|
 |
|
|
Abstract
Background
Laparoscopic cholecystectomy (LC) has traditionally been performed under general anesthesia, however, owing in part to the advancement of surgical and anesthetic techniques, many laparoscopic cholecystectomies have been successfully performed under the spinal anesthetic technique. We hoped to determine the feasibility of segmental epidural anesthesia for LC.
Methods
Twelve American Society of Anesthesiologists class I or II patients received an epidural block for LC. The level of epidural block and the satisfaction score of patients and the surgeon were checked to evaluate the efficacy of epidural block for LC.
Laparoscopic cholecystectomy (LC) with pneumoperitoneum has traditionally been performed under general anesthesia, however, owing in part to the advancement of surgical and anesthetic techniques, many LC have been successfully performed under the spinal anesthetic techniques [1-3]. Generally, spinal anesthesia has lower postoperative mortality and fewer complications than general anesthesia, so spinal anesthesia seems more suitable for the minimally invasive laparoscopic surgery [4].
Although further evaluation and comparison will be required, segmental thoracic epidural anesthesia in LC offers some benefits over lumbar spinal anesthesia: the avoidance of urinary retention and the benefit of a daytime surgery setting [5]. In addition, the level of anesthesia achieved by a spinal anaesthetic is too low to perform laparoscopic surgery in some cases, due to pooling of drug in the sacral region by lumbar lordosis [6]. In addition, the diversity of cerebrospinal fluid volume in each patient makes the anesthetic level unpredictable and a block level above T4 achieved by spinal anesthesia, which is desirable for LC, may cause significant cardiac depression. In epidural anesthesia, the titration of block level is easier, and therefore epidural anesthesia may be preferable in patients with medical conditions such as cardiac disease and obstructive airway disease which depend on active expiration for maintaining lung ventilation, where a slower onset of sympathetic block and minimized muscle weakness are desirable.
We hoped to determine the feasibility of a segmental epidural anesthesia for LC.
After obtaining approval from our institutional research committee and informed consent from each patient, we studied 12 American Society of Anesthesiologists (ASA) physical status I or II adult patients with normal coagulation profile scheduled to undergo laparoscopic cholecystectomy. The patients were informed about the risk of conversion to general anesthesia and similarly the surgeons were prepared to ask for general anesthesia. Surgical inclusion criteria for epidural anesthesia were as follows: a risk score for conversion from LC to open cholecystectomy (RSCO) of less than negative 3 (Table 1) [3]; and the presence of gallstone disease. RSCO is developed by Kama et al. [7] and decides on the likelihood of conversion to open cholecystectomy. The patients with scores less than negative 3 can be predicted to undergo successful LC. On the patient's arrival at the operating room, noninvasive monitoring (electrocardiogram, noninvasive BP monitoring, and pulse oximetry), and a peripheral venous infusion were started before anesthesia. A nasogastric tube was not inserted. Oxygen 5 L/min was applied via a facial mask and end-tidal carbon dioxide monitoring was started.
Patients were placed at the right lateral position and, under full aseptic precautions, an epidural block catheter (Perifix┬«, B. Braun, Melsungen, Germany) was placed at the 10th thoracic interspace using a 17 gauge Tuohy needle and a midline approach. In cases where the 10th interspace was not easily palpated, the block was performed at another interspace. The epidural space was identified by the 'loss of resistance' technique and the tip of the catheter was advanced 3 cm cephalad beyond the tip of needle. The anesthetic solution was prepared with 18 ml of lidocaine 2%, plus epinephrine (1 : 200,000) plus 2 ml of sodium bicarbonate 8.4%. After negative aspiration, 3 ml of the solution was administered as a test dose. If after 2 minutes there was no evidence of intravascular or subarachnoid injection, an additional 7 ml was injected over a 1.5 minute period with fentanyl 50 ┬Ąg, and an additional 2 ml of the solution was administered incrementally to reach the desired level of segmental block. Upper and lower levels of sensory and motor block were assessed by a pinprick test and the Bromage scale respectively, and recorded every 5 minutes until the start of surgery, and every 15 minutes postoperatively. Intraoperative anxiety was treated with midazolam 1-2 mg, abdominal or referred shoulder pain with incremental fentanyl 1-2 ┬Ąg/kg, and hypotension with ephedrine 5-10 mg, all as I.V. boluses as required. During and after the procedure, any discomfort in the patient were recorded (for example: pain, nausea, or itching).
Surgery was performed by the same surgical team, beginning with the placement of three trocars (10 mm just below the umbilicus, 10 mm below the xyphoid, and 5 mm below the costal margin at the midclavicular line). Once the anesthetic block was considered adequate, surgery commenced. Pneumoperitoneum was estabilished with CO2 at a maximum intraabdominal pressure of 10 mmHg instead of the usual 15 mmHg. Another modification of the technique was minimal, if any, tilting of the operating table to the left, with the head up, order to minimize diaphragmatic irritation. No patient had nasogastric drainage perioperatively.
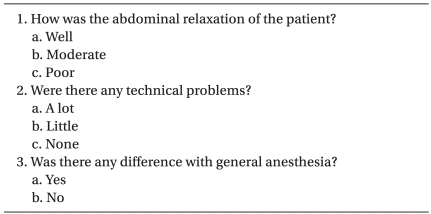
Simplified questionnaire forms were developed for patients and the surgeon to evaluate comments about the operation (Table 2 and 3) [3]. The patients were asked to complete the questionnaire on the first postoperative day. Visual analog scale (VAS) for pain was also checked on postoperative day 1. The surgeon completed the questionnaire forms immediately after the operation.
Our study included 12 patients, 6 women and 6 men, all with gallstone disease and one of them with acute cholecystitis. Demographic data and clinical characteristics of patients are shown in Table 4. The patient with acute cholecystitis was included in this study after discussion with the surgeon, despite his RSCO score being 15, because his inflammation was considered to be mild according to physical examination and laboratory results. The mean age was 54.7 years (range, 27-75 years). 4 patients had concomitant systemic diseases: all 4 had hypertension and 2 had diabetes. One patient had asthma. In this study, the initial trial point of epidural block was the lower thoracic intervertebral space (T10-T11 or T11-T12), however 3 patients received the block in the lumbar area. In 2 patients, there were technical difficulties, and one patient had a mild inflammatory skin lesion in the thoracic area.
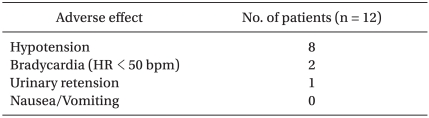
The operation was completed laparoscopically and there was no need for open surgery. Hypotension was observed in 8 patients during surgery. These patients were treated successfully with intravenous ephedrine. Significant bradycardia, with a heart rate below 50 bpm, occurred in 2 patients who required an injection of atropine sulfate. Eleven patients experienced right shoulder pain and 6 patients needed an intravenous fentanyl injection at a dosage of 50 ┬Ąg due to severe pain. Five patients still had shoulder pain and needed an additional intravenous fentanyl injection to control the pain. One of these 5 patients, whose RSCO score was 15 due to acute cholecystitis, needed conversion to general anesthesia due to uncontrolled pain.
One patient complained of dyspnea after insufflation of CO2 gas at the peritoneum and needed assisted mask ventiltation temporarily. Adverse effects observed during surgery are shown in Table 5.
The average total operation time was 38.3 minutes (range, 30-55 minutes) and total anesthesia time was 62.1 minutes (range, 55-90 minutes).
All patients could ambulate the 6 hours after operation, and there were no complications or morbidity in the postoperative period, except in one case with urinary retention that was resolved within 4 hours.
In the questionnaire given on postoperative day 1, 10 patients responded positively to the question about the comfort of the operation and answered this question as "well" or "very well." With the exception of the 2 patients, one with general anesthesia and the other with assisted mask ventilation, the patients were satisfied with the procedure and would recommend this technique to their friends. The average patient's satisfaction score assessed at 2 hours after the operation was 7.6 (range, 3-9) and the average pain score checked at 4 hours after operation was 2.3 (range, 1-3). All surgeons agreed that there were no problems with relaxation of musculature, or the surgical technique, and answered that there was no difference between the technique and general anesthesia.
In our study, 12 patients were included for LC under epidural anesthesia. Eleven patients experienced shoulder pain and 6 of them needed a pain killer. Conversion to general anesthesia occurred in 1 case due to intractable shoulder pain. Hypotension was observed in 8 patients.
Regional anesthesia for LC is considered to have some advantages compared with general anesthesia. Patients can be awake and oriented at the end of the surgery and have less postoperative pain, nausea and vomiting. Problems related to general anesthesia such as oral and teeth injury during laryngoscopy, and a sore throat and stomach inflation as a result of mask ventilation might be avoided in a regional anesthetic setting [8].
In our study, we chose the epidural anesthesia as the anesthetic technique for LC. To complete LC successfully, neuraxial blockade must be performed to cover T4-5 level. Lal et al. [9] demonstrated a significant association between sensory block at the T6 level or higher and the success of the procedure with the patient under epidural anesthesia. Thoracic epidural anesthesia was performed first but another site was chosen in case of failure of the second trial. Three patients received the block in the lumbar area and these cases were possible because LC is not a day-surgery in this center, and the purpose of this study was the applicability of epidural anesthesia to LC.
One of the intraoperative events was a decrease of in the mean arterial pressure. This is a well known adverse effect of spinal and epidural anesthesia covering the thoracic dermatome level, and is easily controlled with ephedrine administration.
Referred shoulder pain due to diaphragmatic irritation from carbon dioxide pneumoperitoneum was also a significant intraopertive event. Most patients experienced right shoulder pain or discomfort and 6 patients needed treatment. One of them received general anesthesia consequently. Incidence of shoulder pain in our study was higher than in the previous reports. According to the report by Sinha et al. [10], shoulder pain occurred in 12.29% of patients. Pursnani et al. [11] noted that shoulder pain occurred in 2 of their 6 patients operated on under epidural anesthesia, and was easily manageable with reassurance, no medical treatment, or simple analgesics. Tzovaras et al. [12] noted that 43% of 50 patients who reveived the spinal anesthesia experienced some degree of shoulder pain, however less than half of those patients required treatment. However, in the series of Hamad and El-Khattary [4], 10 LC were done under spinal anesthesia and 1 patient had to be given general anesthesia due to intolerable shoulder pain.
The higher incidence of shoulder pain in this study might result from the surgical manipulation in part, even after sufficient discussion with the surgical team. This was the first attempt in our hospital of 12 cases of LC under regional anesthesia. The absence of a nasogastric tube could be one of the reasons for a high incidence of shoulder pain. As mentioned in previous studies, using nitrous oxide [8], gentle surgical manipulation [4], nasogastric tube insertion for gastric decompression [1], irrigation of the right diaphragm with 2% lidocaine solution [3], and phrenic nerve block and addition of nonsteroidal anti-inflamatory drugs [13,14] might be helpful for shoulder pain.
One patient required general anesthesia. His RSCO was 15 due to acute cholecysitis and abdominal tenderness, but inflammation was minimal, so it was unlikely that there would be a conversion to open cholecystectomy. After surgery started, he experienced right shoulder pain which did not subside with intravenous analgesic injection, and he was converted from epidural to general anesthesia. Surgery was completed laparoscopically, and there were no difficulties in the surgery, however surgical manipulation was greater than in other simple gallbladder (GB) stone patients. As a result, underlying inflammation around the GB, however mild, might provoke diaphragmatic irritation more intensely during the surgical procedure, which might influence the severe shoulder pain.
The other intraoperative problem encountered was respiratory difficulty, in one of our study cases. A 75-year-old female patient without an underlying disease, whose RSCO was -15, complained of dyspnea after peritoneal CO2 gas insufflation. Her epidural block level was T3 just before starting surgery, but an acute rising of block level to T1 was checked after pneumoperitoneum. Hypotension was also observed which was easy to control with administration of intravenous ephedrine. The patient increased her tidal volume rather than respiratory rate as educated, but because of persistent dyspnea due to the high level of anesthesia, she underwent the operation under assisted mask ventilation with oxygen. Arterial blood gas analysis was not carried out. The patient's dyspnea might be due to increased intra-abdominal, pressure although the interval between epidural block and the beginning the of operation was more than 20 minutes. We think further study to investigate the optimal safe interval to fix the level of epidural block in LC is needed.
Concerning the status of respiratory parameters during regional anesthesia, the observations are not uniform and conflicting reports are present. Chiu et al. [15] reported significant arterial blood gas alteration during epidural anesthesia. Ciofolo et al. [16] noted that PaCO2 was maintained within the normal range through increased minute ventilation during LC under regional anesthesia, and epidural anesthesia for a laparoscopy doses not cause ventilatory depression. Ventilation had to be increased by an average of 30% during cholecystectomy with spontaneous breathing under epidural anesthesia, and intermittent positive pressure ventilation for maintenance of normocarbia is essential to minimize the incidence of arrhythmias [9]. In our case with assisted mask ventilation, the patient might have had some respiratory muscle paralysis due to a high sensory block level. Therefore, active assisted ventilation was needed because an increase in spontaneous ventilation was not expected in the patient, and cardiac depression caused by sympathetic block and respiratory acidemia might result in arrhythmia. Anesthesiologist must keep in mind that respiratory problems can occur.
Postoperative nausea and vomiting, which are common after general anesthesia, were also not seen in our patients. In other series where LC was applied under spinal anesthesia, nausea and vomiting were not common [4,5]. Postoperative urinary retention developed in 1 patient, who was one of 3 patients who underwent lumbar epidural anesthesia. This is known to be related to regional anesthesia with rates of up to 20% in some series [17].
One of the most important problems of LC under regional anesthesia is inadequate relaxation of abdominal musculature [3]. This problem result in difficulties in performing the operation. In our study, the surgeon who performed LC under epidural anesthesia was asked about this problem. He stated that there was no difficulty related to the technique, and relaxation was enough to perform the operation.
This study has limitations in patient selection. Patients whose RSCO was lower than negative 3 and ASA classification was grade 1 or 2 were selected for this procedure. Patients with comorbid diseases may have benefitted more from the regional technique [8]. These patients have a high risk of morbidity for general anesthesia but the usefulness of epidural anesthesia in these patients was not systematically evaluated in this study. Clinically, many patients of LC have combined cholecystitis, but these patients were excluded in our study except in one case. The feasibility of epidural block in these cases were not fully evaluated.
In conclusion, this study has provided preliminary evidence that epidural anesthesia can be effective for LC in treating gall stones. However, unlike other studies that stated that shoulder pain was easily treatable, in our study, shoulder pain was a major problem that could not be ignored and sometimes was not easily manageable. Patients with unbearable shoulder pain needed several fentanyl injections. Careful observation and consideration of other methods such as using nitrous oxide instead of CO2, diaphragmatic irrigation with local anesthetics, and less surgical manipulation to reduce pain are needed for successful LC under regional anesthesia.
References
1. Tzovaras G, Fafoulakis F, Pratsas K, Georgopoulou S, Stamatiou G, Hatzitheofilou C. Laparoscopic cholecystectomy under spinal anesthesia: a pilot study. Surg Endosc 2006; 20: 580-582. PMID: 16437265.


2. van Zundert AA, Stultiens G, Jakimowicz JJ, Peek D, van der Ham WG, Korsten HH, et al. Laparoscopic cholecystectomy under segmental thoracic spinal anaesthesia: a feasibility study. Br J Anaesth 2007; 98: 682-686. PMID: 17371777.



3. Yuksek YN, Akat AZ, Gozalan U, Daglar G, Pala Y, Canturk M, et al. Laparoscopic cholecystectomy under spinal anesthesia. Am J Surg 2008; 195: 533-536. PMID: 18304510.


4. Hamad MA, El-Khattary OA. Laparoscopic cholecystectomy under spinal anesthesia with nitrous oxide pneumoperitoneum: a feasibility study. Surg Endosc 2003; 17: 1426-1428. PMID: 12802665.


5. Tzovaras G, Pratsas K, Georgopoulou S. Laparoscopic cholecystectomy using spinal anaesthesia. Br J Anaesth 2007; 99: 744.author reply 745. PMID: 17933801.


6. Kim JT, Shim JK, Kim SH, Jung CW, Bahk JH. Trendelenburg position with hip flexion as a rescue strategy to increase spinal anaesthetic level after spinal block. Br J Anaesth 2007; 98: 396-400. PMID: 17283005.



7. Kama NA, Kologlu M, Doganay M, Reis E, Atli M, Dolapci M. A risk score for conversion from laparoscopic to open cholecystectomy. Am J Surg 2001; 181: 520-525. PMID: 11513777.


8. Sinha R, Gurwara AK, Gupta SC. Laparoscopic surgery using spinal anesthesia. JSLS 2008; 12: 133-138. PMID: 18435884.


9. Lal P, Philips P, Saxena KN, Kajla RK, Chander J, Ramteke VK. Laparoscopic total extraperitoneal (TEP) inguinal hernia repair under epidural anesthesia: a detailed evaluation. Surg Endosc 2007; 21: 595-601. PMID: 17180283.


10. Sinha R, Gurwara AK, Gupta SC. Laparoscopic cholecystectomy under spinal anesthesia: a study of 3,492 patients. J Laparoendosc Adv Surg Tech A 2009; 19: 323-327. PMID: 19522659.


11. Pursnani KG, Bazza Y, Calleja M, Mughal MM. Laparoscopic cholecystectomy under epidural anesthesia in patients with chronic respiratory disease. Surg Endosc 1998; 12: 1082-1084. PMID: 9685547.


12. Tzovaras G, Fafoulakis F, Pratsas K, Georgopoulou S, Stamatiou G, Hatzitheofilou C. Spinal vs general anesthesia for laparoscopic cholecystectomy: interim analysis of a controlled randomized trial. Arch Surg 2008; 143: 497-501. PMID: 18490561.


13. Scawn ND, Pennefather SH, Soorae A, Wang JY, Russell GN. Ipsilateral shoulder pain after thoracotomy with epidural analgesia: the influence of phrenic nerve infiltration with lidocaine. Anesth Analg 2001; 93: 260-264. PMID: 11473840.


14. Wills VL, Hunt DR. Pain after laparoscopic cholecystectomy. Br J Surg 2000; 87: 273-284. PMID: 10718794.


15. Chiu AW, Huang WJ, Chen KK, Chang LS. Laparoscopic ligation of bilateral spermatic varices under epidural anesthesia. Urol Int 1996; 57: 80-84. PMID: 8873362.


16. Ciofolo MJ, Clergue F, Seebacher J, Lefebvre G, Viars P. Ventilatory effects of laparoscopy under epidural anesthesia. Anesth Analg 1990; 70: 357-361. PMID: 2138437.


17. Jensen P, Mikkelsen T, Kehlet H. Postherniorrhaphy urinary retention: effect of local, regional, and general anesthesia: a review. Reg Anesth Pain Med 2002; 27: 612-617. PMID: 12430114.


Table┬Ā4
Demographic and Clinical Characteristics of 12 Patients with Epidural Anesthesia
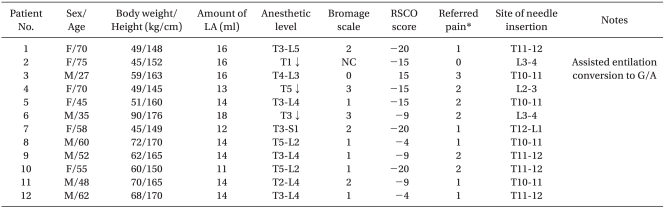
Bromage scale, 0: able to lift extended leg, 1: just able to flex knees, full ankle movement, 2: no knee movement, some ankle movement, 3: complete paralysis. Anesthetic sensory level and Bromage scale were checked 30 minutes after epidural injection by pinprick test. LA: local anesthetic solution injected to epidural space (all solution included with fentanyl 50 ┬Ąg), RSCO: risk score for conversion from laparoscopic cholecystectomy to open cholecystectomy, NC: not checked, F: female, M: male, G/A: genaral anesthesia. *Grade of referred pain, 0: none, 1: mild, no additional analgesics needed, 2: moderate, additional analgesics needed, 3: severe, not controlled by analgesics.
- TOOLS