine the passage of ABTN in the popliteal fossa. None of the cadavers had any history of congenital defects, major procedures, or surgery in lower extremities. To avoid selection bias, each cadaver underwent one dissection on either side of one leg according to a computer-generated randomization list created by an independent researcher.
All cadavers were placed in the prone position and a longitudinal incision was made in the midline of the posterior thigh from the gluteal region to upper leg, followed by transverse incisions at the popliteal crease level. After removal of the skin and subcutaneous tissue, the boundaries of the popliteal fossa were demarcated by the superolateral, superomedial, and inferior limits, which were defined by the biceps femoris muscle, semimembranosus and semitendinosus muscles, and plantaris and two heads of the gastrocnemius muscle, respectively. Dissection of fat and local fascia was then performed, while preserving the nerve’s original position. When bifurcation of the sciatic nerve was clearly identified at the fossa level or thigh, the pathway of the tibial nerve was observed. Further dissection following the pathway of the articular and muscular branches of the tibial nerve was done until a plexus close to the popliteal vessels was observed either reaching the knee capsule (the articular branch) or into the surrounding muscle (the muscular branch). The anatomical structures located closest to the ABTN and nearest to the capsule of the knee were identified, in order to determine the position of the ultrasound probe and needle injection.
To verify the accuracy of the ultrasound-guided procedure, we injected 8 ml of methylene blue (1%) using a 100-mm insulated nerve block needle (Stimuplex A, 22 Ga. x 4 in., B Braun, Germany) into the other non-dissected legs of 10 cadavers. Ultrasound-guided injections were performed using a high-frequency linear ultrasound transducer (Sonosite X-Porte 13-MHz, HFL38x, Sonosite Inc., USA) by one of the authors (W.K.), who was skilled in ultrasound-guided nerve blocks. A similar dissection technique was performed immediately after the injection to determine the spread of dye. The successful spread of dye was defined as blue coloring of the distal part of the popliteal fossa within the ABTN and popliteal artery and vein.
In total, 15 patients (3 males, 12 females) who underwent the first elective TKA case of the day at the King Chulalongkorn Memorial Hospital participated in this study. All participants were between 18–80 years of age, with an American Society of Anesthesiologists functional status of I to III, and body mass index between 18–40 kg/m2. Exclusion criteria were allergy to any drug administered in the study, any contraindication to neuraxial anesthesia, intolerance to non-steroidal anti-inflammatory drugs, and chronic opioid drug use (daily or almost daily use of opioid drugs for ≥ 3 months, morphine use ≥ 60 mg/day for ≥ 1 month, or diagnosis of neuropathic pain). Written informed consent was obtained from all patients.
In a block room, patients were placed in the prone position with the high-frequency linear ultrasound transducer (Sonosite X-Porte 13- MHz, HFL38x, Sonosite Inc., USA) oriented transversely at the popliteal fossa level. The injection position for ultrasound-guided iPACK was based on the landmarks for the ABTN forming the popliteal plexus as defined by the anatomical study. Lidocaine (2 ml, 1%) was infiltrated at the needle injection point before a 100-mm insulated nerve block needle (Stimuplex-A, 22 Ga. x 4 in., B Braun, Germany) was inserted in the lateral-to-medial direction using an in-plane approach. A mixed solution of 0.25% levobupivacaine with 1 : 200,000 epinephrine (20 ml) was prepared, of which 5 ml was injected first at the lateral borders of the popliteal artery and remaining 15 ml was incrementally injected in the area between the popliteal artery and posterior capsule of the knee at the same level. After 30 minutes, sensation in the tibial and common peroneal nerves was assessed by comparing the loss of cold and light touch sensations on the plantar and dorsal aspects of the operative and non-operative feet using a 3-point scale (0 = normal; 1 = absent cold perception but intact touch sensation; and 2 = absence of both cold and touch sensations). Motor sensation testing of the tibial and common peroneal nerves was assessed by determining the ability of the patient to plantarflex or dorsiflex the foot (0 = normal, 1 = weak, and 2 = absent).
All patients were subjected to spinal anesthesia using 0.5% hyperbaric bupivacaine (3 ml) with intraoperative local infiltration analgesia (LIA). All surgeries were performed by two surgeons who participated in the clinical study using the minimally invasive mini-midvastus approach. A thigh tourniquet was used in all cases. After implantation of the component and lavage of the surgical site were completed, an LIA cocktail (60 ml; 100 mg of levobupivacaine, 30 mg of ketorolac, 0.3 mg of epinephrine, and 40 ml isotonic sodium chloride solution) was injected around the prosthesis, avoiding the posterior capsule.
After the operation was completed, all patients received a continuous adductor canal block using an in-plane approach, with the needle tip placed inferior to the sartorius muscle and superior to the femoral artery. Levobupivacaine (15 ml; 0.25%) was then injected with intermittent negative aspiration and 0.15% levobupivacaine continuously dripped (5 ml/h) via a catheter with a disposable infusion pump (COOPDECH syrinjector, Daiken Medical, Japan) for 60 hours.
All patients received postoperative paracetamol (650 mg) orally every 6 hours, and celecoxib and pregabalin (400 mg CelebrexⓇ and 75 mg LyricaⓇ, respectively) orally once daily for two days. Patients were also administered 2 mg of intravenous morphine every 2 hours if they reported pain at a numeric rating scale (NRS) score of ≥ 5 for the first 48 hours, postoperatively. When severe pain did not improve, intravenous fentanyl (25 μg every 15 minutes) was administered until patients reported pain at < 4 on the NRS.
The outcomes measured after treatment included the incidence of posterior knee pain, pain score at rest and during movement, findings of the assessment of motor and sensory functions of the tibial and common peroneal nerves after full recovery from the effect of spinal anesthesia, and intravenous morphine consumption during the first 12, 24, and 48 postoperative hours. Tibial and common peroneal nerve sensorimotor function was reported in the evening on postoperative days (POD) 0, 1 and 2, or until function was equal to that of the non-operative leg. Tibial and common peroneal muscle strength was measured by a digital dynamometer (MicroFET2TM, Hoggan Health Industries, USA) pre-operatively and daily until POD 2. All outcomes were measured by anesthesiology and orthopedic residents, who were blinded to the procedures performed on each patient. All data were analyzed using Statistical Package for the Social Science for Windows (version 22.0; SPSS, USA). Descriptive statistics were represented with mean ± standard deviation (SD) for continuous variables and proportions for nominal variables.
In total, the popliteal fossa was dissected in 12 male and 18 female cadavers (average age = 79 ± 7 years) and the location of the ABTN was identified in all cadavers. We found that the tibial nerve gave off articular branches to the posterior capsule of the knee at the level of the popliteal fossa and in the subgluteal region in 29 cadavers and one cadaver, respectively.
In 29 cadavers, the tibial nerve ran superficially and laterally with respect to the popliteal vessels at the proximal portion of the popliteal fossa, and gave off articular branches (1–3 filaments, average = 1) originating 0.5 to 16 cm (5.9 ± 4 cm) above the knee joint line (Fig. 1A). At the distal portion of the popliteal fossa (3 ± 0.28 cm below the origin of the gastrocnemius and plantaris muscles), the tibial nerve ran most superficially and very close to the popliteal vasculature (Fig. 1B). The articular branches ran laterally and entwined with the popliteal vessels forming a plexus. Some filaments of this plexus then entered the adventitia of the popliteal vessels, and distributed towards the posterior capsule of the knee below the medial side of the upper edge of lateral femoral condyle (Fig. 1C). We also found that the posterior capsule was located very superficially and close to the popliteal plexus and skin at this level. The muscular branch of the tibial nerve ran directly through both heads of the gastrocnemius and plantaris muscles.
In one cadaver, the tibial nerve gave off an articular branch in the upper thigh (subgluteal region), and then continued into the knee joint between the popliteal vasculature and the posterior capsule of the knee at the same level as that of other cadavers (Fig. 1D). Therefore, we chose the tibial nerve, popliteal vessels, posterior capsule, femoral condyle, and surrounding muscle as anatomical landmarks for our ultrasound-guided iPACK.
To identify the sciatic nerve and the popliteal artery and vein, the ultrasound probe was placed transversely across the upper level of the popliteal fossa. The angle of the probe was adjusted until clear visualization of the nerve was obtained. The semimembranosus, semitendinosus (both located medially), and biceps femoris (located laterally) muscles were seen on either side of the nerve (Figs. 2A and 2D).
The probe was kept at this initial angle and moved slowly in the caudal direction until bifurcation of the sciatic nerve was seen (Figs. 2B and 2E). The probe was further moved caudally to follow this bifurcation (located superficial and lateral to the popliteal artery) until the common peroneal nerve was completely separated from the tibial nerve, and the semimembranosus, semitendinosus, and biceps femoris muscles were no longer visible (Figs. 2C and 2F).
The ultrasound probe was then moved in a caudal direction until the tibial nerve, which was located just above or superficial to the popliteal vessels, and the two heads of the gastrocnemius muscle were visualized (Figs. 3A and 3C). The femoral condyle and posterior capsule of the knee were clearly identified at this level, where we created two points for needle injection. The first point was located at the lateral border of the popliteal artery, and the second was between the popliteal artery and femoral condyle (Figs. 3B and 3D).
Identification of the correct injection position for modified iPACK using ultrasound guidance (including localization of the tibial nerve, popliteal artery, gastrocnemius muscle, and femoral condyle) was achieved in all 10 cadavers. After dye injection and dissection, traces of dye were observed in the ABTN and popliteal plexus in the distal part of the popliteal fossa. The tibial nerve was stained with a mild amount of dye, but it did not spread to the common peroneal nerve in any of the 10 cadavers (Fig. 4).
This study included 15 patients. Patient demographic data are summarized in Table 1. Modified iPACK using ultrasound guidance was successful, and spread of local anesthesia to the tibial nerve was not observed in any cases. No patient developed posterior knee pain on POD 0. Minimal pain ratings both at rest and during movement are reported in Table 2. One patient required administration of intravenous morphine (2 mg) during the first 12 postoperative hours, whereas the others (14/15) did not need intravenous morphine for postoperative pain relief.
None of the 15 patients experienced complete motor and sensory blocks of the tibial and common peroneal nerves within 30 minutes following the nerve block procedure. On POD 0, two patients (13.3%) developed partially decreased sensory and motor function of the tibial nerve. With respect to the common peroneal nerve, four patients (26.7%) showed partially decreased sensory function on POD 0, but motor function was intact in all cases. Only one patient presented decreased sensation at the tip of the greater toe, which lasted until POD 1. The results for tibial and common peroneal muscle strength are shown in Table 2.
In our cadaveric study, we investigated the pathway of the ABTN after it diverges from the main tibial nerve to form a plexus around the popliteal vessels in the popliteal fossa. Our results were consistent with a previous study described by Horner and Dellon [9] in 1994; however, no prior studies have extensively characterized the pathway of the ABTN before it enters the knee joint. Our study clearly demonstrates that this branch directly contributes to the popliteal plexus and posterior capsule of the knee below the origin of the gastrocnemius and plantaris muscles (approximately 3 cm). Furthermore, this branch is situated close to the joint line at the distal aspect of the popliteal fossa, where the tibial nerve is located closely, superficially, and corresponds to the position of the popliteal vessels, making it an ideal anatomical landmark for ultrasound-assisted anesthetic procedures.
Several studies have adopted the term ‘genicular nerve’ for the sensory innervation of the knee, due to its corresponding genicular artery [14–17]. Previous studies have reported that the tibial nerve also gives off the superior medial genicular or inferior medial genicular nerves to supply the medial aspect of the knee joint [16–18]. However, this term fails to differentiate between the capsular and cutaneous innervations of the knee joint [18–20]. Moreover, one literature quotes that the tibial nerve runs superficial to the popliteal vessels and crosses over to the medial side of the popliteal artery at the level of the knee [21]. Our study found that the tibial nerve gives rise to only posterior articular branches composed of 1–3 filaments. These filaments directly contribute to the posterior capsule and supply the posterior aspect of the knee joint, after running lateral to the popliteal vasculature to form a plexus with some filaments that enter the adventitia of the popliteal vessels. Based on these findings, we believe that the tibial nerve does not give off a branch to supply the medial aspect of the knee joint, but only emits branches to supply the posterior aspect of the knee joint and surrounding muscles.
Several studies have described that the posterior branch of the obturator nerve innervates the posterior aspect of the knee joint together with the ABTN [22,23]. However, this finding was not replicated in our study, and the absence of the obturator nerve within the popliteal fossa was noted in other studies too [17,20,24]. Since our needle injection point is relatively close to the popliteal plexus and the posterior capsule of the knee joint, the local anesthetic could spread and involve the terminal part of the posterior branch of the obturator nerve, which anastomoses with the same branch of the tibial nerve and forms the popliteal plexus.
Recently, there has been increasing interest in developing novel techniques for local anesthetic administration in combination with systemic analgesia to preserve muscle strength following TKA. Several previous studies suggested that LIA, PPBs, and iPACK (also known as the ‘sensory posterior articular nerves of the knee block’) could bring about adequate posterior knee analgesia while sparing motor function, when used as part of multimodal analgesic regimens [10–13,25,26] .
Due to its simplicity and practicality, many studies have found that LIA is beneficial for posterior knee pain following TKA when combined with ACBs, especially during the first 24 postoperative hours [25,26]. This technique can be performed under direct vision by the orthopedic surgeon during surgery; however, it remains a blind technique and has many potential complications, including transient foot drop from common peroneal nerve infiltration (when injected into posterior capsule during the procedure) and increased risk of joint infection [3]. A recent study described the blockade of the popliteal plexus by injecting local anesthesia in the distal part of the adductor canal, from which the drug spread via the adductor hiatus to the popliteal fossa and plexus [13]. When combined with spinal anesthesia and a femoral triangle block, this technique could relieve postoperative posterior knee pain after TKA without ankle motor sensation blockade. However, as previously suggested, it would more accurately be described as a distal adductor canal block, based on the needle injection point [27,28].
The recent advent of an ultrasound-guided iPACK has shown to induce analgesia in the posterior part of the knee by targeting only terminal branches of the tibial nerve and other contributing branches from the popliteal plexus, without affecting the tibial or common peroneal nerves [10–12]. Use of the needle injection point is more accurate and safer than the LIA technique because the needle tip can be visualized on an ultrasound monitor. These iPACK studies primarily indicated that the location of the needle injection point should be in the area between the popliteal artery and posterior capsule, and at the level of the femoral shaft adjoining the femoral condyle. However, some authors still consider the optimal level of injection in this technique to be 1–2 fingers’ breadth above the patella (i.e., the femoral shaft level) or the femoral condyle level. Only one anatomical study evaluated the distribution of the injectate after iPACK. It revealed that 30% of cadaver knees showed spread of injectate to the tibial and common peroneal nerve when iPACK was performed at the level of the posterior femoral shaft and superior to the upper part of the femoral condyle, despite no evidence of spread to the main trunk of the sciatic nerve [29]. However, our study showed no incidences of injectate spread to the common peroneal nerve and minimal spread to the tibial nerve. Notably, excellent pain relief without complete tibial and common peroneal motor blockade was observed in all patients in the clinical study described here. Furthermore, our technique was easy to perform because the site of injection was more superficial, such that the needle tip can be clearly visualized under ultrasound guidance. Therefore, this study suggested that the level below the upper edge of the lateral femoral condyle, in the area of the tibial nerve immediately superficial to the popliteal vessel could be the optimal level to perform ultrasound-guided iPACK (i.e., distal approach iPACK). Further clinical studies are needed to compare the analgesic efficacy and motor-sparing effect between proximal and distal approaches of ultrasound-guided iPACK after TKA.
Despite the obvious advantages of our modified iPACK technique, this study had some limitations that require further investigation. Firstly, post-mortem changes for embalmed cadavers (including the absence of muscle tone and body temperature) might alter the spread of the injectate as compared to that in living patients. Secondly, a control group was not included in the clinical study. Hence, future studies are required for comparison between the efficacy of this method and other regional analgesic techniques for providing postoperative pain relief after TKA.
This study demonstrated that our modified iPACK technique of injecting at the level of the ABTN that formed the popliteal plexus is a feasible and reliable method for treating postoperative knee pain after TKA. The relationship between the course of the tibial nerve and the popliteal vessels can be used to facilitate successful needle positioning for iPACK. Moreover, our study also confirms that iPACK can serve as an improved anesthetic regimen for enhancing recovery after TKA.
Acknowledgments
The authors wish to thank Dr. Chananya Hokierti for figure preparation for this study. We also wish to thank the individuals who donated their bodies and tissue for the advancement of education and research.
NOTES
Author Contributions
Wirinaree Kampitak (Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Validation; Writing–original draft; Writing–review & editing)
Tanvaa Tansatit (Formal analysis; Investigation; Methodology)
Aree Tanavalee (Data curation; Investigation)
Srihatach Ngarmukos (Investigation)
Fig. 1.
Illustrations of anatomical dissection delineating the trajectory of the tibial nerve and its branches in the popliteal fossa (A) the course of the tibial nerve and the articular branch after branching off from the tibial nerve, (B) the tibial nerve runs superficially and closely to the popliteal vasculature in the distal part of the popliteal fossa, (C) the articular branch runs outside and laterally, and entwines with the popliteal vessels forming the popliteal plexus, (D) the articular branch is given off from the tibial nerve in the upper thigh in 1 cadaver. ABFM: biceps femoris muscle, CPN: common peroneal nerve, TN: tibial nerve, PA: popliteal artery, ABTN: articular branch of tibial nerve, GNM: two head of gastrocnemius muscle, MBTN: muscular branch of tibial nerve, Lat: lateral, Med: medial.

Fig. 2.
Illustrations of ultrasound probe positioning and ultrasound views of the interspace between popliteal artery and posterior capsule of the knee (iPACK) at the level of the ABTN, forming a popliteal plexus (A, D) the sciatic nerve is located superficial and lateral to the popliteal vessels in the popliteal fossa, (B, E) bifurcation of the sciatic nerve in the upper part of the popliteal fossa, (C, F) the common peroneal nerve completely separates from the tibial nerve in the distal part of the popliteal fossa. ABTN: articular branch of the tibial nerve, SN: sciatic nerve, STM: semitendinosus muscle, TN: tibial nerve, BFM: biceps femoris muscle, CPN: common peroneal nerve, GNM: two heads of gastrocnemius muscle, SMM: semimembranosus muscle, PA: popliteal artery, FS: femoral shaft, PV: popliteal vein, FC: femoral condyle, Med: medial, Lat: lateral.
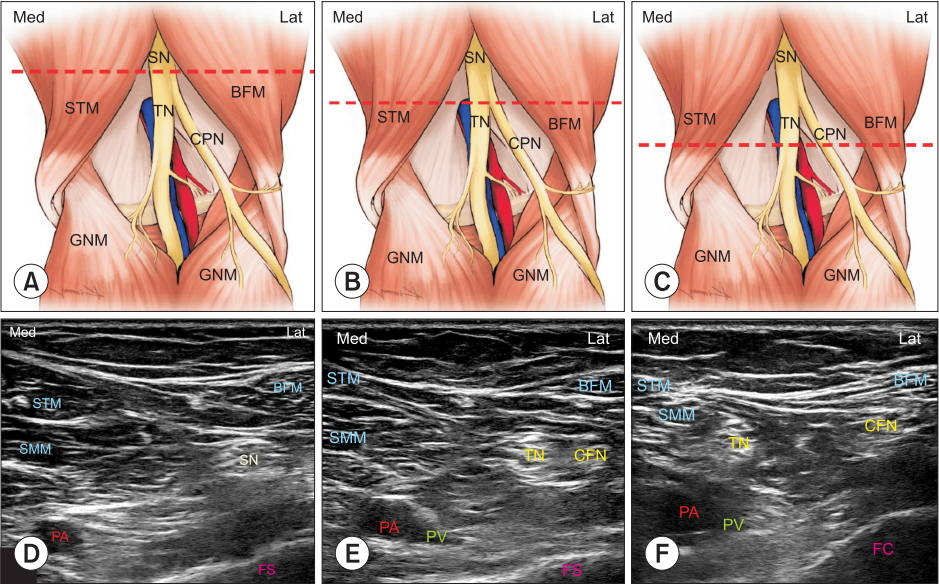
Fig. 3.
Illustrations of ultrasound probe positioning and ultrasound views of the interspace between popliteal artery and posterior capsule of the knee (iPACK) at the level of the articular branch of the tibial nerve forming the popliteal plexus (continued) (A, C) the tibial nerve is located just above, superficially, and close to the popliteal vessels in the distal part of the popliteal fossa, (B, D) the first (purple arrow) and second injection (orange arrow) points for ultrasound-guided iPACK. SN: sciatic nerve, BFM: biceps femoris muscle, STM: semitendinosus muscle, TN: tibial nerve, CPN: common peroneal nerve, GNM: two heads of gastrocnemius muscle, PV: popliteal vein, PA: popliteal artery, PC: posterior capsule, FC: Femoral condyle, Med: Medial, Lat: lateral.
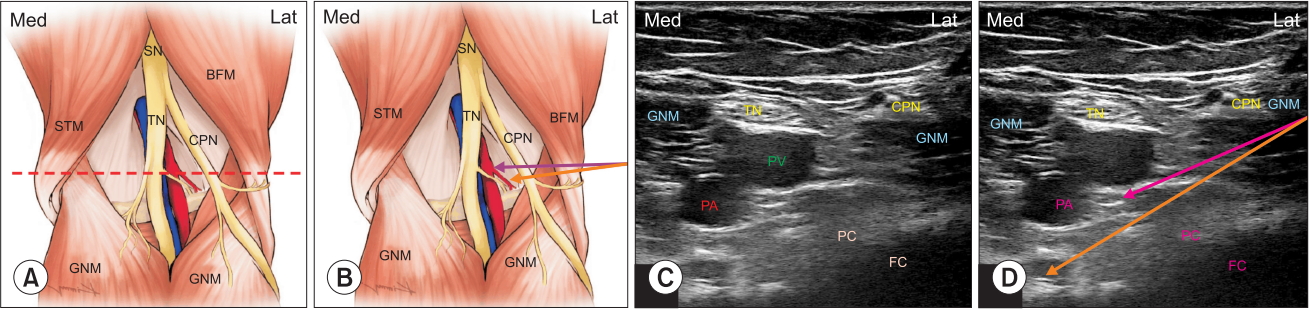
Fig. 4.
Spread of methylene blue dye injected into the popliteal fossa after ultrasound-guided injection in interspace between popliteal artery and posterior capsule of the knee (iPACK). MBTN: muscular branch of tibial nerve, ABTN: articular branch of tibial nerve, TN: tibial nerve, PV: popliteal vessel, GNM: two heads of gastrocnemius muscle, Lat: lateral, Med: medial.
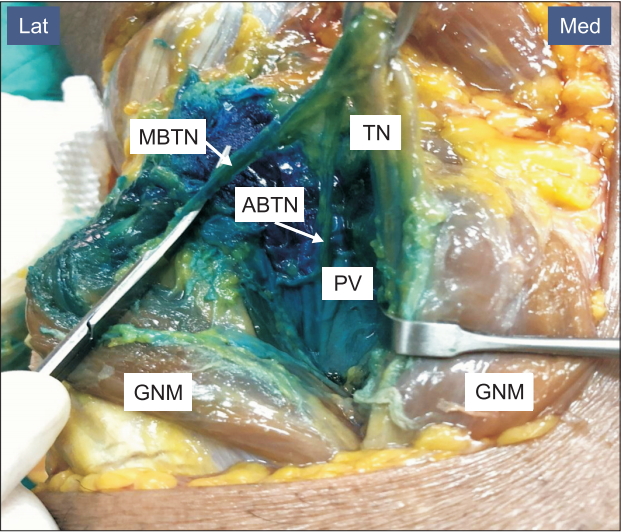
Table 1.
Patient Characteristics
Values are presented as mean ± SD and frequency (n). ACB: adductor canal block, iPACK: interspace between the popliteal artery and posterior capsule of the knee, ASA: American Society of Anesthesiologists Classification (I = A normal healthy patient, II = A patient with mild systemic disease, III = A patient with severe systemic disease).
Table 2.
Patient Outcomes Following Total Knee Replacement (n = 15)
References
1. Husted H. Fast-track hip and knee arthroplasty: clinical and organizational aspects. Acta Orthop Suppl 2012; 83: 1-39.

2. Kehlet H, Thienpont E. Fast-track knee arthroplasty -- status and future challenges. Knee 2013; 20 Suppl 1: S29-33.


3. Terkawi AS, Mavridis D, Sessler DI, Nunemaker MS, Doais KS, Terkawi RS, et al. Pain management modalities after total knee arthroplasty: a network meta-analysis of 170 randomized controlled trials. Anesthesiology 2017; 126: 923-37.


4. Sharma S, Iorio R, Specht LM, Davies-Lepie S, Healy WL. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res 2010; 468: 135-40.


5. Seo JH, Seo SS, Kim DH, Park BY, Park CH, Kim OG. Does combination therapy of popliteal sciatic nerve block and adductor canal block effectively control early postoperative pain after total knee arthroplasty? Knee Surg Relat Res 2017; 29: 276-81.




6. Sinha SK, Abrams JH, Arumugam S, D'Alessio J, Freitas DG, Barnett JT, et al. Femoral nerve block with selective tibial nerve block provides effective analgesia without foot drop after total knee arthroplasty: a prospective, randomized, observer-blinded study. Anesth Analg 2012; 115: 202-6.


7. Silverman ER, Vydyanathan A, Gritsenko K, Shaparin N, Singh N, Downie SA, et al. The anatomic relationship of the tibial nerve to the common peroneal nerve in the popliteal fossa: implications for selective tibial nerve block in total knee arthroplasty. Pain Res Manag 2017; 2017: 7250181.




8. Kampitak W, Tanavalee A, Ngarmukos S, Amarase C. Opioid-sparing analgesia and enhanced recovery after total knee arthroplasty using combined triple nerve blocks with local infiltration analgesia. J Arthroplasty 2019; 34: 295-302.


9. Horner G, Dellon AL. Innervation of the human knee joint and implications for surgery. Clin Orthop Relat Res 1994; (301): 221-6.

10. Kim DH, Beathe JC, Lin Y, YaDeau JT, Maalouf DB, Goytizolo E, et al. Addition of infiltration between the popliteal artery and the capsule of the posterior knee and adductor canal block to periarticular injection enhances postoperative pain control in total knee arthroplasty: a randomized controlled trial. Anesth Analg 2019; 129: 526-35.


11. Thobhani S, Scalercio L, Elliott CE, Nossaman BD, Thomas LC, Yuratich D, et al. Novel regional techniques for total knee arthroplasty promote reduced hospital length of stay: an analysis of 106 patients. Ochsner J 2017; 17: 233-8.


12. Kardash KJ, Noel GP. The SPANK block: a selective sensory, single-injection solution for posterior pain after total knee arthroplasty. Reg Anesth Pain Med 2016; 41: 118-9.


13. Runge C, Bjørn S, Jensen JM, Nielsen ND, Vase M, Holm C, et al. The analgesic effect of a popliteal plexus blockade after total knee arthroplasty: a feasibility study. Acta Anaesthesiol Scand 2018; 62: 1127-32.

15. Choi WJ, Hwang SJ, Song JG, Leem JG, Kang YU, Park PH, et al. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain 2011; 152: 481-7.


16. Yasar E, Kesikburun S, Güzelküçük Ü, Yazar F, Tan AK. Accuracy of ultrasound-guided genicular nerve block: a cadaveric study. Pain Physician 2015; 18: E899-904.

17. Tran J, Peng PW, Lam K, Baig E, Agur AM, Gofeld M. Anatomical study of the innervation of anterior knee joint capsule: implication for image-guided intervention. Reg Anesth Pain Med 2018; 43: 407-14.


18. Hirasawa Y, Okajima S, Ohta M, Tokioka T. Nerve distribution to the human knee joint: anatomical and immunohistochemical study. Int Orthop 2000; 24: 1-4.




20. Orduña Valls JM, Vallejo R, López Pais P, Soto E, Torres Rodríguez D, Cedeño DL, et al. Anatomic and ultrasonographic evaluation of the knee sensory innervation: a cadaveric study to determine anatomic targets in the treatment of chronic knee pain. Reg Anesth Pain Med 2017; 42: 90-8.


21. Apaydin N, Bozkurt M. Surgical exposures for nerves of the lower limb. In: Nerves and Nerve Injuries. Edited by Tubbs RS Rizk E Shoja MM Loukas M Barbaro N Spinner RJ:Cambridge, Academic Press. 2015, pp 139-53.
22. Franco CD, Buvanendran A, Petersohn JD, Menzies RD, Menzies LP. Innervation of the anterior capsule of the human knee: implications for radiofrequency ablation. Reg Anesth Pain Med 2015; 40: 363-8.


23. Runge C, Moriggl B, Børglum J, Bendtsen TF. The spread of ultrasound-guided injectate from the adductor canal to the genicular branch of the posterior obturator nerve and the popliteal plexus: a cadaveric study. Reg Anesth Pain Med 2017; 42: 725-30.


24. Burckett-St Laurant D, Peng P, Girón Arango L, Niazi AU, Chan VW, Agur A, et al. The nerves of the adductor canal and the innervation of the knee: an anatomic study. Reg Anesth Pain Med 2016; 41: 321-7.


25. Hu B, Lin T, Yan SG, Tong SL, Yu JH, Xu JJ, et al. Local infiltration analgesia versus regional blockade for postoperative analgesia in total knee arthroplasty: a meta-analysis of randomized controlled trials. Pain Physician 2016; 19: 205-14.


26. Berninger MT, Friederichs J, Leidinger W, Augat P, Bühren V, Fulghum C, et al. Effect of local infiltration analgesia, peripheral nerve blocks, general and spinal anesthesia on early functional recovery and pain control in unicompartmental knee arthroplasty. BMC Musculoskelet Disord 2018; 19: 249.



27. Morozumi K, Takahashi H, Suzuki T. Distal adductor canal block for administering postoperative analgesia in lower limb surgery. J Clin Anesth 2018; 44: 44.











